Stool and Fluid Tagging
Judy Yee
Currently patients typically undergo bowel cleansing before computed tomography colonography (CTC). However, investigators have made significant progress in identifying methods to label residual fluid and stool with positive oral contrast agents so that there is easier differentiation from the homogeneous soft tissue density of polyps. This technique has been evaluated both with and without the use of a laxative. However, if the requirement for a cathartic agent could be eliminated or if the amount of cathartic agent needed could be reduced, this would likely lead to improved patient tolerance. This can give CTC a significant advantage over colonoscopy by improving patient compliance with screening for colon cancer. Once residual fluid and stool are tagged with a positive contrast agent, electronic subtraction of the high-density material may then be performed. It has been postulated that electronic subtraction bowel cleansing may eliminate the need for scanning in both supine and prone positions because electronic removal of residual material may be performed with one acquisition. However, dual-position scanning may still be necessary in order to achieve optimal segmental distention.
Tagging of residual material in the colon may be achieved by the ingestion of iodinated contrast material and/or barium. Studies have been performed evaluating the use of iodinated contrast or barium alone as well as in combination and in some of the studies a laxative is administered. Variable results have been achieved depending upon the specific type of contrast and laxative used as well as on the volume of contrast and laxative administered and the timing of when the contrast and laxative are ingested. The employment of dietary modification and hydration before CTC can also impact on the amount of residual stool and fluid as well as the adequacy of tagging.
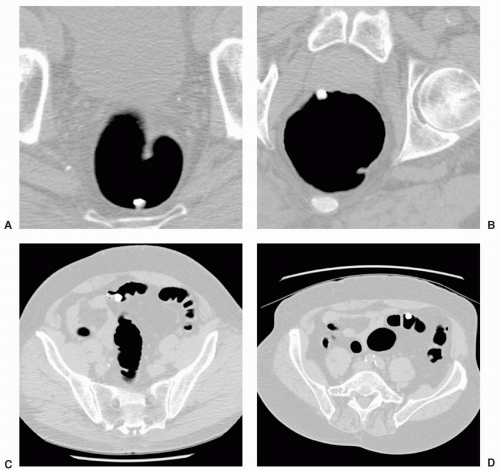
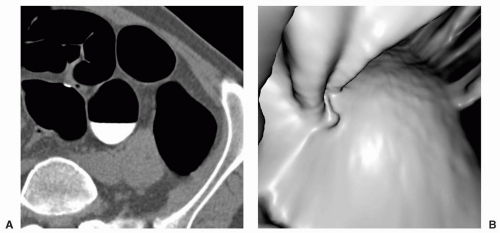
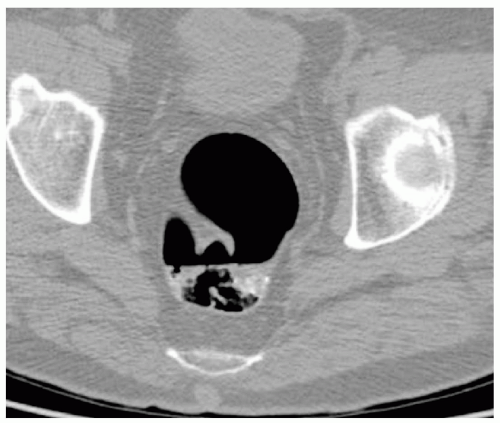
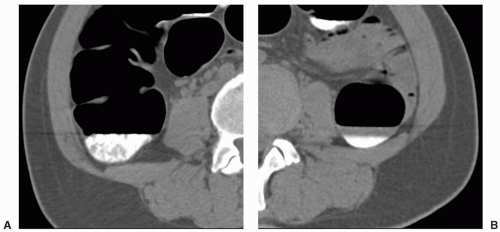
Optimally tagged stool has homogeneous internal high-density, which allows for easy differentiation from the soft tissue density of polyps on two-dimensional (2D) images. Optimally tagged fluid is uniformly high density allowing the detection of polyps submerged in the fluid on 2D images (see Figures 10.1 and 10.2). Homogeneous labeling of material allows for effective subtraction of the tagged material which in turn enables more efficient primary three-dimensional (3D) interpretation. An alternative method that may be employed for distinguishing tagged stool from polyp on 3D images is the use of translucency rendering, which is available using specific software.1 Translucency rendering is a function that combines attenuation-dependent transparency with color mapping. Colors are assigned to maximize the different densities of tagged stool versus polyp. Tagged stool may be assigned a white color whereas soft tissue polyps appear as lesions with gradual density change of blue, green, and red corresponding to regions of increasing attenuation (see Figures 10.3 and 10.4). Using this color scheme, fatty lesions appear green on translucency rendering.
The use of oral contrast material as a tagging agent for CTC may also allow for the identification of polyps with villous histology. O’Connor et al. evaluated 216 patients with 338 polyps in a retrospective study and found that 46% of the 312 polyps not touching a contrast pool had adherent contrast.2 Patients had received 500 mL of 2.1% barium for stool tagging and 120 mL of iodinated contrast material for fluid tagging as well as 90 mL of sodium phosphate and bisacodyl for colonic cleansing. Villous polyps were much more likely to have adherent contrast compared to nonvillous polyps (77% vs. 43%). In this study, villous polyps also tended to be larger on average compared to nonvillous polyps (13.9 mm vs. 7.4 mm). Pedunculated polyps were found to more likely have adherent contrast (68%) compared to sessile (45%) and flat lesions (24%).
Heterogeneous tagging of residual stool and fluid can make it difficult to distinguish polyps from unlabelled stool or fluid (see Figures 10.5 and 10.6). Electronic subtraction of heterogeneously tagged material may result in nondiagnostic images with residual unsubtracted stool confused for polyps (see Figure 10.7). Polyps may also be obscured by poorly tagged material that is not subtracted.
TAGGING WITH LAXATIVE
The labeling of residual colonic fluid with oral iodinated contrast material has been evaluated in patients who have
also received a purgative. There are also several studies evaluating the iodinated contrast as a tagging agent without the use of a laxative and these are presented in the next section. In an earlier study by Fletcher et al., 73 patients underwent bowel cleansing with 4 L of polyethylene glycol (PEG) lavage solution and two 5-mg bisacodyl tablets.3 Patients ingested 120 mL of iodinated contrast material the night before the computed tomography (CT) scan. Results showed that there was no increase in sensitivity or specificity for polyp detection when oral iodinated contrast material was administered. In fact there was a trend for decreased detection of medium-sized polyps (5-9 mm) with the use of oral contrast. An increase in residual fluid attenuation was found in only 48% of patients who received oral iodinated contrast according to the protocol in this study. Thomeer et al. performed a study evaluating 150 patients who received either 3 to 5 L of a home-made electrolyte solution (130 patients) or PEG before thin-slice multidetector computed tomography (MDCT) Colonography (1-mm collimation, 0.8-mm reconstruction interval, 60 effective mAs, 120 kVp).4 Iodinated contrast material was added to the bowel preparation solution (30 mL/L) to tag residual colonic fluid and stool. Bowel cleansing and tagging occurred in the hospital up to 5 hours before the CT scan. In contrast to the results of Fletcher et al., tagging was found to be optimal with homogeneous labeling in 95% of cases and this was felt to be due to the short interval during which the patients had to ingest the iodinated contrast material before the CTC. Sensitivities were 64% to 67% for 5- to 9-mm polyps and 92% for polyps larger than 9 mm. The overall specificity was high at 94% to 95%.
also received a purgative. There are also several studies evaluating the iodinated contrast as a tagging agent without the use of a laxative and these are presented in the next section. In an earlier study by Fletcher et al., 73 patients underwent bowel cleansing with 4 L of polyethylene glycol (PEG) lavage solution and two 5-mg bisacodyl tablets.3 Patients ingested 120 mL of iodinated contrast material the night before the computed tomography (CT) scan. Results showed that there was no increase in sensitivity or specificity for polyp detection when oral iodinated contrast material was administered. In fact there was a trend for decreased detection of medium-sized polyps (5-9 mm) with the use of oral contrast. An increase in residual fluid attenuation was found in only 48% of patients who received oral iodinated contrast according to the protocol in this study. Thomeer et al. performed a study evaluating 150 patients who received either 3 to 5 L of a home-made electrolyte solution (130 patients) or PEG before thin-slice multidetector computed tomography (MDCT) Colonography (1-mm collimation, 0.8-mm reconstruction interval, 60 effective mAs, 120 kVp).4 Iodinated contrast material was added to the bowel preparation solution (30 mL/L) to tag residual colonic fluid and stool. Bowel cleansing and tagging occurred in the hospital up to 5 hours before the CT scan. In contrast to the results of Fletcher et al., tagging was found to be optimal with homogeneous labeling in 95% of cases and this was felt to be due to the short interval during which the patients had to ingest the iodinated contrast material before the CTC. Sensitivities were 64% to 67% for 5- to 9-mm polyps and 92% for polyps larger than 9 mm. The overall specificity was high at 94% to 95%.
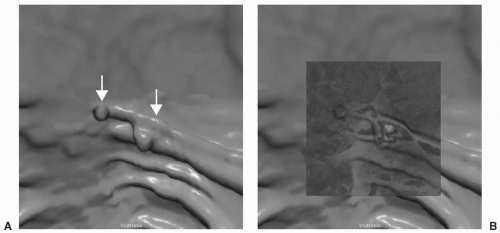 FIGURE 10.3 Polyp and Tagged Stool. 3D endoluminal view (A) shows two polypoid lesions on a fold. When the translucency view is employed (B), the central white core in the larger lesion demonstrates it to be tagged stool. The color pattern of the smaller lesion with gradual change in the colors red, green and blue suggest a polyp. (Views A and B: See also color plate.) |
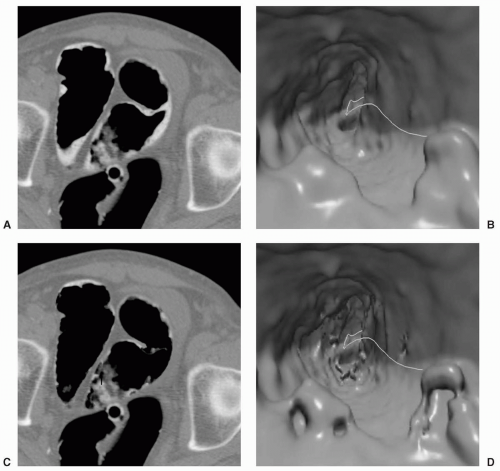
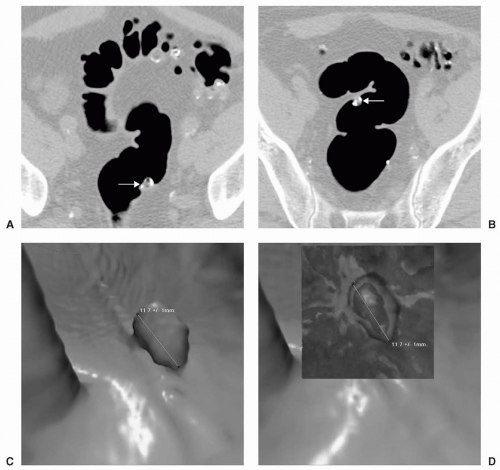 FIGURE 10.4 Heterogeneously Tagged Stool. Axial supine (A) and prone (B) images show mobile heterogeneously tagged stool. The partially tagged stool simulates a polyp on the 3D endoluminal view (C). When the translucency view is applied (D), the color pattern shows white centrally indicating that this lesion is tagged stool. (Views C and D: See also color plate.) |
Barium has been evaluated as an oral agent for stool tagging with the use of a laxative. In an initial study, Lefere et al. compared reduced colonic cleansing based on dietary fecal tagging with standard colonic cleansing.5 Fifty patients underwent a low residue diet starting 2 days before the CT scan including a specific meal kit which was ingested the day before CTC with three separate 250-mL doses of barium (2.1% weight per volume) at each meal. In the early evening on the day before CTC, patients also underwent bowel cleansing with 16.4 g of magnesium citrate and bisacodyl tablets. A bisacodyl suppository was given the morning of the CTC examination. Fifty patients underwent standard colonic cleansing with up to 3 L of PEG the afternoon before the CTC. Results showed that patients undergoing fecal tagging had more residual stool but there was improved specificity of 88% versus 77% in the nonfecal tagging group. Overall per-patient sensitivities between the two groups were similar at 85% (nonfecal tagging) and 88% (fecal tagging). Fecal tagging
was found to significantly reduce discomfort, side effects, and sleep disturbance and produced a better final opinion of how comfortable the examination was and a trend for increased patient willingness to repeat the examination.
was found to significantly reduce discomfort, side effects, and sleep disturbance and produced a better final opinion of how comfortable the examination was and a trend for increased patient willingness to repeat the examination.
Gryspeerdt et al. compared three different colon cleansing techniques which were each used in 20 patients.6




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree