Adnexa
Retrieval of ovarian tissue for freezing before any type of RT and/or CT in young cancer patients
Ovarian suspension before pelvic radiation for cervical cancer
RRSO
Conservative and not conservative treatment and (re)staging of borderline ovarian tumors
Potential conservative and demolitive treatment and (re)staging of apparently stage 1 ovarian cancer (both epithelial and others)
Uterus
Treatment and staging of early endometrial cancer
Treatment and staging of IB1 small tumor cervical cancer
Staging for conservative treatment in early stage cervical cancer
Retroperitoneal staging in LACC
13.2 Operating Room Organization
A well-organized operating room is a prerequisite not only for the success of the intervention but also to optimize the timing of surgery and to lower related costs. Surgical team position radically changes during LESS surgery compared with standard laparoscopy, because single-site incisions force surgeons to change their position to maximize mobility of the instruments. In this case, the first surgeon, after inserting the port, stands behind the shoulders of the patient, at the level of the head, the place usually occupied by the anesthesia team. The assistant is positioned at the right shoulder of the patient. An appropriate Trendelenburg position is required to decrease the distance between the surgeon and the patient, which is more extreme than in standard laparoscopy. A third surgeon may be placed between the legs of the patient to manipulate the uterus.
13.3 Surgical Technique
Surgical procedures are performed through a single multiport reusable or disposable trocar (LESS) inserted into the umbilicus. We generally use an Olympus multiport trocar (Olympus Winter & IBE GMBH; Hamburg, Germany). This device consists of three components: the introducer, the fixing valve, and the trocar itself. The trocar, made of a doubled-over cylindrical sleeve of pliable film material fixed to the proximal ring, flows down around the distal ring and then back up and out. To introduce the trocar, the distal ring is passed through an open access into the abdominal cavity using the introducer. A 1.5– 2-cm longitudinal transumbilical skin incision is made. The subcutaneous fat is opened, with exposure and incision of the abdominal fasciae for approximately 2 cm. The parietal peritoneum is smoothly dissected with blunt scissors, achieving access into the peritoneal cavity. After the skin incision is made, the distal ring is mounted on an introducer, an instrument used to insert and push the distal ring through the abdominal wall. Then the introducer is removed, the retractable sleeve is gripped to the proximal end, and the outer ring is pushed down to create a perfect seal with the abdominal wall. The excess sleeve is finally cut off. Through the adjustable length of the sheath, the outer part of the trocar can be positioned in contact with the skin regardless of the thickness of the abdominal wall or body mass index of the patient, making it comfortable even in obese patients. Triport (Olympus Winter & IBE GMBH; Hamburg, Germany) has two channels for the transit of gas and three ports for surgical instruments: two measuring 5 mm and one measuring 12 mm. Although a model with four ports is available, three ports seem sufficient to perform any gynecologic-oncologic procedure. The cannula positions are adjustable within the flexible port, and a separate channel allows for carbon dioxide insufflation. In order to maintain the pneumoperitoneum, the ports are sealed with a gelatinous plastic material, which prevents the escape of gas during surgical maneuvers; this does make it necessary to lubricate the instruments to avoid excessive friction. Once pneumoperitoneum (12 mmHg) is achieved, intra-abdominal visualization is obtained with a 5-mm 30° telescope or, alternatively, a 5-mm 0° laparoscope with a flexible tip (EndoEYE; Olympus Winter & IBE GMBH; Hamburg, Germany) (Fig. 13.1). Straight conventional 5-mm instruments are inserted into the remaining two ports, namely, the surgeon’s choice of graspers, scissors, suction/irrigation, bipolar coagulator, and a multifunctional versatile laparoscopic device that grasps, coagulates, and transects simultaneously. The combination of one standard 33-cm long instrument with a 43-cm long instrument is preferred to prevent excessive contact between the surgeon’s instruments outside the abdominal cavity and to facilitate stripping and traction maneuvers (Fig. 13.2). Changes in the positions of the instruments and camera are performed according to the needs of the surgeon. A steep Trendelenburg position is usually needed to complete the surgery (about 30°). At the end of the procedure, each layer of the access port is separately sutured to prevent subsequent umbilical hernia occurrence. In particular, the abdominal fascia is closed by separate delayed reabsorbable sutures, and the skin is repaired with rapid absorbable suture.



Fig. 13.1
Laparoendoscopic single-site surgery (LESS) for conservative treatment of borderline ovarian tumors: external view (a); internal view (b)

Fig. 13.2
The position of instruments during stripping of an ovarian cyst
The following table describes some of the most common surgical procedures performed in gynecologic oncology (Table 13.2).
Table 13.2
Single port surgical procedures in gynecologic oncology
Intraperitoneal |
Abdominal inspection and washing |
Peritoneal biopsies |
Infra-colic omentectomy |
Appendectomy |
Extrafascial and radical hysterectomy |
Adnexectomy, cystectomy, salpingectomy |
Retroperitoneal |
Pelvic and para-aortic lymphadenectomy |
13.3.1 Risk-Reducing Salpingo-Oophorectomy, Bilateral Salpingo-Oophorectomy for Adnexal Masses, and Ovarian Cancer Staging
An intrauterine device (intrauterine manipulator-Olympus Winter & IBE; Hamburg, Germany) may be used to make surgery easier (i.e., pelvic endometriosis or large adnexal masses). Once pneumoperitoneum is achieved (12 mmHg), intra-abdominal visualization is obtained, and one grasper and one multifunctional versatile laparoscopic device that grasps, coagulates, and transects simultaneously are inserted to perform surgery. However, the use of different surgical instruments does not change the surgical technique. Pelvic washing is performed in all cases. The broad ligament is transected between the ovarian pedicle and the iliac vessels, and the retroperitoneal structures and the ureter are identified. The infundibulopelvic ligament is skeletonized and transected using the 5-mm multifunctional device. The fallopian tube and mesosalpinx are dissected, and the utero-ovarian ligament is transected. The same procedure is repeated on the opposite side. The adnexa are inserted into a 10-mm Endocatch bag (Covidien; Mansfield, MA) and removed through the umbilicus after taking out the single-port device. In the case of large adnexal cysts, they may be emptied within an endobag to avoid spillage.
13.3.2 Simple Extrafascial Hysterectomy and Bilateral Salpingo-Oophorectomy
The patient is placed in the dorsal lithotomy position, and both arms are gently tucked and padded at the patient’s sides. A high-quality uterine manipulator with a colpotomy valve is utilized in order to achieve the necessary counter-traction for LESS hysterectomy cases. It is positioned only after bilateral coagulation of the tubes in order to prevent tumor from spreading into the peritoneal cavity. In our experience, the use of a manipulator is not detrimental to any procedures in terms of increased bleeding or difficulty with pathologic evaluation. This was corroborated by Rakowski and colleagues and Fanfani and colleagues, who demonstrated that minimally invasive radical hysterectomy cases performed with a uterine manipulator did not show any clinical-pathologic differences in depth of invasion, lymphovascular space invasion, or parametrial involvement compared to open cases [8, 9].
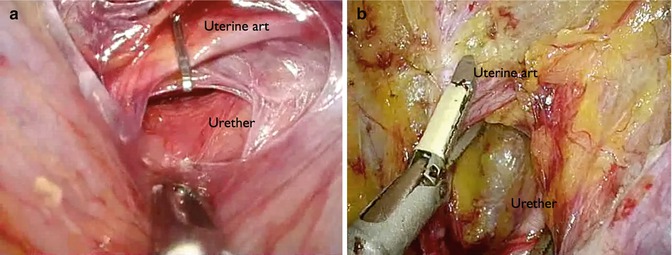
A combination of one straight 33-cm long, 5-mm instrument with one 43-cm long, 5-mm instrument (such as graspers, cold scissors, suction/irrigator) and a 5-mm multifunctional device (that grasps, coagulates, and transects simultaneously) plus a 5-mm flexible-tipped laparoscope are used. After coagulation and section of the round ligament, entry into the retroperitoneal space is performed, and the ureter is visualized. Hemostatic clips or direct coagulation is performed at the origin of the uterine artery (Fig. 13.3a, b) [10]. The infundibulopelvic ligaments are skeletonized and transected. A bladder flap is developed using the multifunctional instrument. An adequate margin of the vagina is ensured before colpotomy, which is performed using a monopolar hook. The uterus, cervix, and bilateral fallopian tubes and ovaries are removed through the vagina, and the vaginal vault may be closed either via the vagina with single stich technique or by a laparoscopic extracorporeal knotting technique. Vascular or visceral injuries, loss of pneumoperitoneum, or intraoperative port-site bleeding are in line with literature data such as wound hematoma, wound infection, or delayed bleeding postoperatively [1–6]. Median operative time reported in the literature is about 100 min (range, 45–155 min) with a median estimated blood loss of 30 mL (range, 10–500 mL) [10]. Most patients report complete satisfaction with cosmetic appearance and postoperative pain control. They are discharged home one day postoperatively with only optional analgesic therapy.