CHAPTER 24 Roux-en-y gastric bypass (linear stapler)
Step 1. Surgical anatomy
♦ Hepatomegaly—large left lateral segment may require division of falciform ligament for optimal hepatic retraction and visualization of gastric pouch.
♦ Ligament of Treitz—ensure proper identification by careful manipulation and verification that the small bowel is attached to the retroperitoneum and passes through the transverse mesocolon.
♦ Where the circular muscular fibers of the esophagus join the oblique fibers of the stomach. Externally, the gastroesophageal fat pad is a consistent identifier of the GE junction.
Step 2. Preoperative considerations
Patient preparation
♦ Bowel preparation consists of a liquid diet the day before surgery.
♦ Prophylaxis for deep venous thrombosis with sequential compression devices and subcutaneous heparin is started before induction with anesthesia.
♦ Intravenous cefazolin (or alternatively clindamycin) is administered prophylactically.
♦ After induction of anesthesia, an orogastric tube and a urinary catheter are placed to decompress the stomach and bladder, respectively.
Equipment and instrumentation
♦ When operating on a morbidly obese patient, it is an obvious and important consideration to have an operating table that is safe for the patient’s weight. The table base needs to support the patient’s weight plus the weight of foot plates in steep reverse Trendelenburg position without tipping. We prefer a hydraulically operated operating room table that can drop low to the ground, which makes it possible for all surgeons and staff to stand on the ground instead of step stools.
♦ An optical trocar is used to access the abdomen once insufflation is obtained with a Veress needle. We prefer this to the open Hassan technique so that we can avoid an umbilical incision, which decreases the risk of hernia formation.
♦ A long 45-degree, 10-mm endoscope allows for optimal visualization of the operative anatomy despite variations in body shapes.
♦ The expandable liver paddle is easily deployed and offers blunt retraction of the left lobe of the liver, even in very large patients.
♦ Additional equipment includes the following:
Room setup and patient positioning
♦ The patient is placed supine on a well-padded operating table. The arms are extended on padded arm boards and secured with padded straps. Foot plates as well as safety straps on the waist and legs are used to ensure secure positioning, especially during steep reverse Trendelenburg position.
♦ The operative surgeon stands on the patient’s right side while the assistant surgeon and camera operator, if available, are on the patient’s left side.
♦ Monitors are placed at the head of the bed near each shoulder.
Step 3. Operative steps
Access and port placement
♦ The abdomen is insufflated using a Veress needle in the left upper quadrant. After adequate carbon dioxide pneumoperitoneum to 15 mmHg, an 11-mm optical trocar is advanced in the same quadrant under laparoscopic visualization using a zero-degree scope. A 45-degree laparoscope is then advanced through the Visiport and used to visualize the peritoneal cavity.
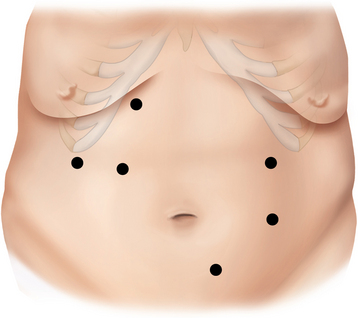
♦ A 10-mm trocar is placed inferolateral to the umbilicus, and the laparoscope is transferred to that position. Two 12-mm and one 5-mm trocars are placed into the right upper quadrant, and a 5-mm trocar is placed lateral to the umbilicus in the left midabdomen (Figure 24-1).
Creation of jejunojejunostomy (J-J)
♦ The transverse colon and omentum are retracted superiorly and the ligament of Treitz identified. The proximal jejunum is divided 50 cm from the ligament of Treitz with a linear stapler (2.5 mm). The mesentery between the two limbs of bowel is taken down using the LigaSure device. The proximal jejunum is the pancreaticobiliary limb, containing secretions from remnant stomach as well as liver and pancreas. The distal jejunum will be brought up to the stomach pouch to contain ingested food and is referred to as the Roux limb or alimentary limb.
♦ The two limbs are joined by a stapled anastomosis after measuring 100 cm distally on the Roux limb. A tacking suture secures the position in preparation for the anastomosis (Figure 24-2).
♦ Adjoining enterotomies are created. A linear stapler (2.5 mm) is fired distally first (Figure 24-3), then rotated counterclockwise and fired proximally (Figure 24-4). The remaining enterotomy is tacked with 2-0 silks for retraction into a linear stapler (2.5 mm). The enterotomy is closed in a transverse direction to minimize potential narrowing. The small bowel mesenteric defect is closed with a running 2-0 silk suture.
♦ To prevent obstruction of the biliopancreatic limb (BP) at jejunojejunostomy, we prefer the 180-degree double fire technique.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree