Name (type)
Point of uterine vessels transection
Amount of vagina removed
Point of uterosacral ligament transection
Simple (I)
At insertion into cervix (level of the internal os)
Minimal
At insertion into cervix
Modified radical (II)
At level of the ureter
1–2 cm
Midway between cervix and rectum
Radical (III)
At their origin from the internal iliac vessels
Upper half
At their origin
Extended radical (IV)
At their origin from the internal iliac vessels
Upper three-fourths with paravaginal tissue
At their origin
Partial exenteration (V)
At their origin and en bloc with ureters (and possibly bladder)
Entire vagina above levator muscles
At their origin (and possibly en bloc with rectum)
Table 6.2
Querleu–Morrow classification of radical hysterectomy
Type | Extent of resection | Ureter | Comment |
|---|---|---|---|
Type A | The paracervix is transected medial to the ureter but lateral to the cervix. | Ureter palpated or directly visualized without freeing from bed | |
Uterosacral and vesicouterine ligaments are not transected at a distance from the uterus | |||
Vaginal resection is minimal without removal of the paracolpos | |||
Type B1 | Paracervix is transected at the level of the ureteral tunnel | Unroofing of ureter | Type B2: Type B1 + removal of the lateral lymph nodes |
Partial resection of ureterosacral and vesicouterine ligaments | Ureter rolled laterally | ||
No resection of caudal (deep) neural component of the paracervix (caudal to the deep uterine vein) | |||
Vaginal resection of at least 10 mm of the vagina from the cervix or tumor | |||
Type C | Transection of paracervix at junction with internal iliac vascular system, uterosacral ligaments at the rectum, and vesicouterine ligaments at the bladder | Ureter completely mobilized | Type C1: with autonomic nerve sparing/preservation |
Resection is 15–20 mm of the vagina from the tumor or cervix and corresponding paracolpos | Type C2: without autonomic nerve sparing/preservation | ||
Type D1 | Resection of the paracervix at the pelvic side with vessels arising from internal iliac system, exposing the roots of the sciatic nerve | Ureter completely mobilized | |
Type D2 | Resection of the paracervix at the pelvic side, with hypogastric vessels plus adjacent fascial or muscular structures (laterally extended endo-pelvic resection) | Ureter completely mobilized |
6.2.2 Procedure
What follows is a description of the Piver-Rutledge-Smith type III radical hysterectomy. Once mastered, this procedure can easily be modified for more (type IV) or less (type II) radical procedures. The order of the steps listed may differ slightly from surgeon to surgeon. Although this surgery can be performed with monopolar electrocautery, we recommend using one of the many advanced vessel sealing devices because they tend to have better hemostasis and, more importantly, less lateral thermal spread. The latter is particularly important when dissecting near the ureter.
The surgery begins with a careful exploration of the entire peritoneal cavity for evidence of intraperitoneal spread. This includes inspection of the upper abdomen and all peritoneal surfaces. For women with cervical cancer, if metastatic disease is encountered, the surgery should be terminated and the patient reassigned to chemotherapy and/or radiation.
The round ligament is then divided and the retroperitoneal space is entered. Gentle blunt dissection in this avascular space is performed, and the external iliac vessels, internal iliac artery, and ureter are identified. A careful examination of the pelvic lymph nodes should be made, and any enlarged or abnormal-appearing nodes should be removed and sent for frozen section evaluation. One of the few limitations of the minimally invasive radical hysterectomy is the decreased tactile sensitivity for palpating lymph node basins.
A bladder flap is then created using a combination of the advanced vessel sealing device and blunt dissection. Early in the surgery only a small bladder flap is necessary. However, throughout the procedure, the surgeon returns to the bladder, further dissecting it from the pubovaginal fascia to achieve the desired vaginal margins.
The pararectal and paravesical spaces are then opened. We favor opening the pararectal space first, although this varies based on the surgeon’s preference. The pararectal space is entered by bluntly dissecting between the ureter and internal iliac artery along the curve of the sacrum. This is another avascular space bordered by the internal iliac artery/levator ani laterally, the rectum medially, the sacrum posteriorly, and the cardinal ligament (parametrium) anteriorly.
Once the pararectal space is opened to the pelvic floor, the paravesical space should be opened. With anterior retraction of the proximal portion of the severed round ligament and using the superior vesicle artery as a landmark, this space can be entered either medially or laterally to that vessel (although we favor lateral entry). Again, blunt dissection is used to open this avascular space bordered by the obturator internus muscle laterally, the bladder medially, the pubis symphysis anteriorly, and the cardinal ligament posteriorly. Care must be taken not to create an inadvertent cystotomy. Historically, after opening these spaces, the surgeon would place one finger in each space, palpating the cardinal ligament to rule out tumor infiltration. With a minimally invasive approach, this is not possible. However, opening these two spaces does help identify the uterine artery and its surrounding parametrial tissue (Fig. 6.1
).
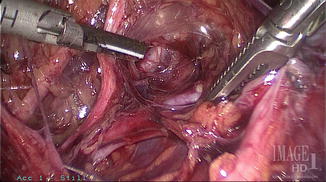
Fig. 6.1
The uterine artery is seen at its origin from the internal iliac (hypogastric) artery
Once identified, the uterine artery is dissected and ligated at its origin using an advanced vessel sealing device. With gentle traction upward, the surrounding parametrial tissue is taken en bloc with the uterine vessels. As the parametrial tissue is freed laterally and deeply, the ureter is tunneled from underneath it as the parametrial tissue is brought up over it (Fig. 6.2
). The tunneling of the ureter continues until its insertion into the bladder is reached. Along the way, the ureter is freed from its medial attachments and “rolled” laterally. When dissecting the deep portion of the parametrium, care must be taken not to disrupt the sympathetic nerve fibers innervating the bladder and rectum.
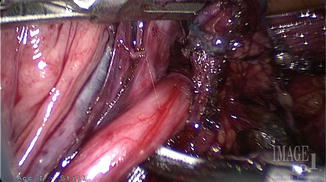
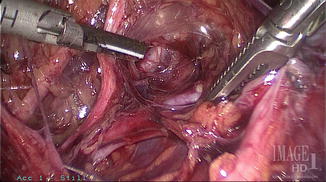
Fig. 6.2
The ureter is untunneled as it courses through the parametrial tissue
The vesicouterine peritoneal fold is now transected using the advanced vessel sealing device. This often requires further mobilization of the bladder downward. Care must be taken not to perform an inadvertent cystotomy during this portion of the procedure. Backfilling the bladder may assist in helping to decide the best surgical plane to take.
The uterus is now anteflexed, and the rectovaginal space is developed. Another avascular space, this can be entered by retracting the sigmoid colon caudally and posteriorly and incising the fold between the bowel and the posterior cervix (Fig. 6.3

). This incision is extended laterally, and the rectovaginal space is developed bluntly. This mobilizes the rectum away from the vagina and exposes the uterosacral ligaments. With good visualization of the lateralized ureters, the uterosacral ligaments can now be transected at their origin using an advanced vessel sealing device (Fig. 6.4

).

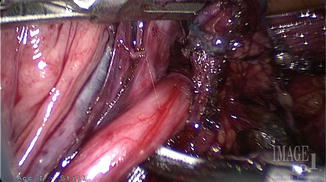
Fig. 6.3
The recotvaginal space is opened, exposing the uterosacral ligaments

Fig. 6.4
The uterosacral ligaments are transected
With the bladder, the vesicouterine fold, the parametrium, and the uterosacral ligaments now freely dissected and the ureters mobilized laterally, a circumferential colpotomy incision can be made, taking care to achieve the desired vaginal margins. The radical hysterectomy specimen is removed through the vagina, and the vaginal cuff is closed either vaginally or laparoscopically based on the preference of the surgeon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








