Fig. 8.1
Transcervical tubal cannulation to assess for tubal patency
8.2.3 Distal Tubal Occlusion
If preoperative HSG has confirmed a more distal tubal occlusion, a diagnostic laparoscopy can be the next step for those patients not proceeding directly to IVF. Prior to these procedures patients should be counseled on both salpingostomy and tubal repair as well as salpingectomy, since large hydrosalpinges have been demonstrated to negatively affect IVF success [4]. Patients with the best chance of success for tubal repair are those with small amounts of filmy adhesions and mild dilation of the fallopian tubes (Fig. 8.2).
Salpingolysis and Fimbrioplasty. Once laparoscopic access is established, the fallopian tube is identified. The mesosalpinx can be injected with dilute vasopressin (5 international units per 20 mL of normal saline) to reduce bleeding. The tube is gently elevated with an atraumatic grasper, and adhesions are either lysed or excised using a harmonic scalpel or endoscopic scissors. Avoiding lateral damage may help improve long-term tubal function. Outcomes are best if distal tubal disease is limited to encapsulating adhesions.
A straight dissector can be used to resolve fimbrial agglutination or prefimbrial phimosis. If a small hydrosalpinx is present, an incision is made using a laparoscopic needle or scissors with harmonic, monopolar electrosurgery employed sparingly. This incision allows drainage of the hydrosalpinx fluid.
If the hydrosalpinx is large or the adhesions are extensive, salpingectomy should be undertaken and followed by IVF because a large hydrosalpinx (greater than 3 cm) has a poor response to neosalpingostomy. A blunt probe can be very useful in truly gauging the severity of a hydrosalpinx (Fig. 8.3).



Fig. 8.2
Peritubal adhesions. Intraoperative laparoscopic image of peritubal adhesions (Courtesy of M. Milad)

Fig. 8.3
Utilizing a blunt probe to assess the size of a hydrosalpinx (Courtesy of M. Milad)
Salpingectomy is performed by dividing the proximal tube at the cornua using an electrosurgical coagulation and cutting device. The same device is then used to coagulate and cut the mesosalpinx close to the tube along its length serially. Electrosurgery should be used sparingly, given the concern for thermal injury to the ovarian vessels and the potential for fewer oocytes retrieved at egg aspiration. To avoid any electrosurgery at the infundibulopelvic ligaments, sutures or an endoloop may be employed (Fig. 8.4).


Fig. 8.4
Use of an endoloop to ligate the infundibulopelvic ligament as part of a salpingectomy, enabling minimal use of the electrocautery and maximal sparing of the ovarian blood supply (Courtesy of M. Milad)
Neosalpingostomy. If the fimbria have become severely adhered in such a way that the tubal opening is obliterated and no retention of normal fimbria is seen, a more complex tubal repair may be warranted. After placement of dilute vasopressin and salpingolysis, a stellate or cruciate incision is made at the distal end of the hydrosalpinx using a needle, harmonic shears, or scissors. Electrosurgery should be used sparingly to avoid tubal damage. The distal end “fimbriae” are then everted, and interrupted sutures are placed to maintain the increased size of the opening (see Fig. 8.5a, b). Owing to the technically difficult nature of placing these sutures in friable and delicate tubal tissue, this procedure should only be undertaken by laparoscopic surgeons who are very comfortable with the laparoscopic microsuturing technique and the use of 6–0 suture or finer. Alternatively, desiccation using electrosurgery or laser immediately behind the distal end may help facilitate retention of patency after the stellate or cruciate incision has been made (see Fig. 8.6).
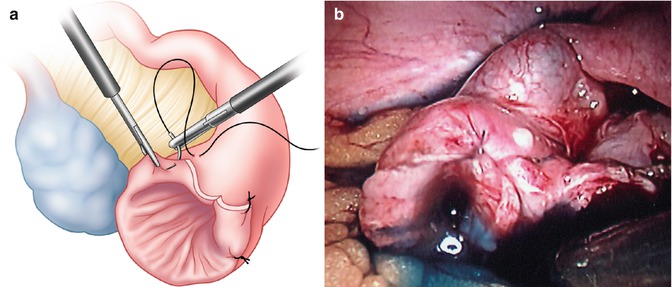
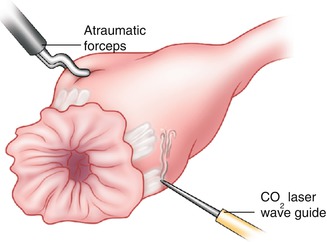
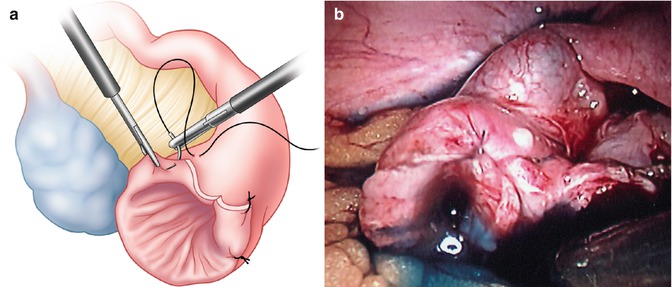
Fig. 8.5
Neosalpingostomy. (a) Line drawing of neosalpingostomy technique illustrating suturing of divided tubal edge to proximal tube to create a new tubal opening. (b) Intraoperative photograph demonstrating the resulting tubal opening after completion of the neosalpingostomy
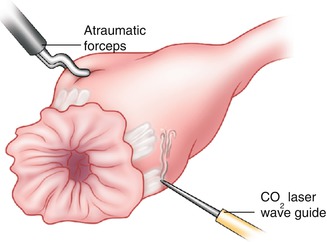
Fig. 8.6
Bruhat technique using carbon dioxide laser just behind the distal tubal edge to attempt to maintain tubal patency after lysis of adhesions of a blocked tubal opening
Success rates for these procedures range widely. Patients with only mild hydrosalpinx have had intrauterine pregnancy rates ranging from 58 to 77 % after the procedure, with an ectopic pregnancy rate of 2–8 % [5].
8.2.4 Reversal of Prior Tubal Ligation
Patients undergoing reversal of prior tubal ligation should be counseled about the alternate option of IVF. Most patients with tubal ligation have excellent IVF cycle specific success rates. If tubal reversal is warranted, it should be undertaken by an expert reproductive surgeon experienced with handling of fine suture and delicate tissue.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








