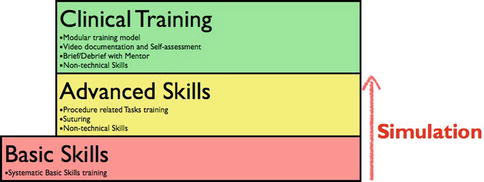
Fig. 2.1
Factors affecting the clinical pathway of a surgical patient. The WHO checklist for surgical safety is a means to ensure Human and Team factors. A quality control for surgeon factors is challenging but can be achieved by step-wise, modular training systems (Adapted from Patel and Joseph [5])
Surgical training is currently challenged by working hour directives and high quality standards. The traditional “master-apprentice” model cannot meet the demands of high quality, increasingly complex procedures and the need for new surgeons. Simulation training is effective and a means to shorten learning curves in laparoscopic surgery [7]. Simulation training is often divided into basic skills training, advanced skills training and laparoscopic team training (Fig. 2.2). Basic and advanced skills training is preferably done in box trainers and/or Virtual Reality (VR) simulators. Both are proven effective for the training of spatial skills and eye-hand coordination [7]. Box trainers are cheap and versatile, VR simulators include the advantage of objective assessment and progress reports, repeatability and standardization of the tasks [8]. Training curricula using VR simulators for standard procedures e.g. laparoscopic cholecystectomy have been shown to shorten learning curves and improve technical proficiency compared to standard training [9,10]. These training programs generally consist of an initial basic skills training followed by procedure related tasks.
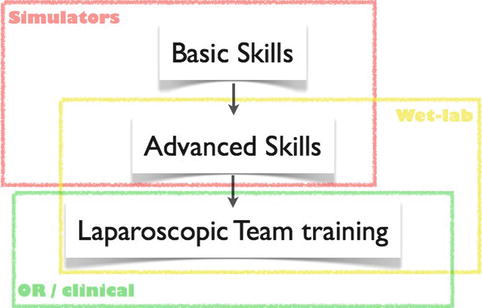
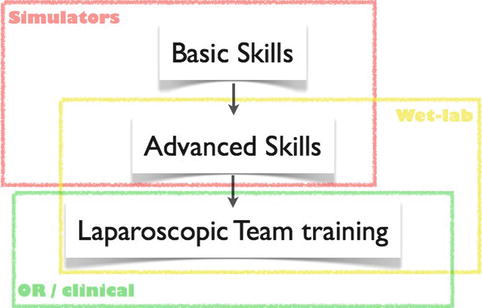
Fig. 2.2
The three steps of laparoscopic training. Basic and advanced skills are trained in simulators. Advanced skills can also be trained in animal models/wel-lab. Laparoscopic team training is usually done in a clinical setting but is also possible in a wet-lab
Laparoscopic pelvic surgery has early on been considered technically challenging due to limited work space, complex anatomy and in many cases the need for reconstruction, i.e. suturing. Attempts have been made to classify the level of difficulty of laparoscopic procedures in order to improve training [11]. In a traditional master-apprentice surgical training model, a sequential allocation of procedures by the degree of difficulty would be reasonable but is time-consuming, inefficient and impracticable. Also, the level of difficulty of a procedure basically refers to the difficulty of learning the necessary skills to perform the procedure. Thus, simulation in surgical training attenuates long and challenging curricula for advanced laparoscopic surgery, in particular pelvic surgery.
In complex laparoscopic surgery, learning curves are often considered to be a measure of how many procedures a trainee has to attend/perform in order to become competent. However, the sole number of procedures does not reflect the level of difficulty of the case or if the procedure was successful. Performing a minimum number of procedures does not necessarily lead to competence. In many European countries, this system of a minimum number of different procedures is used in the accreditation of surgeons. Even though this quality control appears better than no specified requirements at all, it is possible to differentiate the factors that determine whether a single procedure is a “rookie” or “expert” case. For instance in prostate cancer prostatectomy, prostate size, clinical tumor stage, histological tumor burden and pelvic comorbidity are factors that complicate the procedure and increase the level of difficulty. A preoperative assessment of surgical risk factors increases the preparedness of the trainee.
Laparoscopic pelvic surgery usually involves many steps and reconstruction towards the end of the procedure. Performing a complete procedure is oftentimes overwhelming for a trainee. Breaking down the procedure into steps and subtasks is in this respect beneficial. The trainee can perform single subtasks or steps of the operation that have been assigned different levels of difficulty. As the clinical training progresses, the trainee performs steps with gradually increasing level of difficulty. The easier steps are then done by another trainee or the mentor, so that the trainee can focus on a defined task. This training concept is known as modular training and has been validated for e.g. laparoscopic radical prostatectomy. Interestingly, the modular approach in training shortens the learning curve significantly without compromising outcome [12,13].
Another underestimated asset to surgical training is self-observership and assessment. Laparoscopic procedures should in principle be recorded for documentation and the self-assessment of the trainee—preferably together with a mentor—improves training. Such debriefs can be done straight after the procedures or later. The self-observation and assessment shortens the learning curve and is highly motivating for trainees. However, dedicated mentors and time for debriefs must be provided to implement this concept. The principle of self-assessment is widely used in e.g. aviation and athletics and has been shown to improve training in a simulated environment. Laparoscopic suturing skills in surgical trainees improve significantly by video self-assessment mirroring the training effect of a larger volume [14]. This training effect is also applicable to single steps or complete procedures and the debrief sessions utilize this effect.
In addition to self-assessment, athletes have long used mental training to improve preparedness and focus and ultimately improve their performance. Interestingly, mental training can also be utilized in simulation training. In a recent study by Eldred-Evans et al. [15] and colleagues, medical students performed two basic laparoscopic tasks in a box trainer and VR Simulator. They were randomized to either box training, box training supplemented by a VR simulator session, box training supplemented by mental training or VRS training supplemented by mental training. Mental training consisted of one session of 30 min. The tasks, e.g. cutting a circle, were divided into 12 sub-steps, so-called nodal points. The mental training session focused on mental visualization of these nodal points. All participants were assessed after the intervention, both in a box trainer and a VR simulator. The combination of box training and mental training lead to the highest scores with regards to precision, accuracy and overall performance when assessed in a box trainer. In the VR simulator assessment, the combination of box training and VR simulator performed best followed by box training and mental training. The group that did not receive any box training had the lowest scores with regards to speed, precision, accuracy and performance compared to the other groups regardless if assessed in a box trainer or VR simulator. The study shows that mental training as a supplement to box training improves laparoscopic skills compared to box training alone. Interestingly, this enhancing effect does not seem to apply to VRS training. One reason might be that mental training enhances the sensory experience acquired in the box trainer. The VRS trained group might lack these due to limited haptic feedback of the system. Also, mental training alone cannot replace conventional training. In a study with similar design, a group of novices merely received mental training and the post-training assessment could not match the effect of box or VRS training [16].
In both studies, skills acquired in box training were transferable to VRS assessment while not all skills acquired in VRS training were reproducible at box trainer assessment. This shows that box trainers still are the mainstay for basic skills training.
Mental training amends basic skill training in a simulated setting and the implementation has great potential. However, the principle can already be utilized in clinical training. In modular training, the trainee performs a number of predefined steps of an operation and the focus on particular tasks increases the trainee’s preparedness. This can be formalized by a short, preoperative briefing where technical aspects of the steps are repeated. This mental rehearsal improves performance [17] and is supported by the postoperative debrief session including video assessment.
2.2 How to Set Up Simulation Training for Pelvic Training
Simulation training for any surgical specialty that involves laparoscopic technique should start with basic skills training. This should be organized as a systematic, structured program with defined tasks and certification of the participants. A certification of basic skills is recommended since not all candidates will acquire the necessary skills within a given number of training sessions [18]. Next, more advanced and procedure-related simulation tasks are trained. There are numerous models for e.g. prostatectomy [19] and gynecological surgery [20]. The clinical training can start simultaneously. Specific tasks e.g. anastomotic suture in prostatectomy are practiced in a simulated setting (Fig. 2.3).