Fig. 12.1
DCT: manometric control of the bladder and bowel pressures
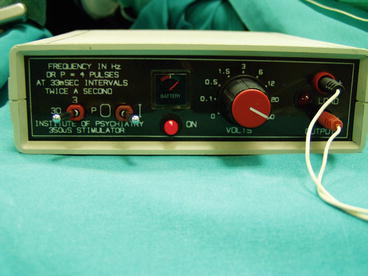
Fig. 12.2
DCT: external stimulator

Fig. 12.3
DCT: testing needles in S2 and S3 foramina, bilaterally. Patient cable stimulating right S2
Dysfunctional voiding with urinary retention can be regarded as the most suitable dysfunction to be treated with SNM. Negative control exerted toward the bladder by a contracted urethral sphincter (hyperexcitability of vesico-urethral reflex) maintains urinary retention. SNM modulates this dysfunctional reflex. The statement by Tanagho and Schmidt in 1991 [13] that “neuromodulation through foraminal stimulation of the sacral nerve depends on electrical stimulation of afferents axons that modulate sensory processing of the voiding reflex pathways of the central nervous system” is still up-to-date. During the last 15 years, research in the field of electrical modulation of the nervous system through the sacral nerves has refined and completed this initial hypothesis.
12.4 Sacral Neuromodulation: From Testing Its Efficacy to Follow-Up of Permanent Implant
Patients with urinary retention selected to receive SNM therapy have to be tested for the efficacy of functional treatment. Percutaneous needle testing of nerve functional integrity followed by placement of a temporary wire electrode (percutaneous nerve evaluation, PNE) has been used for years as the only tool for patient selection. The duration of the stimulation test varied from a few days to a week; wire electrode displacement occurred even in informed and properly nursed patients. In well-selected patients with dysfunctional voiding, spontaneous micturition often occurred within few hours from electrode placement. In other cases, spontaneous voiding did not occur, and in most of cases, suboptimal nerve stimulation was suspected. PNE revealed in time as a non-reliable tool for the selection of patients. This observation stimulated the research of a more reliable electrode placement to test the patients. Janknegt (1997) suggested the use of surgically implanted permanent electrode to test the patients [14], proposing for the first time a two-stage technique. Permanent electrode was connected through a temporary extension to external screener. The two-stage technique allowed longer stimulation test. The need for open surgery to implant (and to remove, in case of unsuccessful test) permanent electrode represented the main limit of the two-stage technique. The ardent research of a more feasible system to test the patient led to the development of a percutaneously implantable electrode [15], the tined lead system. Since then permanent tined lead electrode was used to test the patient in a two-stage implant. In case of positive follow-up of the first stage, the tined lead is connected to permanent InterStim® device. The flexibility of percutaneous tined lead implant and removal increased the number of tested patients and the percentage of positive results of SNM therapy, especially in the retention group of patients. A first randomized prospective study [16] evaluated PNE technique versus a surgical first stage tined lead placement to better predict whether a patient would progress to an implantation of permanent device. The study was conducted in a cohort of older urge incontinent women; the authors concluded that the first stage procedure using the tined lead electrode better predicted progression to implantable pulse generator placement than PNE in that cohort of patients.
The implant of the InterStim® device (second stage of SNM implant procedure) requires accurate nursing to instruct the patients how to manage their symptoms with implanted device. Since urinary retention may happen again, it is important to train the patient to recognize eventual incomplete voiding or signs of bladder overdistension and to perform intermittent catheterization. Voiding diary is a mandatory tool for nurses to follow up patients immediately after surgery; it becomes a precious tool for the patient to check voided volumes in time. In patients with urinary retention that may be eligible for SNM, strict control of the urinary bladder capacity is essential. Patients with bladder capacities of more than 500 mL often request immediate SNM testing. However, before the SNM evaluation, the regular use of clean intermittent self-catheterization with a 400-mL bladder capacity limit is mandatory to remodel the detrusor muscle as a base for efficacy.
InterStim® device is programmed by an external device to optimize the quality of chronic stimulation. The patient needs to be trained to the use of a personal device (i-Con® patient’s programmer) to communicate with InterStim® device. i-Con® device is a relatively new tool in which utility is conditioned by the quality of training to use it.
12.4.1 Results
A report of the use of SNM in UR was published in 2001 by Jonas et al. [6] in which 177 patients with UR refractory to conservative therapy were enrolled between 1993 and 1998. Thirty-seven patients were assigned to treatment and 31 to the control group. At 6 months the stimulation group showed 69 % elimination of catheterization and an additional 14 % with greater than 50 % reduction in catheter volume per catheterization. Temporary inactivation (3 days) of SNM therapy resulted in significant increase in residual volume. The effectiveness of SNS therapy was sustained for18 months after implantation.
Recently, the 5-year follow-up results of patients included in the trial in order to obtain FDA approval were analyzed. Of 163 patients enrolled, 152 have been implanted. Of the 163 patients, 103 (64 %) had UI, 28 (17 %) UF, and 31 (19 %) UR. Voiding diaries were collected annually over 5 years. In the UR group, the average number of catheterizations per day decreased from 5.3 at baseline to 1.9 at 5 years post implant [17]. However, an important finding in this study is the high correlation between 1- and 5-year success rates. Of the implanted patients, 78 % with UR continued to have a successful outcome at 5-year follow-up, if successful at 1 year.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






