Genital pelvic sites
Extragenital pelvic sites
Rare locations
Ovaries
Sigmoid colon
Umbilicus
Rectovaginal septum
Rectum
Small bowel
Anteroposterior cul-de-sac
Appendix
Lungs
Broad ligament
Bladder
Kidney
Cervix
Cesarean section/episiotomy scar
Vagina
Sciatic nerve
Fallopian tubes
Arms
Nasal mucosa
Spinal column
Liver
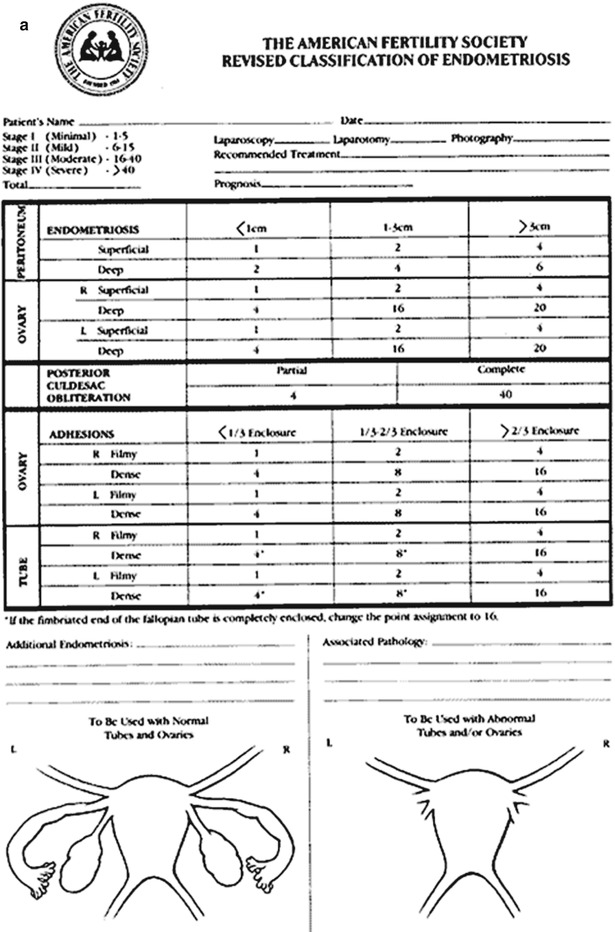
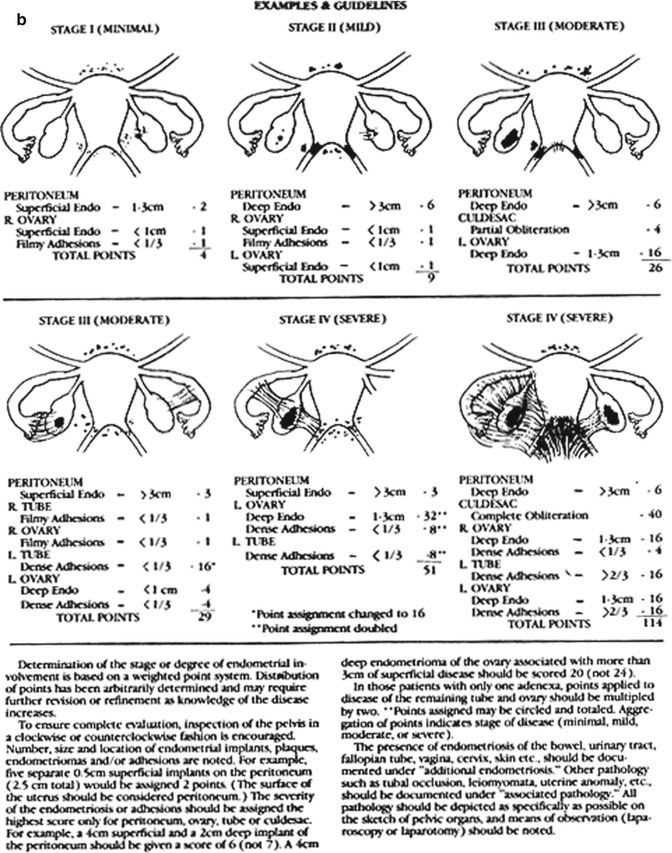
Fig. 12.1
(a, b) American Society for Reproductive Medicine Endometriosis Classification assigned points according to the severity of endometriosis on the basis of size and depth of implants and severity of adhesions. Stage I (1–5 points): minimal disease; Stage II (6–15 points): mild disease; Stage III (16–40 points): moderate disease; Stage IV (>40 points): severe disease
To felicitate a standardized approach to examine the pelvis in endometriosis patients, it was recently proposed that the pelvis could be topographically divided into two midline zones (Zone I & II) and two paired (right and left) lateral zones (Zone III & IV). Zone I is the area between the two round ligaments from their origin at the uterine cornua to their insertion in the deep inguinal rings. Zone II is the area between the two uterosacral ligaments from their origin from the back of the uterus to their insertions in the sacrum posteriorly. Zone III is the area between the uterosacral ligament inferiorly and the entire length of the fallopian tube and the infundibulopelvic ligament superiorly. Zone IV is the triangular area lateral to the fallopian tube and the infundibulopelvic ligament and medial to the external iliac vessels up to the round ligament (Fig. 12.2
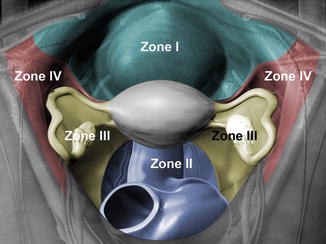
) [2].
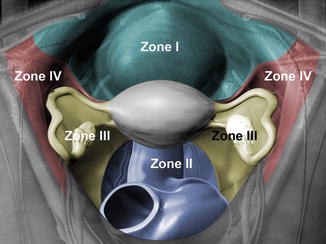
Fig. 12.2
A color-coded illustration of the anatomical boundaries and the contents of all pelvic zones. Zone I: Midline anterior abdominal cavity limited by the round ligaments bilaterally. Zone II: Midline posterior zone of the abdominal cavity limited by the uterosacral ligaments bilaterally. Zone III: Lateral pelvic side walls limited by the uterosacral ligament and the adnexae and infundibulopelvic ligamentsone IV: Pelvic side wall limited by the round ligament, adnexae and infundibular ligament, and external iliac vessels
12.2 Surgical Management of Endometriosis
Surgery may be indicated in women who suffer severe disease, do not respond to medical therapy, or desire fertility. The indications for surgical intervention are summarized in Table 12.2. Endometriosis can be challenging to manage surgically because of the peculiarities of the disease. Because it is adhesive, widespread, infiltrative, and recurrent, the objective of surgical management is to safely resect or ablate all visible disease. To date there are four primary surgical options. Traditional laparotomy is associated with longer recovery and hospital stay but may be necessary for advanced disease with extensive adhesions or involvement of the ureter, bladder, uterine arteries, and/or bowel. Laparoscopy is an alternative minimally invasive approach that has been shown to be equally effective in resecting endometriomas. Robotic-assisted laparoscopy is another new modality that has been reported.
Most recently, laparoendoscopic single-port surgery (LESS) has emerged as a minimally invasive approach. Compared to traditional laparoscopy, it is associated with better cosmetic results, a shorter hospital stay, and less postoperative pain. It has been used extensively for a wide variety of gynecologic indications. More recently, LESS was used in an attempt to treat endometriosis requiring a single incision [3–6].
Table 12.2
Indications for surgical management of endometriosis
Severe incapacitating symptoms with significant functional impairment |
Advanced disease with distortion of pelvic organs |
Failure of expectant or medical management |
Noncompliance with or intolerance to medical treatment |
Endometriosis emergencies |
Ruptured or torsed endometrioma
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





