Fig. 13.1
Open surgical approach to the S3 foramen
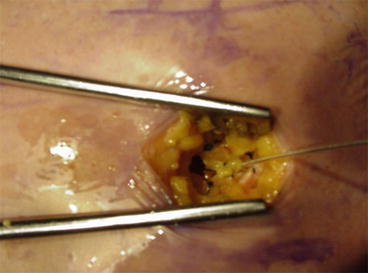
Fig. 13.2
Sacral electrode fixed to the fascia of the gluteus maximum
The procedure was made easier and reliable by Spinelli [13] after the introduction of a tined quadripolar lead (model 3889, Medtronic, USA) provided with special plastic wings to prevent accidental displacements, which can be placed by means of a total percutaneous access with an introducer kit (Fig. 13.3). This method is nowadays used all over the world and, because of the higher reliability compared to the monopolar wire electrode, is used also for the percutaneous nerve evaluation (PNE) temporary testing [14] (Fig. 13.4).
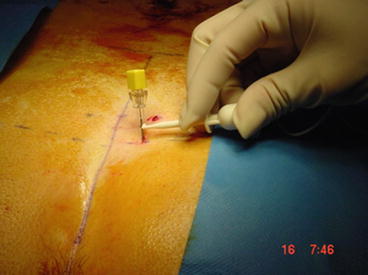

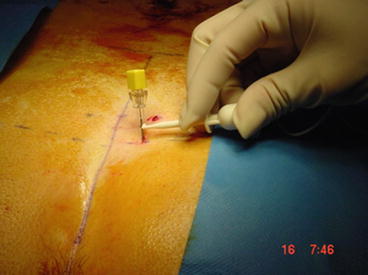
Fig. 13.3
The percutaneous nerve evaluation (PNE) test

Fig. 13.4
Tined lead quadripolar electrode
The traditional screener for the temporary test period was changed with a new patient’s è programmer (mod 3537 Medtronic, USA) (Fig. 13.5) connected via Bluetooth to a new interactive screener which can be programmed by the patient and the doctor (Fig. 13.6).



Fig. 13.5
Verify™ External neurostimulator (mod 3531 Medtronic, USA)

Fig. 13.6
Patient’s programmer (mod 3537, courtesy of Medtronic Inc., USA)
Finally, the implantable pulse generator also was made smaller and thinner (InterStim™ II, model 3889, ©Medtronic, USA, Fig. 13.7) with an easy and simple direct connection to the electrode compared to the earlier model which also needed an extension wire to connect the electrode to the pulse generator. The patient portable programmer (iCon™ model 3037, ©Medtronic USA) was made compact and with an interactive display (Fig. 13.8).



Fig. 13.7
Implantable neurostimulator InterStim II® (mod 3058, courtesy of Medtronic Inc., USA)

Fig. 13.8
Patient’s programmer iCon® (mod 3037, courtesy of Medtronic Inc., USA)
13.4 The Procedure of SNS
The usual approach consists of a two-step procedure which has recently been modified together with the changes of the technical devices.
Nowadays, in most of the centers for SNS, the first step is performed under local anesthesia and short-term antibiotic prophylaxis with the patient in prone position and consists of the percutaneous positioning of the tined quadripolar electrode through one of the S3 foramens previously identified on the skin of the sacral region on the base of some bone landmarkers. The exact lead position is controlled under fluoroscopy and by stimulating a test needle (Fig. 13.3) before placing the electrode, which is then tunneled under the skin and connected, through an extension, to the new Verify™ device. The latter is connected via Bluetooth to the patient’s programmer (model 3537 Medtronic, USA). The stimulation parameters are then optimized according to the patient sensation in the perineum.
During the next 2–3 weeks, the patient will fill in a dedicated stool diary in order to record any episodes of incontinence and to recalculate the scores of incontinence. If at least one of these tools will show at least 50 % improvement, the patient is rescheduled for the definitive implant of the pulse generator (InterStim II, mod. 3889, Medtronic, USA) which will be connected directly to the electrode and placed under the skin of the gluteus region.
13.5 Stimulation Parameters
This aspect of the SNS has poorly been investigated, and there are no trials comparing different parameters, despite the change of voltage, frequency, and pulse width is frequently performed in the follow-up of these patients searching the best combination for success stimulation.
While the pulse width is rarely modified from the default of 210 μs during the follow-up of these patients, the frequency is often changed ranging from 14 to 31 Hz, even if the best combination with other stimulation parameters has never been established. Usually urologists are more prone to use higher frequencies than coloproctologists.
The voltage is normally set to the minimum required to reach the patient sensory threshold because this can spare the battery life and reassure the patient about the active function of the stimulation. Actually, the voltage value is dependent of the proximity of the electrode to the pelvic nerves and of the integrity of the neural pathways.
The only paper dealing with manipulation of the stimulator parameters was carried out on 14 incontinent patients and concluded that short pulse duration (210 μs) and higher frequency (31 Htz) gave the best results in this series [15].
13.6 Outcome Evaluation
Most of the papers on this topic define the success of this therapy with more than 50 % improvement of the incontinence scores (Cleveland Clinic Score [16], St. Marks’ score [17], etc.) and/or at least 50 % reduction of the number of the episodes of major fecal incontinence written down a stool diary sheet in the last 2–4 weeks.
An ad hoc subcommittee of the European Society of Coloproctology has recently discussed the choice of the best incontinence scoring system, and one of the score, which reached the best performance, was the Revised Faecal Incontinence Score by Sansoni et al. [18] where the authors have attempted to improve on the Cleveland Clinic score’s weaknesses. In fact the flatus item was deleted and two other items for urgency and leakage were added. The reliability of this new score was tested showing higher performance compared to the Cleveland Clinic score and the St. Marks’ score.
Another even more important way to evaluate the outcome of this therapy is the measure of the changes in patient’s quality of life. While generic indices like SF36 are not being used anymore because of their poor sensitivity in detecting QoL changes in follow-up after intervention for fecal incontinence, the use of a disease-specific index like FIQL [19] is increasing including its validation in different languages. Another useful and reliable index is the ICIQ B score [20], which combines symptoms and QoL variables, however, is rarely used in studies dealing with fecal incontinence.
13.7 Mechanisms of Action
At the beginning of this therapy, the peripheral effects on the pelvic musculature were believed important, but, although present, the effect of SNS on the anal sphincter tone is inconstant, or irrelevant, insufficient to explain any changes in fecal continence [21–24]. Furthermore, it was demonstrated that the latency between the stimulation and the pelvic muscle contraction was about ten times more than expected as a result of the activation of the reflex arc, indicating that it was the result of a medullary polysynaptic reflex [25].
An effect on rectal compliance and on colorectal motility was hypothesized, but never clearly demonstrated [15, 26].
Several studies carried out in patients with urinary and fecal incontinence using different techniques (PET scan [27], evoked sensory potential [28], and functional magnetic resonance [29]) have demonstrated an activation or inhibition of the central brain areas involved in the control of micturition and continence. Furthermore, the only type of incontinent patients where SNS has never shown to give positive results is the complete spinal patients; on the contrary good results can be achieved even in patients with demonstrated anal sphincter defects indicating that a central, sensory-type effect is more important than any peripheral motility activation.
Finally, a recent study has demonstrated that in most of fecal incontinent patients with long-term successful SNS, the effect is maintained for long term even when the pulse generator has switched off, suggesting that a long-lasting SNS could induce a form of the brain neuroplasticity [30].
13.8 Long-Term Outcome
While the early success rate after SNS for fecal incontinence ranges around 80 % [31–33], its long-term outcome tends to decline with time as for all the other types of treatment for fecal incontinence [34–36]. Few single center [37–41] and multicenter [42, 43] experiences have been carried out looking at the long-term outcome of SNS for fecal incontinence. Taking into consideration the report concerning patients with at least 5 years of permanent implant, the success rate ranges between 89 and 55 %. In this regard, however, it should be emphasized that the success rate is always considered an at least 50 % improvement if the baseline condition, which does not correspond to be cured by fecal incontinence. If the percentage of patients with fully continent after SNS is considered, the success rate ranges between 61 and 36 %.
Finally, there is a debate whether the success rate should be related to the patients selected for SNS (Intention to treat criteria) or just those who succeeded the temporary test and underwent permanent implant of the electrostimulation. Based on the ITT criteria, only 42–54 % of the patients maintained the long-term success [41, 44] and only 26 were cured [44]. Similar results were recently reported on a large series of patients recorded in a European survey [45].
Confirming these results, a total of 57.3 % of the patients offered SNS therapy were satisfied at 4 years follow-up despite their continence status. However, although patient satisfaction was clearly related to the number of FI episodes and patients experiencing full continence were all satisfied, and the satisfaction rate decreased as the number of FI episodes increased, 46 % of the patients with more FI episodes at follow-up than at baseline were still satisfied. In total, 74.7 % of the patients receiving active SNS therapy reported a reduction of ≥50 % in FI episodes, and only 10.3 % of whom were dissatisfied after 4 years of follow up. Therefore, functional outcome of SNS therapy cannot be based only on bowel-habit diaries and bowel scores [46].
In conclusion, although an approximately 10 % loss of effectiveness was demonstrated within 5 years, SNS still appeared to be an effective long-term treatment option. To put this figure into context, most patients seeking treatment for FI can be managed successfully with conservative measures alone; in more than half of the remainder, SNS can provide at least a 50 % improvement in continence maintained into the long term [3].
References
1.
Mellgren A, Wexner SD, Coller JA et al (2011) Long-term efficacy and safety of sacral nerve stimulation for fecal incontinence. Dis Colon Rectum 54:1065–1075PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





