Stimulation group (%)
No treatment group (%)
References
Cured
Improved
Cured
Improved
Weil [28]
9/16 (56)
Not reported (29)
1/22 (5)
0/22 (0)
Schmidt [26]
16/34 (47)
10/34 (29)
0/42 (0)
2/42 (5)
Hassouna [25]
–
22/25 (88)
–
8/25 (32)
Weil et al. [28], Schmidt et al. [26], and Hassouna et al. [25] showed that the daily number of leakage episodes and of pads used was significantly lower 6 months after implantation in the stimulation group compared with baseline. Weil et al. [28] also observed that mean bladder capacity assessed by cystometry increased at 6 months compared with baseline in the stimulation group.
Although evidence from case series studies can be less reliable than evidence from randomized trials, because of the risk of confounding, it is notable that these results are similar to those of the randomized trials. In more than 40 case series studies, about 39 % of patients with urgency urinary incontinence were cured following implantation, and 67 % of patients achieved 50 % or greater improvement in incontinence symptoms [29]. In addition, in the case series studies, the benefits of neuromodulation were reported to persist at follow-up periods 3–5 years after implantation.
Results of persistence of the clinical success in the long term appear to be conflicting. A randomized study [30] suggested some reduction of efficacy with time: a similar proportion (46 %) of patients with urgency urinary incontinence remained dry at 3 years and 6 months after SNM, but only 59 %, as opposed to 87 %, showed greater than 50 % improvement in the number of leakage episodes. Further, a multicenter 5-year prospective trial showed reduction of the number of leakage episodes and pads used in patients with urgency urinary incontinence and decrease in frequency and urgency and increase in mean voided volume per micturition episode in OAB dry patients [31].
By contrast, a 5-year follow-up study [24] on 121 patients with refractory OAB showed persistence of the clinical success in the long term: 84 % of the patients with urgency urinary incontinence and 71 % of the patients with urgency/frequency who had a successful outcome 1 year after implantation continued to have a successfully outcome after 5 years.
The use of SNM may also be recommended for particular populations such as the elderly. Despite age over 55 years and the presence of three or more chronic comorbidities were considered as negative predictive factors for successful outcome with SNM in urinary urge incontinence [32]; in our study [33] on 18 patients over 65 years affected by intractable OAB, 15 women obtained an overall success rate of 83 %. Among all women who underwent implantation of SNM, there was also a statistically significant improvement in the health-related quality of life. No major long-term complications occurred; minor ones happened in two patients (13.3 %) who complained of pain at the pulse generator site; in both cases the event resolved after 3 months using anti-inflammatory treatment. SNM can be considered a viable alternative for treating OAB syndrome in well-selected elderly women.
11.3.2 Quality of Life
Satisfaction and quality of life after SNM have also been studied. Quality of life improvements have been reported in patients with detrusor overactivity, and a strong correlation was identified between the number of incontinence episodes and quality of life index.
Cappellano et al. [34] showed a significant improvement in the quality of life score in patients with urgency urinary incontinence who underwent SNM: at 18 months of follow-up, 90 % of subjects gave a positive response to treatment and 100 % of patients recommended it to a relative or friend. In addition, Foster et al. [35] showed that the majority of patients (84 %) were satisfied with SNM treatment.
11.3.3 Adverse Events
Adverse events associated with SNM implant have been extensively discussed in the literature. A recent study reported an explantation rate of 21 % and a surgical revision rate of 39 % [36]. The most common complications [25, 28, 31] are pain at the implant site (3–42 %), lead migration (1–21 %), wound problems (5–8 %), bowel dysfunction (4–7 %), infection (4–10 %), and pulse generator problems (5 %). The majority of adverse events do not require surgical intervention, but conservative treatment. The introduction of the tined lead and the two-staged procedure have positively affected the adverse event and reoperation rates. Lower incidences of pain (2.5 %), lead migration (0.6 %), and infection (2.5 %) were reported in a follow-up study [37]. Surgical revision was required in 16 % of patients including those with reduced efficacy (10 %) [37]. The learning curve and patient selection may have an additional beneficial effect on the reoperation rates [31].
11.3.4 SNM Versus Botulin Toxin
Studies comparing the effectiveness of the SNM versus BTX have produced conflicting results [15, 31]. A decision analysis model was constructed using values for efficacy and complications from the literature and the personal series. Markov state transition modeling was used with health states and transitions between states designed to fully account for the complex interplay of therapeutic efficacy and multiple possible complications. Overall outcomes and complications for the two operations (SNM vs. BTX injection) were yearly compared (Fig. 11.1), and the probability of success of the SNM was higher than the BTX injection (59 % vs. 48 %, p < 0.05, respectively).
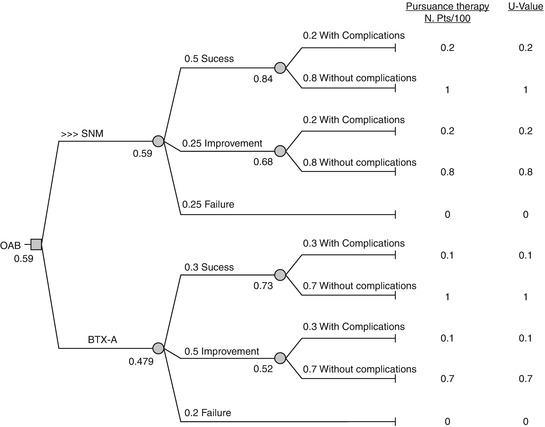
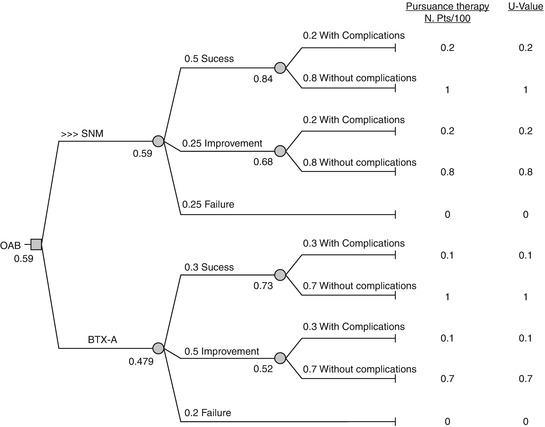
Fig. 11.1
Decision-makers on the clinical benefits between SNM and BTX
11.3.5 Cost-Effectiveness
Few studies have examined the cost-effectiveness of SNM. Siddiqui et al. [38] suggested that SNM treatment strategy was more expensive ($ 15743 vs. $ 4392) but also more effective (1.73 vs. 1.63 quality-adjusted life years – QALYs) than BTX injections in the first 2 years of therapy. However Leong et al. [39] showed that SNM treatment was cost-effective after 5 years compared to BTX injection.
11.4 Conclusions
In conclusion, current evidence supports the short- and long-term efficacy of SNM in treating intractable OAB syndrome, and, in addition, there is a low incidence of adverse events, many of which do not require reoperation. Currently SNM stands as the single licensed second-line treatment for OAB, but more research is needed to improve the selection of patients and the identification of more prognostic factors and to clarify the reduction in effectiveness over time.
References
1.
2.
Irwin DE, Kopp ZS, Agatep B et al (2011) Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int 108:1132–1138PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






