Fig. 19.1
Patient position and immobilisation for robotic rectal surgery (Lloyd-Davies position)
For right colectomy, the patient is supine with arms tucked by the side. For left colon and rectal surgery, the modified lithotomy position of Lloyd-Davies is used, placing the buttocks at the edge of the table, with the legs in padded Allen stirrups and the hips minimally flexed to allow unrestricted movement of the robotic arms.
19.4.2 Positioning and Peripheral Neuropathy
Obesity increases the risk of postoperative peripheral neuropathy after minimally invasive colon and rectal surgery and is an independent risk factor despite adequate precautions; however, most neuropathy is temporary and self-limited, and the incidence is minimised with our approach as described above [18]. The overall incidence quoted in our paper is 2 % of all minimally invasive colorectal operations and 3.6 % in robotic operations (all were rectal operations performed in lithotomy). An analysis of our data showed that the side towards which the patient is tilted in the transverse plane suffers neurologic damage more frequently, specifically the left-sided nerve axis during right colectomy and the right-sided nerves during left colon operations. The incidence theoretically should be minimised further by differential padding favouring the side towards which the patient is tilted.
19.4.3 Access to the Peritoneal Cavity and Establishment of Pneumoperitoneum
Access to the peritoneal cavity is most rapid and effective in the obese and morbidly obese subjects with the Veress needle. Extra long needles (150 mm) as against the standard 120 mm are occasionally needed in the morbidly obese patient. We insert the Veress through a 2 mm stab incision through or just above the umbilicus after tenting up the tissues with two towel clips. The Palmer’s point represents another site for Veress needle insertion in the morbidly obese as this location has less fat than the periumbilical area in these individuals. Optical trocar systems can also be used; Visiport (Covidien, Norwalk, CT) and Optiview (Ethicon Endo-surgery, Cincinnati, OH) are two FDA-approved commercially available devices which allow safe insertion under vision [19]. In patients who have prior surgeries especially midline incisions, we use the Palmer’s point in the left subcostal region or place the first trocar by the optical method far out in the lateral quadrants. Once entry is established, we use a high-flow thermosufflator (Insuflow, Lexion Medical, St. Paul, MN, USA), which delivers CO2 gas heated to 95 °F and 95 % relative humidity to rapidly establish pneumoperitoneum to 14–15 mmHg. The use of heated and humidified gas prevents hypothermia and tissue desiccation, which translates into less abdominal and shoulder pain [20]. The optical trocar is then placed either by enlarging the initial stab or in the location of choice through a separate incision. The use of two insufflation ports is recommended by bariatric surgeons in morbidly obese patients to maintain pneumoperitoneum, but we have never needed to use this method in our practice. The open Hasson technique is frequently difficult to perform in the morbidly obese, and it is even more difficult to achieve a tight fascial seal around the trocar and is the least preferred entry method in this group in our practice.
19.4.4 Trocar Positioning and Manipulation: Modification of Standard Trocar Position
Obesity alters the normal dimensions of the torso and alters spatial orientation of normal landmarks. Specifically, changes of torso length by 10–11 cm and torso girth by 12–13 cm are reported between underweight and obese patients [21]. Contrary to popular belief, the position of the umbilicus relative to the torso is not fixed. In normal-weight individuals, the umbilicus is located roughly halfway between the xiphoid and the pubic symphysis. With increasing BMI, the umbilicus shifts caudad (Fig. 19.2) [22]. Port positions based on the umbilical location may therefore be erroneous. A good rule of thumb is to use a 5 mm trocar to perform the abdominal survey and then place the additional robotic and assistant trocars under vision at the appropriate distance from the target anatomy rather than through defined premarked sites. When placing lateral ports for right and left colectomy, the ports should be placed at a defined distance usually 10–12 cm lateral to the optical trocar and not far lateral based on patient girth, so as to allow access to the colon on the opposite side. This is because the size of the actual muscular torso does not change much in most obese individuals, and placing the ports too far lateral leads to a tangential entry into the abdomen rather than the perpendicular entry which is desirable (Fig. 19.3a–c).
Fig. 19.2
Caudal shift of the umbilicus with increasing obesity
Fig. 19.3
(a) Correct [purple line] and incorrect [green line] port positions relative to the umbilicus for right colectomy. (b) Representative patient after robotic low APR showing clustering of ports in the middle of the torso representing the right location. (c) CT scan of the same patient showing small [normal torso] size despite morbid obesity with huge pannus
In low anterior resections, the entire trocar setup moves down closer to the pelvis to allow access to the low pelvis and the pelvic floor (Fig. 19.4a, b).
Fig. 19.4
Port positions in a normal (a) and obese individual (b) for robotic low anterior resection [note that ports are closer to the pelvis but are not related to umbilical position which moves caudally in the obese]
Length of the pelvis is also an important consideration and should be assessed in every patient by review of the CT scans. Tall obese males particularly may have a very long pelvis and we have encountered difficulties in reaching the pelvic floor with the robotic instruments with trocars in standard locations. In situations where the instruments don’t reach the lower extremes of the pelvis, the robot is undocked, a fresh set of ports is placed closer to the target anatomy, redocking is performed and the procedure is continued. As experience grows, the trocars should be placed lower in the abdomen, thereby moving closer to the target anatomy.
19.4.5 Robotic Docking
Docking the robot presents some unique challenges in the morbidly obese patient. A steep Trendelenburg position is often used in all colon and rectal operations (except during flexure mobilisation) to use gravity-aided exposure. The increase in abdominal wall fat leads to a massive increase in anteroposterior girth, and the robotic arms may not have sufficient space to clear the wall despite the table being dropped down to the lowest position (Fig. 19.5). A compromise with a slight decrease in head-down tilt with the assistant actively retracting the small bowel out of the field is often needed to physically allow the robot to reach the field. The use of bariatric tables is useful because they allow a much steeper Trendelenburg tilt than with normal tables and their lowest height setting is as low as 25 in. as against the 32 in. standard.


Fig. 19.5
Massive anteroposterior girth in the morbidly obese patient
19.4.6 Creation of the Operative Field and Optimal Exposure
Gravity is the most important aid in exposure in robotic colorectal surgery especially in the obese. The use of steep Trendelenburg and right-down tilt (low anterior resection and left colectomy) or left-down tilt (right colectomy) is indispensable. To allow the small bowel to fall away from the operative area, release of all adhesions is mandatory. The ligament of Treitz is always released for left-sided resections, to allow the small bowel to be packed into the right paracolic and supracolic compartments. Release of the omentum is often needed to allow space for the bowel to be thus placed. The use of radiopaque gauze as a sling over the small bowel to which it adheres is also a useful technique to keep the bowel in place. The fat-laden mesentery is prone to tearing, and it is often prudent to handle the bowel directly or with sweeping motions to deliver it out of the pelvis into the upper abdomen. The use of endoscopic paddles is recommended by some surgeons to retract the small bowel, but we have never found it necessary to do so.
19.4.7 Specimen Extraction and Anastomosis
Obese patients have an increased incidence of wound infections and fascial dehiscence leading to hernias. Careful consideration should be given to specimen extraction site and site for anastomosis when performed extracorporeally. The specimen tends to be bulky due to fat-laden mesocolon, giant epiploica and abundant fatty omentum in right colon specimens.
19.4.7.1 Right Colon
The preferred site for extraction and extracorporeal anastomosis is a supraumbilical incision incorporating the umbilical optical trocar with upward extension for 4–5 cm (adjusted to the specimen bulk). While intracorporeal anastomosis enables an unlimited choice of extraction sites, the benefits of this approach should be weighed against the dangers of manipulating the ileum with a thick friable and fat-laden mesentery with potential for devascularisation and bleeding. We strongly prefer extracorporeal anastomosis, as this is a safer approach given the increased risk of anastomotic leaks in obese patients. Even when extracorporeal anastomosis is planned, intracorporeal vessel ligation is preferable in obese patients; extracorporeal ligation can be remarkably difficult as the thickness of the abdominal pannus makes exteriorisation of the specimen difficult [23]. Obese patients often carry foreshortened mesentery and mesocolon, which are at increased risk of tearing at the time of bowel extraction. The bulky omentum needs to be detached completely before specimen extraction and extracted separately if resected for cancer. The supraumbilical region often has relatively less fat compared to the lower abdomen and is therefore the preferred site for extraction. In a very select group of patients with low visceral obesity, with increasing surgeon experience, the intracorporeal method of reconstruction may be attempted. The Pfannenstiel incision is then the site of extraction.
19.4.7.2 Left Colon and Anterior Resection
For resections in the left colon and downwards, a suprapubic Pfannenstiel incision of 5 cm, placed 2–3 fingerbreadths above the upper border of the pubic symphysis, is our preferred method. The sheath is opened transversely, the muscles split in the midline and the peritoneum opened vertically. A commercially available wound protector (Alexis wound protector, Applied Medical, Rancho Santa Margarita, CA, USA) is placed to allow safe extraction without contaminating the abdominal wound. Our experience shows that the incidence of incisional hernia is nil after a Pfannenstiel incision compared to a 16 % rate for a vertical lower midline extraction site [24].
19.5 Specific Operative Procedures
19.5.1 Robotic Right Hemicolectomy
Conventionally, the robotic technique is ideally suited for medial-to-lateral dissection because its precise nature and dexterity enable the ileocolic pedicle to be skeletonised and dissected right down to the superior mesenteric vessels. In obese patients however the bulky mesocolon and large amount of fat around the pedicle make this approach difficult.
A modified approach: a caudal-to-cranial (inferior-to-superior) approach is safer and more effective. This involves incising the base of the ileocecal fold and allowing pneumodissection. Dissection then proceeds upwards towards the duodenum and laterally along the line of Toldt. In essence the direction of dissection is from inferolateral to superomedial (Fig. 19.6). Once the duodenum and head of the pancreas are separated from the ascending mesocolon, the medial-to-lateral approach can be continued. The ileocecal junction is held upwards by the assistant and the peritoneum on either side of the pedicle is incised and the fat and nodes are swept laterally allowing a secure ligation and division of the ileocolic pedicle at its origin.
Fig. 19.6
Direction of dissection in right hemicolectomy; step 1: inferior to superior, step 2: medial to lateral
It should be noted that the ascending colon in the obese tends to be heavy and is difficult to retract and unfold using only the two robotic working arms. Rather than holding the peritoneal edge for retraction, the entire shaft of the fenestrated grasper should be placed parallel to the mesocolon so that it rests on it, thus enabling retraction of the entire colon and straightening it out (Fig. 19.7).
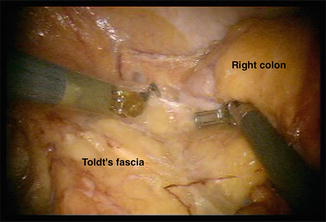
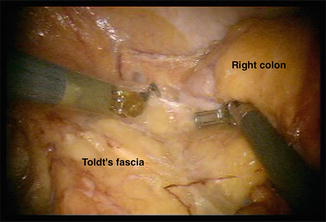
Fig. 19.7
Effective use of instrument shaft for colon retraction in robotic right hemicolectomy
The supracolic dissection is best accomplished with the use of two robotic graspers, a bipolar fenestrated instrument in the left hypochondrial port and a Cadiere forceps in the left iliac fossa port for pulling the transverse colon downwards and the bulky greater omentum upwards. The assistant through the left flank port separates these structures, enters the lesser sac and takes down the hepatic flexure using an energy-sealing device. Our preference is for the Enseal device with straight jaws which functions as an atraumatic grasper, dissector and vessel sealer.
Specimen extraction is facilitated by dividing the terminal ileum intracorporeally using the laparoscopic stapler through the left lower quadrant port. This manoeuvre allows the single limb of bowel to be exteriorised easily through a small supraumbilical incision. Prior to extraction the terminal ileum to be anastomosed should be held with the assistant’s grasper so that it may be easily brought into the wound for anastomosis. Anastomosis is performed in the standard side-to-side functional end-to-end manner. In patients whose mesentery is short and thick, exteriorisation is difficult if not impossible. In this situation, the intracorporeal method using a laparoscopic stapler through one of the robotic ports as has been previously described is extremely useful [25].
19.5.2 Robotic Left Colectomy and Sigmoid Colectomy
Totally robotic approaches to the left colon and sigmoid are commonly performed for malignancy. These are difficult operations to perform due to the need for multiple cart positions, typically by the left shoulder and the left hip and the need for redocking even if a fixed left hip position is used [26, 27]. The one-cart (fit-it-all) position technique is rarely possible due to technical difficulties. The obese patient presents several unique anatomical features that make dissection difficult including:
1.
Bulky, heavy and fat-laden omentum
2.
Adhesions between the sigmoid mesocolon and the small bowel mesentery
3.
Tortuous and heavy sigmoid and descending colon
4.
Obscured origin of the inferior mesenteric artery (IMA) due to visceral fat
5.
Higher chance of damage to the marginal artery due to lack of visualisation consequent to visceral adiposity
6.
Friable peritoneum making it difficult to get a purchase on the specimen
In addition, the current generation of robotic graspers is not well suited to providing a secure but atraumatic hold on a bulky fat-laden mesentery or colon.
All of these make this operation difficult.
One trick is to use an umbilical tape or radiopaque gauze tied tightly around the colon after creating a mesocolic window as a handle, which can be grasped with the robotic graspers and used to manipulate the colon.
The standard approach involving an artery-first approach is modified to a vein-first approach. The inferior mesenteric vein (IMV) is usually not covered by fat, located as it is in the bare area between the middle colic and left colic territories. It is therefore easily visualised even in the most obese individual. Dissection and division of this vein allows access to the proper embryologic interface between Toldt’s fascia and the mesocolon. The left colic artery is then skeletonised and divided [left colectomy] or preserved and used to develop the plane lateral to the superior rectal artery prior to its division [sigmoid colectomy]. Access to both sides of the inferior mesenteric artery (IMA)/superior rectal artery axis also allows visualisation of the autonomic nerves prior to division.
While the presence of large amounts of fat makes the dissection between Toldt’s fascia and the mesocolon relatively easy compared to the patient with a low BMI, there may be considerable difficulty in entering the right plane. A combination of lateral-to-medial and medial-to-lateral approaches is often needed to complete the procedure. The plane is most easily entered cephalad underneath the IMV, and this is an additional advantage of the vein-first approach.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







