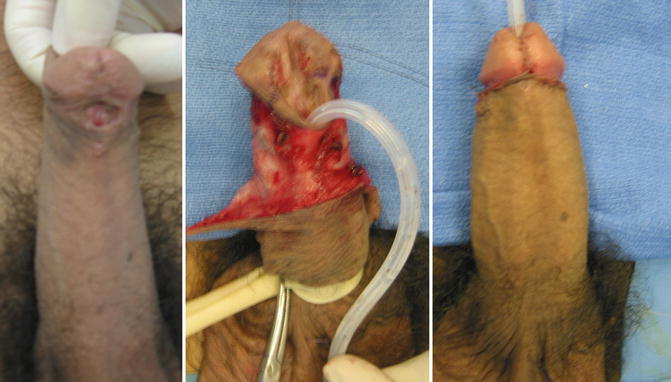
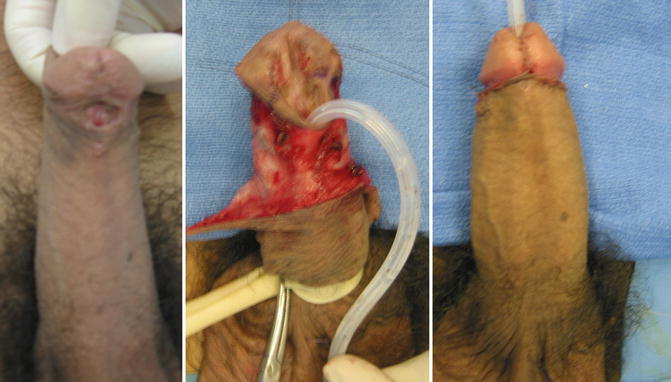
Fig. 8.1
Doral Heinke-Miculikz meatoplasty and Thiersch-Duplay repair for sub-coronal stenotic meatus and deep glans sulcus
Li et al’s [6] experience with the repair of hypospadias using a bladder mucosal tube in 113 adolescents and adults is remarkable. The ages ranged from 13 to 29 years (mean age was 17.1 years). There were 31 primary cases in which adequate foreskin was lacking and 82 secondary cases. The meatus was penile in 33, penoscrotal in 72, and perineal in 8. All of the repairs except one (primary or secondary) were performed as one-stage procedure. They achieved satisfactory cosmetic and functional results in 99 patients (87.6 %). Others have not replicated the success of bladder mucosal tubes, and this technique has been largely abandoned.
Secondary Hypospadias Repairs (Table 8.1)
Table 8.1
Primary and secondary hypospadias repair in adult and adolescent patients: review of the literature
Patients (number) | Average age (years) | Follow-up | Primary repair (number) | Secondary repair (number) | Type of repair | Presenting complaint | Staged or single stage | Outcome (success rate) | Complications | |
|---|---|---|---|---|---|---|---|---|---|---|
Li et al. [6] | 113 | 17.1 (13– 29) | 3 months to 2 years | 31 | 82 | Tubularized bladder mucosa | Hypospadiac meatus | Single Stage | 87.6 % | – UCF 7.1 % – Urethral stricture 5.3 % |
Hensle et al. [5] | 42 | 22.5 (18– 47) | 1– 19 years | 8 | 34 | – Primary: Thiersch-Duplay, Mathieu, Island pedicle tube graft – Secondary: Fistula closure, Mathieu, Island pedicle tube graft, buccal mucosa tube graft, Island pedicle onlay graft, bladder mucosa tube graft, buccal mucosal onlay graft, split thickness skin graft | – Hypospadias meatus – Chordee – UCF – Scarring – Hair bearing urethra – Urethral stones – Diverticulum | Single | – 62.5 % in primary stage repairs – 44.1 % in secondary stage (36.3 % in “cripples”) – Outcomes increased to 100 % primary repair after secondary surgery and 85.3 % in secondary surgery | – UCF 10 – Stricture 6 – Graft loss 2 – Graft contracture 2 – Skin flap loss 2 |
Senkul et al. [3] | 88 | 21.9 (20– 27) | 28 months (5– 60 months) | 59 | 29 | – Primary: MAGPI, Mathieu, TIP, Asopa, Duckett, two stage, buccal tube – Secondary: fistula, Mathieu, TIP, in situ tubularization, buccal tube, and onlay | – Primary: hypospadiac meatus – Secondary: UCF, hypospadiac meatus, cripple | Both (only 2 staged) | – 89.9 % in primary – 72.5 % in secondary – After secondary interventions increased to 100 % and 89.6 % | – Primary: fistula, partial graft loss – Secondary: fistula, partial graft loss, total graft loss, stricture |
Snodgrass et al. [33] | 25 | 18 (16 months– – 40 years) | 5 months (6 weeks– 14 months) | 25 | Bracka two-stage repair with buccal mucosa | Scarred urethral plate and residual hypospadias | Staged | 65 % (in 20 patients) | UCF, glans dehiscence | |
Amukele et al. [7] | 126 | 14 months–35 years | 12 months | 126 | Free skin, bladder and buccal grafts, Thiersch-Duplay | Hypospadias cripples, chordee | Single Both | 74 % 79 % | Multiple UCF, stricture, skin tethering, breakdown, inclusion cyst | |
Dodson et al. [34] | 31 | 13 (10–62) | 14 months (1–288) | 31 | n/a | Metal-based flaps, MAGPI, island onlay flaps, staged procedure, TIP, tube graft, Mathieu | Hypospadiac meatus | Both | 52 % | UCF, stricture, hematoma, loss of repair, urethral web |
Sharma [35] | 13 | 18–26 | 0.5 years (0.25–3) | 13 | n/a | TIP urethroplasty | Hypospadiac meatus | Single | 76.9 % | UCF (closed spontaneously) |
Hatipoglu et al. [36] | 27 | 22 | 13 months (6–18) | 27 | n/a | TIP urethroplasty | Hypospadiac meatus | Single | 81.4 % | Meatal stenosis (successfully dilated in all) and UCF (closed at 6 months) |
Adayener and Akyol [4] | 97 | 21.8 (20–26) | 19 months (6–31) | 80 | 17 | MAGPI, Mathieu, TIP urethroplasty | Hypospadiac meatus | Single | – Primary 76.5 % (increased 100 % secondary procedure – Secondary 91.3 % (increased 100 % in secondary procedure) | – Primary: UCF, skin flap loss – Secondary: UCF and flap loss |
Barbagli et al. [37] | 60 | 32.2 (19–37) | 33.8 months (12–138) | n/a | 60 | Meatoplasty, anastomotic repair, fistula closure, dorsal inlay graft or flap with skin, buccal mucosa inlay and onlay, multistage with skin, multistage with buccal mucosa | Urethral stricture, residual hypospadias, UCF, meatal stenosis, penile curvature, hair, diverticular, stone | Both | 75 % (different success based on one stage vs. multi stage and source of graft) | UCF, meatal stenosis, glans dehiscence, poor cosmesis, residual chordee |
Barbagli et al. [38] | 1,176 | 31 years (1–76) | 60.4 months (12–137) | 1,176 | n/a | Meatoplasty, UCF closure, end-to-end anastomosis, perineal urethrostomy, buccal mucosa, skin graft or flap, Johanson, glans reconstruction, penile skin reconstruction, corporoplasty | Urethral stricture, residual hypospadias, UCF< meatal stenosis, residual curvature, hair, diverticula, stones | Both | 88.1 % | Types of complications not reported |
Schwentner et al. [39] | 31 | 13.5 (15 m–26 years) | 78.45 months (61– 116 months) | n/a | 31 | Single stage full thickness genital skin grafts | UCF, urethral stricture, residual hypospadias, diverticula or breakdown and all patients had a scarred urethral plate requiring graft | Single | 87.1 % | Urethral stricture and fistula |
Lumen et al. [40] | 25 | 36.2 (19–55) | 45.4 months (4–92) | n/a | 25 | Free grafts, anastomotic repair, combined urethroplasty, pedicled flap, and staged repair | Urethral stricture | Both | 72 % (fistula was not considered failure and not reported as failures) | – Recurrence of stricture – 4 patients with fistula, not reported as part of complications |
Meeks et al. [41] | 15 | 30.5 (18–57) | 23 months (5–62) | n/a | 15 | Staged repair with grafts including buccal mucosa, auricular, abdominal skin, and penile skin | Lower urinary tract symptoms, infertility, chordee, fistula, hair, stone, and recurrent infections | Staged | 86 % | Dehiscence, breakdown, fistula, poor cosmesis, coronal meatus, spraying, retention, buccal mucosa oral graft complications, UTI |
Myers et al. [42] | 50 | 38 (19–71) | 89 months (median, range 6– 198) | n/a | 50 | Penile skin flap, perineal urethrostomy, excision and primary anastomosis, tubularized plate, buccal mucosa onlay, UCF closure, chordee correction, combined | Urethral stricture, fistula, persistent hypospadias, hair in the urethra and chordee | Both | 76 % (50 % initially) | Urethral stricture, UCF, periurethral infection, graft contracture, erosion |
Cambareri and Hanna [39] | 29 | 10–29 | 2 years in all (14 patients had follow-up 5 years) | n/a | 29 | Island skin flap onlay or buccal mucosal graft onlay | Urethral stricture in all, UCF, chordee | Single | 86.2 % (increased to 93.1 % with secondary procedures) | UCF and recurrence of stricture |
Our approach for creating a neourethra in redo and complex hypospadias repair has evolved over three decades. We now have an experience with 203 hypospadias cripples who had had 2–23 surgical procedures prior to referral, 126 of whom were previously reported [7]. Early on we used tubed free skin grafts, then tubed bladder mucosa grafts, and later on buccal mucosal grafts and have incorporated any residual urethral plate if it appears healthy no matter how narrow it was. When we reviewed our complication rate for the tubed free skin grafts in 2005, it was 32 %, but rose to 54.5 % by 2010 as more of these grafts developed lichen sclerosis. Our experience with bladder mucosa is that it tends to proliferate in the presence of irritating factors. Accordingly, the most common complication involving all bladder mucosa substitution urethroplasties involves meatal stenosis. When the bladder mucosa is exposed to air, it becomes sticky, friable, and hypertrophic leading to meatal stenosis. Although this can be prevented by anastomosing a 1 cm full thickness skin graft to the distal end of the mucosal tube, the potential morbidity of the end-to-end anastomosis of two free grafts and the sclerosis of the skin tube makes this proposition unappealing. Furthermore, the pliability of bladder mucosa also leads to ballooning during voiding and over time diverticulum formation. We have reported 27 bladder mucosal tubed grafts in complex hypospadias cases [7] and encountered 6 major complications (2 strictures, 3 mucosal prolapse, and 1 fistula with mucosal prolapse). There were four patients who developed minor complications (skin tethering in three and inclusion cyst in one). A consistent problem has been exuberant overgrowth of transitional epithelium at the meatus producing a “cauliflower like “appearance. The total of 37 % secondary surgeries following bladder mucosal tube in our patients and the additional surgery for harvesting the graft led us to abandon the bladder mucosa in favor of buccal mucosal grafts, as have others.
The popularization of oral mucosa-free grafts (OMG) in repair of hypospadias cripples has revolutionized treatment for this group [8]. When tissue transfer is needed, OMG is universally accepted as the best free graft due to ease of harvest, quality of substrate for urethral substitution, low late complication rate, and low long-term donor site morbidity [9, 10]. One-stage onlay or two-stage repairs are preferable to one-stage tubed repairs, resulting in lower complications with durable results in peripubertal/postpubertal patients [2, 11–16, 33]. Successful outcomes in postpubertal hypospadias cripples are more difficult to achieve than in a prepubertal population, rendering a need to utilize two-stage approaches for peri- and postpubertal hypospadias cripples [37, 41]. Urinary function, as characterized by AUA-SS, for patients undergoing buccal mucosa graft reconstruction is reasonable, with most patients reporting mild LUTS. Even after successful repair, however, cosmesis continues to be a challenge for this group, with 1/3 of patients undergoing OMG reconstruction stating that they are very or somewhat dissatisfied with the cosmetic outcome [17]. Sexual function in this group of patients has been characterized utilizing the IIEF and demonstrating excellent results. Similar to all hypospadias patients, ejaculatory complaints predominate [17].
Urethral Fistula
Fistula is an ingrowth of epithelial cells along the suture tracts, and when large is a localized tissue necrosis. Small fistulas may present at a later date during adolescence. After ruling out distal obstruction, closure of a simple fistula can be achieved by dissecting out the fistula tract and directly approximating the edges without narrowing the urethral lumen followed by intraoperative testing for water tightness of the closure, waterproofing by a Dartos or tunica vaginalis flap, and coverage with a rotation trapdoor skin flap based on the upstream edge (Fig. 8.2). Complex fistulae including large, multiple, and recurrent may be a manifestation of another problem. Richter et al. [18] reviewed the records of 28 patients, who had had between 2 and 15 attempts at closure where 17 had a single fistula and 11 patients multiple fistulae were present. The causes of failure were believed to be the awkward fistula site in 12 (coronal fistulas), urethral diverticulum in 7, and distal urethral stricture in 4. In 5 patients, the cause of the recurrent fistula was unclear. In these cases, intraoperative calibration of the distal urethra and urethral distension using a syringe full of water and a Christmas tree adapter will demonstrate a stricture or a diverticulum.
Fig. 8.2
Closure of a simple fistula
For larger fistulas where direct closure would narrow the urethral lumen, either a lateral hinge flap or an adjacent skin flap on subcutaneous mesentery (island flap) can be used. If the local skin is scarred, a free-patch graft of buccal mucosa with buttressing by a tunica vaginalis flap would be another surgical option.
Coronal fistulas are notoriously difficult to repair by layered closure because the distal glandular tissue is fixed. This often causes some degree of tension on the suture line, hence the high failure rate of coronal fistula repairs. In our experience, coronal fistulas are best repaired by converting them to coronal hypospadias, by dividing the bridge of tissue between the fistula and meatus. Then, the urethral plate is tubularized using a wider strip (Thiersch-Duplay tube) with or without a dorsal midline relaxing incision depending on how deep the glans sulcus is (Fig. 8.3). In resurfacing the operative site, the traditional transposition flaps (Y-V and advancement) may be unreliable because their vascularity may have been compromised by previous surgery. The hairless midline scrotal island or rotation of a scrotal flap is more reliable for these cases. It should be noted that these are random flaps and a width/length ratio of at least 1:2 should be maintained.
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




