Fig. 17.1
(a) Patient positioning for single-docking totally robotic LAR or ISR. (b) The robotic setup for single-docking totally robotic LAR or ISR
As the patient will remain in this position for a significant amount of time, care should be taken to ensure the patient would not slide on the operating table during the case. In our institution, we use a surgical beanbag mattress to keep the patient in place.
The patient cart is positioned and docked obliquely at left side of the patient. Also note the robotic arms are well fanned out to minimize external collision (Fig. 17.1b).
During the operation, both the assistant and the scrub nurse should stand on the patient’s right side. This allows them access to the robotic instruments. The video cart is placed toward the right foot of the patient to allow visualization of the video screen.
17.2.3 Trocar Placement
Pneumoperitoneum can be established via either Veress needle, direct optical entry, or direct cutdown. Our preferred method is direct cutdown.
Our standard robotic setup includes five instrument ports in addition to the camera port (Figs. 17.2 and 17.3). RLQ port is usually placed at McBurney’s point. It is important to avoid bony structures such as the iliac crest to allow maximum range of motion for the robotic arm. Another consideration is also given if covering ileostomy is required as this port site will be used for ileostomy.
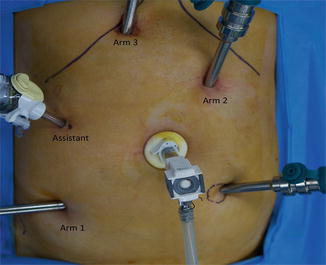
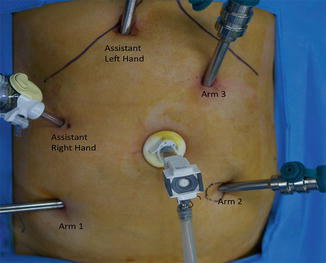
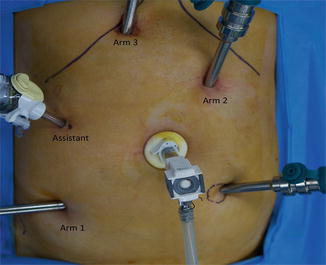
Fig. 17.2
Port placement for abdominal phase
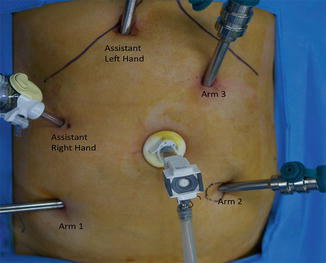
Fig. 17.3
Port placement for pelvic phase
RUQ port is placed 2 cm from the costal margin and just medial to the midclavicular line. Left-side ports are placed along left midclavicular line. The LUQ port is placed at a lower level to the RUQ port to avoid clashing during colonic dissection.
The assistant port is placed in right-flank position between the RUQ and camera port.
Trocar placement is of importance to prevent problems during the operation. Distance between camera/instrument and target anatomy and the distance between the instrument ports are also important. The camera port should be at least 15 cm from target anatomy. The distance between the instrument ports on the same side of the patient should be at least 8 cm apart. The angle between the two right-side instrument ports should be as wide as possible (Fig. 17.4). Correct trocar placement will prevent clashing of the instrument arms during surgery.
Fig. 17.4
Diagram showing the angle between the robotic ports in RUQ and RLQ should be as wide and long as possible
17.2.4 Initial Laparoscopy
Full initial diagnostic laparoscopy is performed looking for evidence of peritoneal or metastatic disease.
Divide any adhesions that may limit mobilization and exposure.
The aim is to expose the left colon, base of the mesentery, and inferior mesenteric artery (IMA) and vein (IMV).
The omentum is retracted above the stomach and the liver along with the transverse colon. The weight of the omentum, along with Trendelenburg position, helps keep the transverse colon way from operative field.
Retract small bowel loops medially and toward RUQ.
Assess the left colon and sigmoid. Sometimes the mobilization of the splenic flexure may not be necessary if there is redundant sigmoid colon.
One or two pieces of small gauze may be placed intraperitoneally to help retract the small bowel.
In female patients, the uterus is best retracted away using sutures.
17.2.5 Docking: Single vs. Double
Various robotic techniques have been described in literature, including hybrid, double docking, and single docking. The authors have developed the single-docking technique over many years involving significant patient numbers and believe this method provide excellent exposure. This is the method we shall describe in detail.
17.2.5.1 Hybrid Approach
The splenic flexure and left colon is mobilized laparoscopically. The patient cart is then docked either at an angle on the patient’s left side or between the legs for pelvic dissection.
17.2.5.2 Double Docking
Two separate dockings include the initial docking for mobilization of splenic flexure and the second docking for sigmoid and pelvic dissection. An alternate technique recently described is to undock the patient cart, but rather than move the patient cart, the patient bed is moved instead into the new position.
17.2.5.3 Single Docking
The patient cart is obliquely placed on the patient’s left. The central column of the patient cart should line up along an imaginary line between the camera port and the left anterior superior iliac spine.
Moving the robotic arms into different ports allows both dissection of the left colon/splenic flexure and pelvic dissection. Docking on the patient’s left also allows access to the patient’s perineum, enabling the surgeon to check his/her dissection by digital examination without undocking the patient cart.
17.3 Abdominal Dissection
17.3.1 Port Placement (Fig. 17.2)
Instrument arm 1: monopolar curved scissors through the RLQ port.
Instrument arm 2: Maryland bipolar forceps through the LUQ port.
Instrument arm 3: Cadiere forceps through the RUQ port.
The assistant utilizes a grasper and a sucker through the assistant port on the right flank.
17.3.2 Medial-to-Lateral Approach
This is the standard practice of this department.
The sigmoid colon mesentery is lifted up using arm 2 to reveal the base of the mesentery and IMA (Fig. 17.5). The assistant uses a non-toothed grasper to retract the small bowel away from operative field. Mesentery above sacral promontory is incised and dissected using arms 1 and 3. The IMA is identified and skeletonized. The aorta is used as a landmark for dissection of the IMA. Keep the aorta horizontal while visualizing the IMA. A D3 dissection is performed by dissecting a cuff of the mesentery at least 1 cm around the origin of the IMA and included in the specimen, while the periaortic sympathetic nerve plexus is preserved (Fig. 17.6). Once skeletonized, the IMA is ligated at its origin with Hem-o-lok clips. This can be performed either by the assistant or via the robotic arm. Using the robotic arm does require exchanging the instrument arm but does have the advantage of better rotation and angulations provided by the robotic wrist. It is best if the IMA is not ligated flush against the aorta. A short cuff is recommended in case of bleeding.
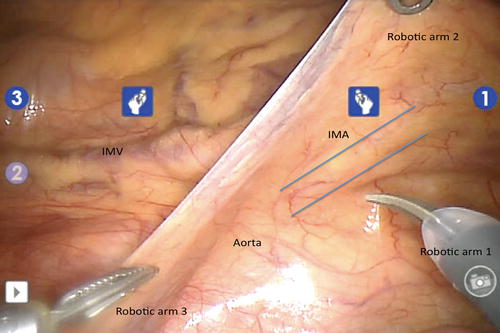
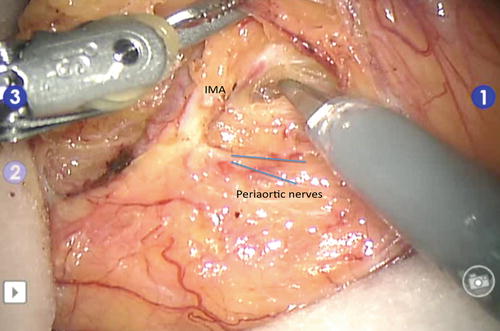
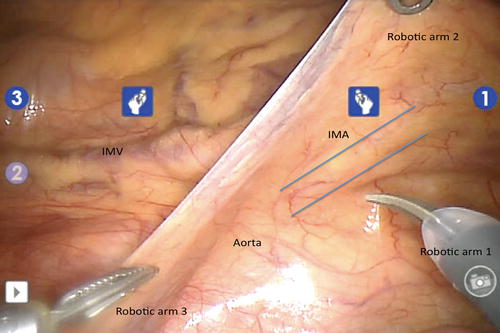
Fig. 17.5
Exposure of the IMA. Arm 2 retracts the sigmoid mesentery toward anterior abdominal wall, leaving both arms 1 and 3 for dissection
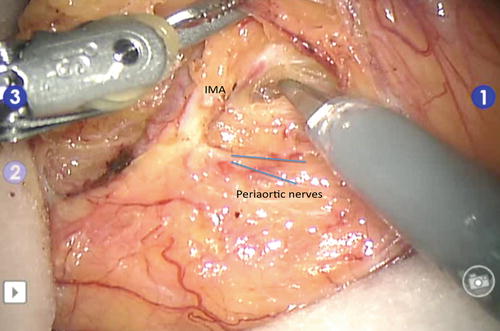
Fig. 17.6
The IMA is skeletonized and the periaortic sympathetic nerves are preserved
We have also developed a technique for patients with cardiovascular diseases whereby the IMA is ligated at a low level while preserving the left colic vessels but oncological resection is not compromised by including the same mesenteric tissue in the final specimen. This is done by carefully skeletonizing the IMA, dissecting mesenteric tissue from the IMA, until the left colic artery is identified. Mesenteric tissue is dissected off the left colic pedicle to allow the IMA to be ligated above the left colic branch.
It is of importance to identify the nerves and preserve them. The 3-dimensional view is very helpful in identifying the nerves. By skeletonizing the IMA, the nerves are better identified and preserved. The assistant may assist with retraction with a sucker or grasper.
The IMA is then lifted toward the anterior abdominal wall and the descending colon and sigmoid mesentery is dissected from the retroperitoneum. Dissection is performed by using a sharp dissection. The plane between the mesentery and the Gerota’s fascia can be identified using both traction and countertraction of both arms 2 and 3. Sometimes the plane can be better identified by gentle pushing using the instrument arms. It is important to constantly reposition arm 2 to help with retraction. Arm 2 should be retracting the mesentery upward toward anterior the abdominal wall. This allows arm 3 to be used for countertraction. Any bleeding can be controlled using bipolar in the left robotic arm (arm 3) or the monopolar scissors in the right arm (arm 1).
Dissection of the colonic mesentery off the retroperitoneum is continued proximally toward the splenic flexure. The IMV is identified on the lateral side of the duodenum and dissected.
Before ligation of the IMV, the arc of Riolan (otherwise known as the meandering artery) should be sorted. The arc of Riolan, when present, may be significant in affecting the blood supply provided by the marginal artery. If required, the IMV should be ligated to ensure the arc of Riolan remains intact (Fig. 17.7). Ligation of the IMV does not affect oncological outcome but provides mobilization of the left colon to reach the pelvis during anastomosis.
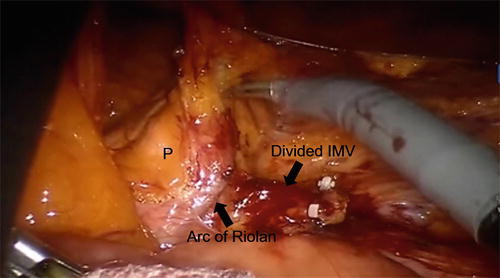
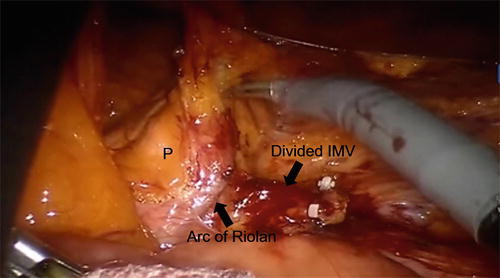
Fig. 17.7
Preservation of arc of Riolan. P pancreas
The boundaries of medial dissection are the inferior border of the pancreas proximally and the aorta medially. Laterally, dissection is carried out as far laterally as possible until the visualization of the psoas muscle. The left ureter should be visualized crossing the left iliac vessels and preserved.
If the splenic flexure is mobilized, proximal dissection is extended above the pancreas and lesser sac entered inferiorly during medial dissection. This is done by incising the peritoneum overlying the transverse colon mesentery at the level of the pancreas. Dissection of the mesentery off the superior aspect of the pancreas will lead you into the lesser sac. Once lesser sac is entered, the transverse colon mesentery can be dissected off its attachment to the anterior aspect of the pancreas (Fig. 17.8). The assistant places the grasper into the lesser sac and lifts the transverse colon mesentery upward. This dissection is carried laterally toward the splenic flexure. This is identified by the omentum that attaches to the tail of the pancreas.
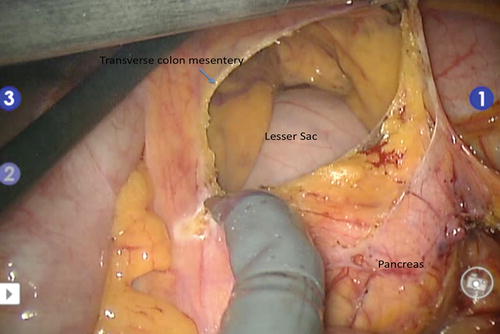
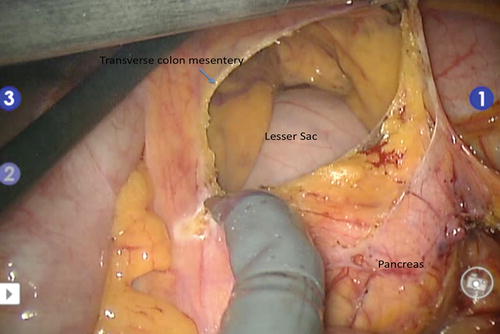
Fig. 17.8
Medial dissection above the pancreas to enter the lesser sac and dissection of the transverse colon mesentery off the pancreas. The black-colored instrument is the assistant’s grasper
Once medial dissection is complete, lateral dissection can be performed. The sigmoid colon is separated from its peritoneal attachments commencing at the sigmoid notch by dissecting along the line of Toldt. The colon is retracted medially and inferiorly (i.e., toward the RLQ) by the assistant and left for the surgeon’s left robotic arm to be used for countertraction (Fig. 17.9). If the medial dissection is adequate, lateral dissection should quickly join the dissection as previously done medially.
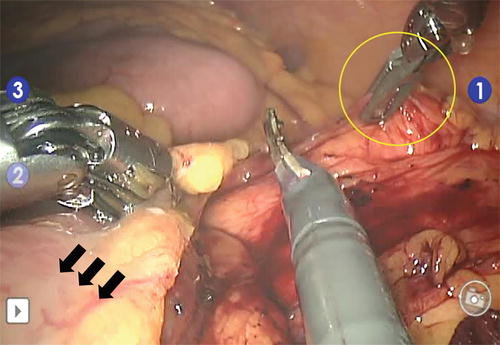
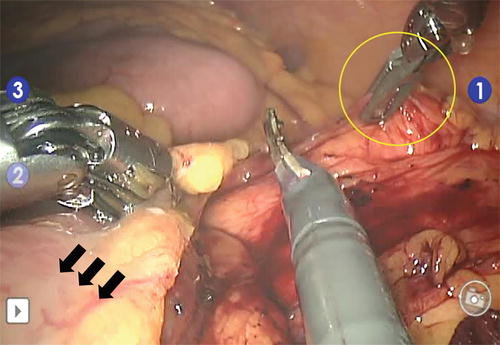
Fig. 17.9




The descending colon is retracted medially and inferiorly by the assistant (arrows) and surgeon’s left robotic arm is used for countertraction (yellow ellipse) during lateral dissection
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







