9 Quality Assurance in Endoscopy
Matthew D. Rutter
9.1 The Importance of Quality
In recent years, the publication of several key studies has brought the importance of quality in health care services into sharp focus. For example, a study from the United States in 2000 indicated that as many as 98,000 people were dying each year as a result of medical errors. 1 In endoscopy, which is a pivotal investigation in the diagnosis and management of gastrointestinal (GI) pathology, the quality agenda has been advanced further by the introduction of organized colorectal cancer screening programs. High-quality endoscopy delivers better health outcomes and better patient experience, 2 yet it is widely recognized that significant variation exists in the performance of endoscopists and of endoscopy units, 3 , 4 , 5 , 6 , 7 and as tens of millions endoscopic procedures are performed every year across the world, the potential health impact of suboptimal endoscopic quality is large.
The current variation in endoscopic quality between services and between individuals is best evidenced in colonoscopy. For example, a recent United Kingdom study demonstrated a fourfold variation in postcolonoscopy colorectal cancer (PCCRC) rates between hospitals. 8 It is known that the majority of PCCRCs arise from missed cancers, missed premalignant polyps, or incomplete polypectomy. 9 , 10 Back-to-back colonoscopy studies show that there is a three- to sixfold variation in adenoma detection rates (ADRs) between endoscopists, and even greater variation in serrated polyp detection rates. 11 , 12 Even when polyps are found, removal may be incomplete: the CARE study concluded that 10% of nonpedunculated polyps of 5 to 20 mm, 23% of nonpedunculated polyps of 15 to 20 mm, and 48% of serrated polyps of 10 to 20 mm were incompletely resected. 13
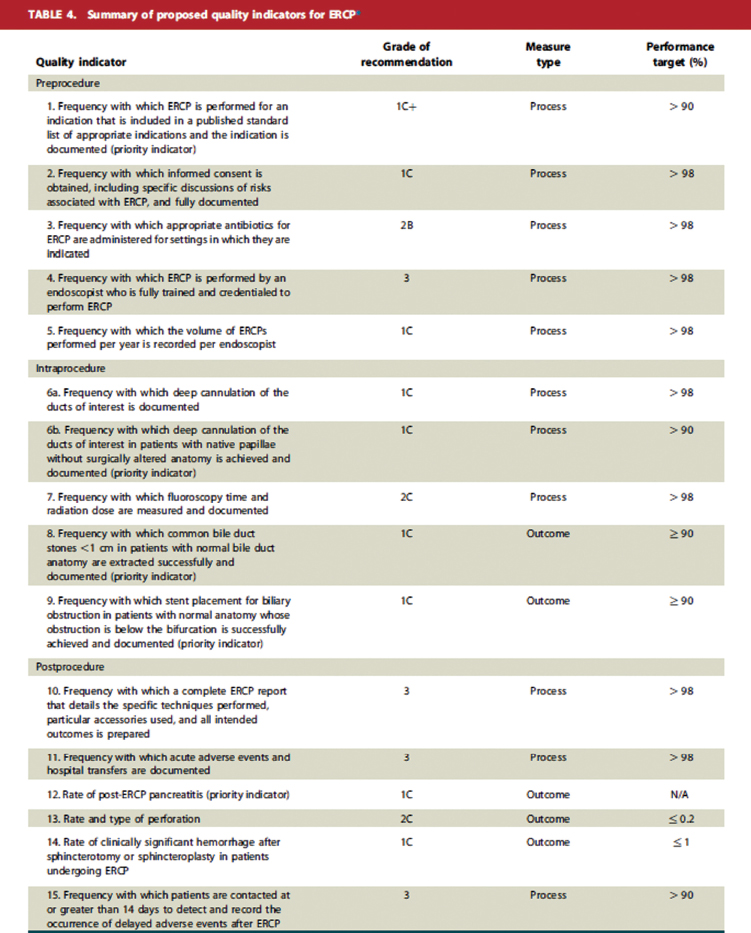
Quality variation is not limited to colonoscopy. In endoscopic retrograde cholangiopancreatography (ERCP), which is one of the most complex and high-risk commonly performed endoscopic procedure, a wide variation is seen in procedure completion and in complication rates. 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 Gastric cancers and precursor lesions are also frequently missed in the upper GI tract—in one series, 7.2% of patients diagnosed with gastric cancer had had a negative gastroscopy within the preceding year, of which around three-quarters were due to endoscopist error. 22
9.2 Performance Measures
Differences in endoscopic quality will only come to light if performance is measured. Services and individuals are unlikely to improve, nor can support be provided, unless they are aware of their performance and how it compares with benchmark standards. Such comparison can be a powerful motivator for individuals and services to improve, diminishing the variation in quality between endoscopists and services. It is also well-recognized that by simply monitoring a service, performance will improve—this is the Hawthorne effect, and it is essentially a free means to improve the quality of patient care.
Performance measures (PMs; also known as quality measures, quality indicators, key performance indicators, or clinical quality measures) are criteria that are used to assess the performance of a service or a component of the service. The provision of high-quality, patient-centered endoscopic care is complex, involving a multidisciplinary team, many detailed processes, and an array of specialist equipment to investigate and treat a wide range of people of differing age and comorbidity with differing levels of urgency. PMs can be used to measure all aspects (often called “domains”) of the endoscopic service, from preprocedure, through the procedure itself, and in the postprocedural period. Examples of domains include timeliness, completeness of procedure, identification of pathology, management of pathology, complications, and patient experience. Ideally, a small number of PMs should be used to assess each domain: used together, they provide a global overview of the quality of the service. A good example of this process is the Endoscopy Global Rating Scale (GRS) used in the United Kingdom, which is now adopted in many other nations (▶Fig. 9.1).

PMs can be categorized as outcome measures, structural measures, or process measures. Outcome measures assess the results of clinically meaningful aspects of care directly, and are usually considered the most important measures—for example, the pancreatitis rate following ERCP. However, it may not always be feasible to measure such outcomes—the data may be too difficult to capture, the event may be rare and therefore difficult to analyze with statistical certainty, or the timeframe to capture such data may be too long for it to be a useful measure of current performance (e.g., PCCRC rates, where several years need to pass before the true figure can be calculated). In these situations, the use of surrogate PMs may be required. These may also be outcome measures—for example, ADR is used as a surrogate for PCCRC rate. Where surrogate measures are used, it is desirable that there is evidence of a correlation between these measures and an important health outcome—reassuringly, in this example, there is increasingly compelling evidence demonstrating a strong correlation between an individual endoscopist’s ADR and its PCCRC rate. 23 , 24 Surrogate measures may also be structural measures, which look at aspects of health care infrastructure (e.g., information about staffing levels or whether a provider has an electronic endoscopy reporting system), or process measures, which measure whether specific quality actions are being implemented (e.g., the proportion of patients that have had a preprocedure endoscopy checklist completed; ▶Fig. 9.2—there is compelling evidence from surgery that the introduction of the WHO surgical checklist can result in a reduction of complications by a third and mortality by almost half). 25 , 26

Colorectal cancer screening has facilitated the implementation of PMs for diagnostic colonoscopy. However, measures for therapeutic colonoscopy and for most other aspects of GI endoscopy are either nonexistent or very much in their infancy.
It is usually desirable to identify a minimum standard and a target standard for each PM. Although PMs will remain relatively static over time, quality improvement is a dynamic process and as such the standards within such measures will usually increase over time as techniques and technologies improve. The standards may also vary according to the specific procedure—for example, the minimum standard for ADR will be higher for fecal occult blood diagnostic colonoscopy compared to screening colonoscopy. At present, there are many PMs where no evidence-based minimum standard has been defined. With time, further research can help determine what the appropriate standards should be; nevertheless, in the interim it may still be useful to measure and benchmark performance against other similar services.
An example of endoscopic PMs is given in ▶Fig. 9.3.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






