Fig. 15.1
Image of deployed Stone Cone (courtesy of Boston Scientific)
Several studies have examined the efficacy of the Stone Cone® in prevention of stone migration. In the initial clinical experience, the Stone Cone® was used in 23 cases of pneumatic lithotripsy for ureteral stones, compared with 27 control cases in which no migration device was used. When compared with controls, the Stone Cone® reduced the number of clinically significant residual fragments (0% vs. 30%, p < 0.001) as well as the need for secondary procedures (0% vs. 20%, p < 0.01) [23]. A second study compared electrohydraulic lithotripsy of ureteral stones with and without the Stone Cone® and noted significantly increased stone retropulsion (23% vs. 0%, p < 0.01) and significantly increased residual fragments greater than 3 mm in diameter (31% vs. 0%, p < 0.001) in cases without the Stone Cone® compared to those with the Stone Cone® [24].
Two noncontrolled series have been published using the Stone Cone® for ureteroscopic laser lithotripsy, with reported migration rates of 0–1.5%. Maislos et al. demonstrated that 19 consecutive patients with proximal ureteral stones underwent semirigid ureteroscopy with laser lithotripsy using the Stone Cone®. At the conclusion of the procedure, none of the patients had residual stone fragments larger than 2 mm and no auxiliary procedures were required [21]. An additional retrospective series of 133 consecutive cases of ureteroscopy with laser lithotripsy demonstrated a 1.5% incidence of patients requiring an additional procedure to treat migrated stone fragments [25].
NTrap®
The NTrap® is a device with a 3F shaft consisting of a wire mesh net composed of tightly woven Nitinol wires within a 115-cm sheath (Fig. 15.2). The net has central wires 1 mm apart and outer wires 2 mm apart. The original device had a mesh diameter of 8 mm and therefore had the ability to occlude a ureter dilated to that size. Because of the flexibility of its mesh fibers, the device is able to accommodate the ureter easily when it is deployed proximal to the stone. With the ureter occluded, the device can prevent proximal migration of stone fragments as small as 1.5 mm (in fact, fragments smaller than 1 mm are prevented from proximal migration by the central portion of the mesh, and only the peripheral wires allow passage of larger fragments) [9, 12, 26].


Fig. 15.2
Image of deployed NTrap (courtesy of Cook Urological)
Wang et al. recently performed a prospective trial of 113 patients undergoing ureteroscopy with pneumatic lithotripsy for proximal ureteral stones [9]. In half of the patients, the NTrap® was used to prevent stone retropulsion. The authors noted a significantly lower incidence of stone migration in the NTrap® group (0% vs. 12%, p = 0.007) as well as an improved stone-free rate in the NTrap® group (100% vs. 84%, p = 0.002). There was no statistically significant difference in need for additional procedures. A second series compared 76 patients who underwent ureteroscopic lithotripsy (81% with Holmium:YAG, 19% with Wolf pneumatic lithoclast) with the NTrap® with 68 patients who underwent standard ureteroscopy. Stone-free rate was significantly higher in the NTrap® group (98.7% vs. 89.7%, p = 0.019) [26].
Finally, a meta-analysis which includes the two aforementioned articles and a case series, totaling 456 cases noted that NTrap® was associated with a threefold increase in stone-free status, a fivefold reduction in stone retropulsion, and a threefold reduction in the need for auxiliary shock wave lithotripsy (SWL) treatment for migrated fragments [27].
Accordion®
The Accordion® is a sheath-wire system, 150 cm in length and with an outer shaft diameter of 0.038 in (Fig. 15.3). It has a floppy tip and a distal multifold film. When the device is deployed by coaxial retraction of the inner core of the coaxial wire, it “Accordions” to a 7 or 10-mm wide plug that blocks stone migration and provides the utility of a basket during stone fragment removal (Fig. 15.4). Because the Accordion® is the newest FDA-approved anti-retropulsion device, few clinical studies have evaluated its efficacy. In two abstracts published in 2007, the use of the Accordion® was described in seven patients undergoing ureteroscopy and Holmium:YAG lithotripsy for proximal and distal ureteral stones [28, 29]. The device prevented retrograde migration of all stone fragments. Interestingly, the authors also noted rebounding of irrigation fluid off the deployed Accordion®, thus flushing the stone fragments distally and allowing for a clearer view.
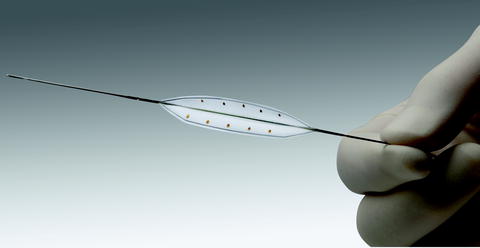

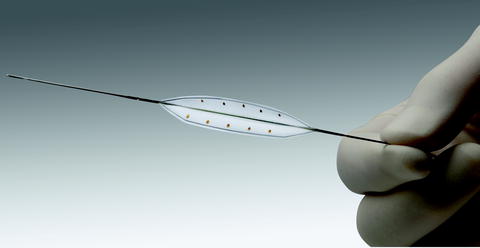
Fig. 15.3
Image of undeployed Accordion (courtesy of PercSys)

Fig. 15.4
Image of deployed Accordion (courtesy of PercSys)
Chemical Antiretropulsion Devices: BackStop® and Others
BackStop® is a unique biocompatible polymer with reverse thermosensitive properties (Fig. 15.5). It exists as a liquid at temperatures below 16 °C and as a soft but injectable gel at room temperature, and then transitions to a viscous gel at body temperature. BackStop® is dispensed with the accessory BackStop® injector and 3 or 5 Fr catheter. Before fragmentation the catheter is positioned 1–2 cm above the stone via the ureteroscope working channel or directly under fluoroscopy. BackStop® is dispensed above the stone, and forms a gel plug that conforms to the ureter and prevents the stone from migrating up the ureter and potentially into the kidney. After stone fragmentation is completed, the BackStop® plug is dissolved using saline irrigation; this process can be facilitated by using cold saline [30, 31].
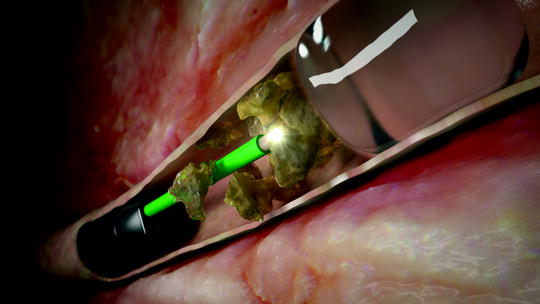
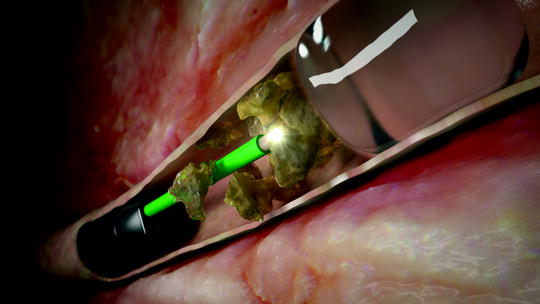
Fig. 15.5
Image of BackStop deployed proximal to ureteral stone (courtesy of Boston Scientific)
In a prospective, randomized trial, 34 patients, who underwent Holmium:YAG or pneumatic ureteroscopic lithotripsy with the BackStop® were compared with 34 patients, who underwent ureteroscopy without any antiretropulsion device. The procedures were performed by different urologists. The rate of stone retropulsion was significantly lower in the BackStop® group (52.9% vs. 8.8%, p = 0.0002). While the rates of ureteral occlusion, auxiliary procedures and adverse events were also lower in the BackStop® group, these differences did not reach statistical significance [30].
In addition to the BackStop®, other viscous materials have been tested to prevent stone retropulsion. In 2004, Ali et al. published a new technique, wherein 1–2 ml of lubricating jelly was injected proximal to a ureteral stone prior to electrokinetic lithotripsy [32]. Among seven patients treated in this manner, stone or fragment retropulsion was observed in none. A subsequent randomized control trial assessed the use of lidocaine jelly to prevent stone migration during pneumatic lithotripsy [33]. A stone retropulsion rate of 4% was observed among patients in whom the jelly was used, while the control group had a 28% rate of retrograde stone migration. Stone-free rates were also significantly different between the two groups (96% vs. 72%, p = 0.045). In 2011, lidocaine jelly was compared with the Stone Cone® for its efficacy in preventing stone migration in a prospective randomized trial with 40 patients [34]. While both methods demonstrated effectiveness, the Stone Cone® was found to be superior to lidocaine jelly in stone retropulsion rates (0% vs. 15%, p < 0.05) and operative time (41.8 vs. 51.4 min, p < 0.05).
Other Issues: Device Deployment, Irrigation Characteristics, Damage, and Cost
In addition to the aforementioned clinical studies on the efficacy of using anti-retropulsion devices, there are number of characteristics common to each, which merit discussion. For any disposable device which is designed to improve outcomes in ureteroscopy, the ease of deployment and potential damage caused by deployment of the device is worth considering. A previously published study examined the dilation of the ureter proximal to obstructing calculi with an eye towards selection of the appropriate anti-retropulsion devices [35]. The authors analyzed 176 obstructing ureteral stones (nearly 1/3 proximal ureteral stones and 2/3 distal ureteral stones) and noted that the degree of dilation of the ureter just proximal to the stone was greater for proximal than for distal calculi, and that in total, 96% of all obstructed ureters could be occluded by a device of 7 or 10 mm diameter, while 4% of ureters demonstrated more dilation than 10 mm [35].
A subsequent study compared the insertion force and maneuverability as well as dilation and extraction forces for the Stone Cone®, Accordion®, and NTrap® in an ex vivo model. This study noted that the Stone Cone® demonstrated significantly higher insertion forces and required more attempts to bypass an experimental impacted stone than the Accordion® or the NTrap®. The Stone Cone® also demonstrated significantly greater radial dilation as well as required force of extraction than the Accordion® and the NTrap®. It remains to be seen how these differences observed in the laboratory setting may translate to differences in the clinical use of the devices [36]. In a related abstract, the pull-through forces of the Accordion®, Stone Cone®, and NTrap® devices were compared in a simulated ureter model and the Accordion® was found to have the lowest pull-through force [37].
The response of the Stone Cone®, NTrap®, and Accordion® to laser damage has also been tested in a laboratory model. Of note, the Accordion® was the most laser resistant device, able to be operated (i.e., deployed and un-deployed) after 100 direct contacts of the Holmium laser on the Accordion® film. The Stone Cone® was less laser resistant than the Accordion® but more resistant than the NTrap®. In a second experiment which tested the carrying catheters of the devices, the Stone Cone® and NTrap® catheters were more laser resistant than that of the Accordion® [22].
One study hypothesized that use of anti-retropulsion devices may decrease pressure transmitted to the upper tracts by decreasing the amount of irrigant which flows cephalad of the device. Using an ex vivo model, this report noted that the Accordion®, NTrap®, and Stone Cone® all significantly decreased renal pelvic pressures when compared to no device, and among them, the Accordion® demonstrated the greatest reduction [38].
A final issue to consider is the cost of the device. As mentioned briefly already anti-retropulsion devices have the potential to reduce costs by decreasing operative times, reducing the need to change from the semirigid to flexible ureteroscopy to chase migrated fragments cephalad, and also by preventing auxiliary procedures to treat clinically significant retropulsed fragments [8, 23, 39]. These cost benefits must be weighed, however, against the cost of the device. A single study examined the cost-effectiveness of use of the Accordion® to prevent stone retropulsion during pneumatic lithotripsy for ureteral stones. Using a decision analysis model which included the cost of additional ureteroscopy or shock wave lithotripsy for a clinically significant migrated stone fragment during the initial ureteroscopy, the authors noted that at a retropulsion rate of 14%, the device was cost-effective to use. It is noteworthy that this analysis model was strictly financial, and did not take into account other potential benefits, such as the potential for decreased operative times or decreased numbers of procedures for an individual [40] (Table 15.1).
Table 15.1




Published studies comparing ureteroscopic lithotripsy with and without anti-migration devices
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







