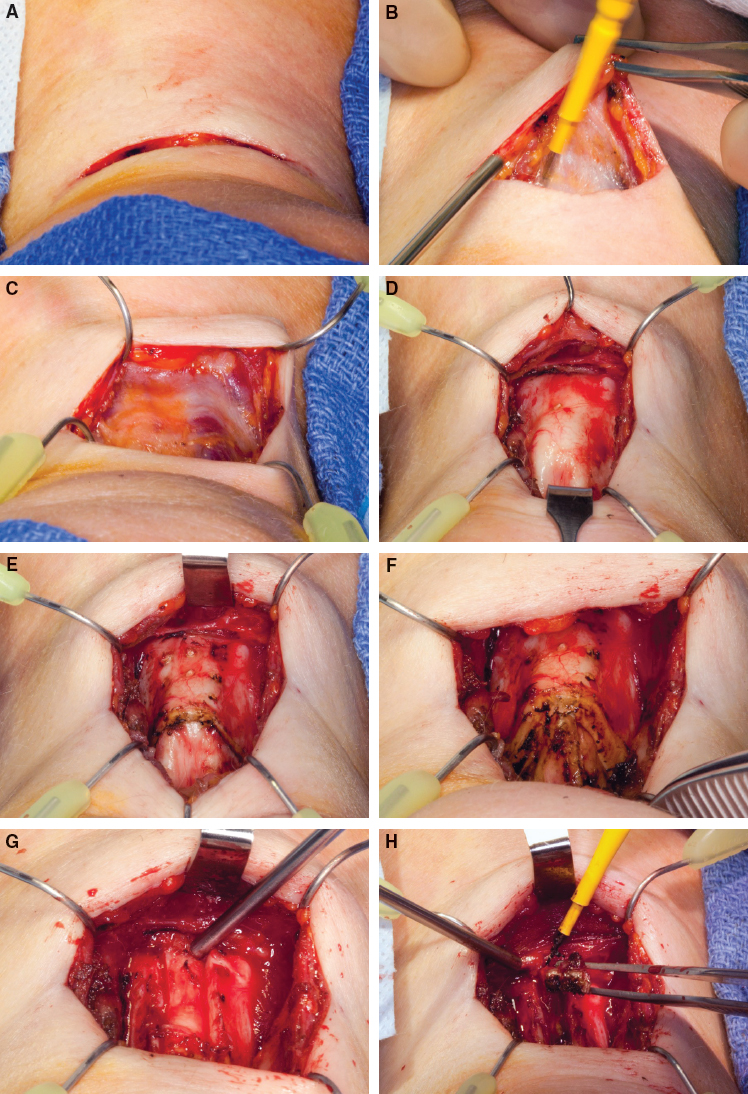
CHAPTER 2 Surgeons should take a history from patients that elicits the reason they wish to change their voice. Many individuals have the primary complaint that they identify with the female gender and are living as females, but when they speak, their voice betrays them. This may range from (1) never passing as a female once they speak to (2) passing as a female in person but not on the phone to (3) passing as a female all the time, but fatigue or discomfort sets in after prolonged speaking in a feminine voice. There is also relatively more nuanced reasoning, such as a desire to feel female without the need to think about sounding female; that is, naturally sounding female. Some individuals express the desire to sound more gender neutral. Another indication is an individual who sounded female until the thyroid cartilage reduction procedure. A voice recording should be made of the following vocal capabilities: This degree of vocal assessment will adequately document the voice both in pitch range and quality before and after surgical intervention. The surgeon can use this type of evaluation to learn what is working well and what is not. It also provides legal documentation that is more believable than a written assessment. Vocal assessment may also provide valuable feedback to patients, who hear their voice internally in a manner that is significantly different from the way others hear it. Often enough, individuals express that they sound the same after voice surgery; however, before and after recordings can provide feedback about the degree of change and improve a patient’s confidence in the new voice. Recording an endoscopic examination (with audio) provides vital information to the surgeon about the effects of surgical intervention and augments legal documentation. An endoscopic recording of the pharynx at low and high pitches documents a portion of vocal resonance variation. An endoscopic recording of the vocal cords should include quiet respiration, sniffing for maximal abduction, and phonation. A stroboscopic examination, including phonation at a comfortable speaking pitch and then at a high and low pitch, completes the examination. Informed written consent for the procedure and the precise procedure depend on the voice modification planned. Six current techniques are currently used alone or in some combination: cricothyroid approximation (CTA), laser vocal cord reduction, vocal cord webbing, anterior commissure advancement, anterior partial laryngectomy, and thyrohyoid elevation. Surgeon preference seems to currently drive the choice of procedure, but each has some pros and cons. In addition, some combination of procedures occasionally provides an optimal voice. CTA,1–8 which is one of the simplest and most commonly performed pitch surgeries, mimics the normal action of the cricothyroid muscle to lengthen the vocal cord.9 The vocal quality produced by this increase in tension (by lengthening) of the vocal cord is called falsetto. By bringing the thyroid cartilage and cricoid cartilage into approximation in the anterior midline, CTA surgery effectively sutures the cricothyroid muscle into a permanent position of contraction, although the degree is variable. Some of the positive attributes of CTA surgery include: However, significant issues were noted with the CTA procedure. Some patients experienced an initial elevation in pitch that faded back to a baseline pitch over a few months; ultimately they had no permanent change in their voice. This occurred in about one third of patients, although the vocal cords remained visibly stretched on endoscopy. Neumann and Welzel7 also noted that about one third of patients had a neutral pitch, and about one third failed to gain in pitch. During attempted surgical revisions, in which various sutures and suture placement techniques were used, no cricothyroid suture failure was noted. The cricothyroid space remained ablated despite inadequate pitch elevation, typically with the cricoid and thyroid cartilage fused in the anterior midline. Although various suturing techniques are used, it is uncommon to have sutures pulled out. Internally, during quiet respiration, the vocal process and membranous vocal cord margins are often in alignment, a position typically only seen when the cricothyroid muscle is contracted. Patients appear to lose pitch elevation by losing internal vocal cord tension. Another problematic issue with patients undergoing CTA surgery is that many patients with successful pitch elevation may speak with an unnatural, hyperelevated pitch, ranging from an extreme falsetto to a mild falsetto quality to the voice. Patients may describe this as a “gay male” sound. My experience with revision surgery is that the cricoid and thyroid cartilages frequently fuse in the anterior midline. However, even when separated, patients do not typically regain control over their falsetto range. It is theorized that the cricothyroid joints ankylose after a sufficient period of immobilization and may subsequently become fixed, perhaps subluxed, such that an individual may almost completely lose the ability to change pitch and volume at all, leaving the individual with a monotonal voice. Despite a successful change in comfortable speaking pitch, after CTA a patient forfeits the use of her cricothyroid muscles. Tensioning the thyroarytenoid muscle must now produce all pitch changes. There are various types of lasers and various modalities for using lasers on the vocal cords. One type of laser treatment, laser-assisted voice adjustment, attempts to increase vocal pitch through a thinning and tightening of the vocal cords. Increases in fundamental frequency with this technique tend not to be as large as with other surgical methods.11 One advantage is that no external incision is required. Laser-assisted voice adjustment may be used after CTA for enhancement of pitch if needed. In the operating room, the CO2 laser may be used to incise the superior surface of the vocal cord adjacent to or within the ventricle. The thyroarytenoid muscle can be removed through the incision; however, a patient can expect a prolonged period of aphonia if bilateral surgery is performed (1 to 3 months), presumably from edema and stiffness despite avoiding the vocal cord margins. This laser has been useful in raising pitch and pulling vocal cord margins to a straight position after other types of surgery, such as webbing or feminization laryngoplasty, improving volume, clarity, and pitch.12 Vocal cord webbing,11,13–15 which has recently gained in popularity, is an attempt to shorten the effective vibratory length of the vocal cords. This procedure is performed with microlaryngoscopy with the patient under general anesthesia. There is no external incision. Surgeons have removed mucosa from the anterior vocal cords, and some surgeons also remove some muscle. The raw edges of the anterior vocal cords are sutured together.15 Suturing within the laryngoscope is a technical challenge for some, and an experienced surgeon should be sought. Tucker16 described anterior commissure advancement, and Somyos Kunachak (personal communication, 2015) more recently performed a modification of this procedure. A skin incision is placed over the thyroid cartilage. The thyroid cartilage is incised vertically, leaving the anterior commissure attached. After pulling this forward, sutures may be placed through the remaining thyroid cartilage and vocal cords, securing the advancement. The advanced strut may then be removed. Kunachak et al17 proposed an open laryngoplasty to alter pitch. This procedure reduced the size of the larynx to a more female size in its cross-sectional dimension and shortened the length of the vibratory vocal fold. Transgender patients particularly adept at creating a female voice quality are able to maintain muscle tension with two pharyngeal parameters: elevation of the larynx and narrowing of the pharynx. Based on these, I have begun to suspend the larynx higher in the neck (thyrohyoid elevation component), shortening the chamber. This modification still requires the patient to address the diameter of the chamber with muscle contraction. A local anesthetic, with or without sedation, is used. The incision is placed within or parallel to a skin crease, preferably within 1 cm of the cricothyroid space. The patient is placed in the supine position, and the head may be extended with a shoulder roll if needed to allow adequate room to work over the cricothyroid space. The surgeon makes a horizontal incision, dissects through the adipose tissue, and raises the superior and inferior flaps, visualizing the strap muscles. The strap muscles are divided in midline. The larynx is exposed from the midthyroid cartilage superiorly to the inferior border of the cricoid cartilage. The perichondrium is incised along the inferior border of the thyroid cartilage and elevated from the thyroid cartilage for 3 to 5 mm along the inner lamina. A 1 mm hole is drilled in each side of the thyroid lamina, angling inferiorly. The cricoid cartilage perichondrium is incised along the superior border, and a tunnel is created beneath the cricoid cartilage. A permanent suture, such as 0-Ethibond, is passed around the cricoid cartilage from below. The suture may grasp a small amount of the cricothyroid tissue and is passed from the posterior aspect of the thyroid cartilage out the drilled hole. A second suture is passed in a similar fashion through the second hole. The sutures are drawn tight (while the surgeon may listen to the change in voice) and tied. Neck incisions may be closed with a 4-0 Monocryl suture, placing a single inverted suture to draw the strap muscles back to midline. Inverted sutures are placed in the deep subcutaneous layer that aligns with the platysma. A single running subcuticular suture closes the epithelium in a cosmetic fashion, from lateral to the incision and ultimately exits through the skin on the opposite side. Cyanoacrylate glue is used on the skin. No ancillary procedures are performed. The patient may speak. No voice rest is required. The incision may be wet after 24 hours. A topical anesthetic is used; 4% lidocaine is sprayed in both nostrils, along with a decongestant such as oxymetazaline. A mixture of 4% lidocaine and phenylephrine, along with stevia and peppermint for palatability, is used. Then 4% lidocaine (up to 4 ml) is gradually dripped onto the phonating vocal cords, creating a laryngeal gargle. The effects of the topical anesthetic last 15 minutes or more. There are no markings. The patient is seated. Frequently a sniffing position everts the larynx for better exposure. A KTP laser may be used to create a burn on the superior surface of the vocal cords, which results in a contracture and tightening of the vocal cord margins. A KTP laser fiber of 400 to 600 nm is passed through the working channel of the endoscope. The endoscope is passed through the larger nostril. It is more challenging to make the bend in the nasopharynx with the 600 nm fiber. Typical settings are 30 W, with a pulse width of 40 ms and a repeat of 2 pulses per second. By positioning the fiber close to the mucosa, a burn may be created along the superior surface of the vocal cord, working from just lateral to the vibratory margin into the laryngeal ventricle. The surgeon is careful to avoid a burn on the vibratory margin of the membranous vocal cord. The posterior limit is the vocal process, and the anterior limit is the anterior commissure. As the mucosa is cauterized, it turns white and may even be vaporized, leaving muscle exposed. Occasionally the false vocal cord is so large that it is difficult to reach the superior surface with the laser. Instead of applying the energy during respiration, the patient may phonate softly, bringing the vocal cords into adduction, for periods of 10 to 15 seconds. It is easier to determine the vibratory edge during phonation, and high pitch phonation will expose more of the surface than low pitch. A similar degree of burn is applied to the contralateral vocal cord. Because of the lateral position of the laser fiber within the endoscope, the surgeon’s view may be obscured while trying to reach the superior surface, and the endoscope may need to be withdrawn, inverted, and reinserted. A 10 Fr suction catheter may be placed through the smaller nostril and attached to a smoke evacuator suction. The patient and staff members wear eye protection. Although patients may speak after the procedure, their voice will deepen as swelling sets in. When monitoring patients after surgery, those who talk tend to induce more bruising on the vocal cords. Consequently, it is recommended that patients have 1 week of voice rest. The voice gradually becomes smoother, and the pitch rises over about 6 weeks in most patients. General anesthesia with a 6-0 laser-safe endotracheal tube is used. There are no markings. The patient is in the supine position. The patient’s head may be elevated into a sniffing position for improved exposure of the laryngeal introitus. A programmable CO2 laser (DEKA, Florence, Italy) may be used to incise the superior vocal cord’s mucosa and debulk some of the thyroarytenoid muscle. Typical settings of 10 W and a 0.8 mm depth may be used. A line length of 40% (about 4 mm) is also used. Each laser device may have different settings. The goal is to use the cutting aspect of the laser while minimizing collateral thermal damage. An incision is made in the superior surface of the vocal cord along the central 80% of the length of the membranous vocal cord. The incision is centered at approximately the edge of the laryngeal ventricle. The incision is spread open, and the thyroarytenoid muscle is gradually removed. I often err on the side of removing too little muscle and on the side of doing the least thermal damage to the remaining muscle. The incision, if narrow, may be left to close by secondary intention, or alternatively, 8-0 Vicryl suture may be used to close the incision with a single stitch to expedite healing. No ancillary procedures are performed. Although the patient may be allowed to speak after the procedure, she quite possibly will become aphonic, because there can be significant intracord edema. The more muscle removed, the longer the period in which the vocal cord margins will not vibrate. However, as long as there is no thermal damage to the vibratory margin, the voice will return when the margins become flexible again. General anesthesia with a 6-0 laser-safe endotracheal tube is used. There are no markings. The patient is in the supine position. The patient’s head may be elevated into a sniffing position for improved exposure of the laryngeal introitus. The patient and staff wear protective eyewear. A programmable CO2 laser (DEKA) with settings of 5 W and a 0.45 mm depth is used, and the line length is set to 40% (about 4 mm). Each laser device has different settings, and the goal is to use the cutting aspect of the laser while minimizing collateral thermal damage. A 6-0 nylon suture is placed, starting at the midportion of the incision and passing into the right vocal cord’s superior cut edge of mucosa through the thyroarytenoid muscle from the superior surface to the inferior surface and out through the inferior cut edge of mucosa. The suture enters the left vocal cord through the incised mucosa’s inferior margin, through the thyroarytenoid muscle from inferior to superior and exits through the superior cut edge of mucosa. At a slightly different position, the suture is passed through both vocal cords again. This figure-of-eight suture is pulled tight, bringing the raw edges of the muscle into apposition. A second suture is placed in the midmembranous vocal cord at the posterior extent of the incision. This will create the new anterior commissure. No ancillary procedures are performed. Patients should rest their voice for 2 weeks after surgery. General anesthesia, or possibly local anesthesia, is used. The markings are horizontal in or parallel to a skin crease overlying the thyroid cartilage. The patient is in the supine position. The anterior thyroid cartilage is exposed, and a vertical incision is placed about 2 mm on either side of midline. The central cartilage strip is pulled forward while the two thyroid alae are collapsed together beneath the advanced portion. Permanent sutures such as 4-0 nylon are passed through the cut anterior edge of the thyroid ala on each side, and the cut edges are drawn together with soft tissue compressed between them. After two or three are placed, the advanced piece of central cartilage may be removed. No ancillary procedures are performed. Voice rest may not be necessary. General anesthesia is used. The markings are horizontal in or parallel to a skin crease overlying the thyroid cartilage, approximately 5 cm long. The surgeon may be able to work through an incision as high as the hyoid bone, although the higher the incision placement in the neck, the wider the incision required, because the inferior skin edge needs to be pulled down to expose the inferior border of the thyroid cartilage. Clindamycin and cefotaxime are administered at the time of surgery. The patient receives 7 days of postoperative oral therapy with either cefuroxime or levofloxacin. The patient receives 10 mg of intravenous dexamethasone at the beginning of surgery. Oral prednisone or methylprednisolone is given postoperatively in selected cases if significant swelling develops 1 to 3 days later. The patient is in the supine position, with the neck extended. Superior and inferior flaps are elevated beneath the platysma layer. Strap muscles are separated in the midline, exposing the anatomy from the hyoid bone to the upper cricothyroid membrane (Fig. 2-1, A through D). If a thyrohyoid elevation is included, the upper 10 mm of the thyroid cartilage alae are removed with a knife or saw (Fig. 2-1, E and F). The surgeon must avoid going too far posteriorly, because this seems to cause edema and ecchymosis of the arytenoids. The thyroid cartilage is divided vertically with an oscillating saw about 4 to 7 mm on either side of midline; the saw kerf removes about 1 additional mm of cartilage (Fig. 2-1, G and H). The goal is to narrow the internal aperture of the laryngeal glottis by collapsing the thyroid alae medially. A prior CTA may preclude this removal.
Speech Modification
Key Points
 Surgery for male-to-female gender voice change is indicated by a patient’s dissatisfaction with his or her perceived gender. Typically this decision is based on sound alone, with male dominant characteristics.
Surgery for male-to-female gender voice change is indicated by a patient’s dissatisfaction with his or her perceived gender. Typically this decision is based on sound alone, with male dominant characteristics.
 Modification of voice pitch and resonance is possible in some individuals through practice or voice therapy.
Modification of voice pitch and resonance is possible in some individuals through practice or voice therapy.
 Multiple surgical approaches are available, but there is no single, clear, correct method.
Multiple surgical approaches are available, but there is no single, clear, correct method.
 Current methods include cricothyroid approximation, laser vocal cord thinning, anterior vocal cord webbing, anterior partial laryngectomy, thyrohyoid elevation, or some combination of these.
Current methods include cricothyroid approximation, laser vocal cord thinning, anterior vocal cord webbing, anterior partial laryngectomy, thyrohyoid elevation, or some combination of these.
 Surgery is the only way to correct the complication of vocal cord detachment after thyroid cartilage reduction, a frequent surgery during gender affirmation.
Surgery is the only way to correct the complication of vocal cord detachment after thyroid cartilage reduction, a frequent surgery during gender affirmation.
Indications and Contraindications to Surgery
Indications
 Individuals who cannot alter their voice through therapy or practice who want to be perceived as female by sound alone, such as during a telephone conversation
Individuals who cannot alter their voice through therapy or practice who want to be perceived as female by sound alone, such as during a telephone conversation
 Individuals who can voluntarily alter their voice to sound female but wish to remove even the potential for inadvertently sounding male if they let their guard down
Individuals who can voluntarily alter their voice to sound female but wish to remove even the potential for inadvertently sounding male if they let their guard down
 Individuals who can voluntarily alter their voice to sound female but wish to no longer think about sounding female before initiating each phonation and are willing to accept the risks of surgery
Individuals who can voluntarily alter their voice to sound female but wish to no longer think about sounding female before initiating each phonation and are willing to accept the risks of surgery
 Individuals whose speaking pitch and vocal range have dropped from the complication of vocal cord detachment after tracheal shave (thyroid cartilage reduction)
Individuals whose speaking pitch and vocal range have dropped from the complication of vocal cord detachment after tracheal shave (thyroid cartilage reduction)
Contraindications
 Individuals who cannot tolerate the chance that surgery will not accomplish a pitch and/or resonance change; all surgeries have the risk of incomplete alteration of the voice from male to female, and most surgery has some risk of no change in the gender quality of the voice
Individuals who cannot tolerate the chance that surgery will not accomplish a pitch and/or resonance change; all surgeries have the risk of incomplete alteration of the voice from male to female, and most surgery has some risk of no change in the gender quality of the voice
 Individuals who cannot tolerate a loss of maximal volume are not surgical candidates
Individuals who cannot tolerate a loss of maximal volume are not surgical candidates
Patient Evaluation
 Comfortable speaking pitch reading a standard passage of several sentences
Comfortable speaking pitch reading a standard passage of several sentences
 Lowest pitch that can be produced, including a glide downward
Lowest pitch that can be produced, including a glide downward
 Highest pitch that can be produced, including a glide upward
Highest pitch that can be produced, including a glide upward
 Loud phonation, a robust yell; vegetative sounds, cough, and a throat clearing
Loud phonation, a robust yell; vegetative sounds, cough, and a throat clearing
 Soft singing of several words at high and low pitches, such as “Happy Birthday to You”
Soft singing of several words at high and low pitches, such as “Happy Birthday to You”
Preoperative Planning and Preparation
Surgical Techniques
Cricothyroid Approximation
 The surgery is relatively easy to perform, because the anatomy is located very close beneath the skin.
The surgery is relatively easy to perform, because the anatomy is located very close beneath the skin.
 Surgeons inexperienced with the procedure can perform the technical aspect of the surgery relatively well.
Surgeons inexperienced with the procedure can perform the technical aspect of the surgery relatively well.
 There is minimal discomfort with the procedure, and it may be performed with the patient under local anesthesia.
There is minimal discomfort with the procedure, and it may be performed with the patient under local anesthesia.
 The patient may speak during the procedure, and for some, “CTA surgery is typically performed with intentional hyperelevation of pitch in anticipation of gradual relaxation of the induced vocal fold tension over time.”10
The patient may speak during the procedure, and for some, “CTA surgery is typically performed with intentional hyperelevation of pitch in anticipation of gradual relaxation of the induced vocal fold tension over time.”10
 Because this procedure is relatively easy to perform and safe from intraoperative surgical complications and can be performed in a relatively short time, surgical costs are low.
Because this procedure is relatively easy to perform and safe from intraoperative surgical complications and can be performed in a relatively short time, surgical costs are low.
Laser Vocal Cord Reduction
Vocal Cord Webbing
Anterior Commissure Advancement
Anterior Partial Laryngectomy
Thyrohyoid Elevation
Surgical Procedures
Cricothyroid Approximation
Anesthesia
Markings
Patient Positioning
Technique
Ancillary Procedures
Postoperative Care
Laser Vocal Cord Reduction: Tightening
Anesthesia
Markings
Patient Positioning
Technique
Ancillary Procedures
Postoperative Care
Laser Vocal Cord Reduction: Mass Reduction
Anesthesia
Markings
Patient Positioning
Technique
Ancillary Procedures
Postoperative Care
Vocal Cord Webbing
Anesthesia
Markings
Patient Positioning
Technique
Ancillary Procedures
Postoperative Care
Anterior Commissure Advancement
Anesthesia
Markings
Patient Positioning
Technique
Ancillary Procedures
Postoperative Care
Anterior Partial Laryngectomy
Anesthesia
Markings
Antibiotics
Steroids
Patient Positioning
Technique
Abdominal Key
Fastest Abdominal Insight Engine