Fig. 6.1
The external genitalia of a female affected by bladder exstrophy. The bifid clitoris is seen along with a gap in the pubic hair
As the child grows, the pubic diastasis widens—tending to widen the gap in the levators predisposing to the risk of prolapse and affecting the external appearance of the lower abdomen and genitalia. The midline scar is augmented by the widening and the mons pubis has limited hair growth in the central portion. It is possible to rotate the hair-bearing skin into the midline with a view to improving this appearance. The external genitalia can become distorted with a resulting unacceptable cosmetic appearance.
Revision Genitoplasty in Females
At least 80 % of female patients treated for bladder exstrophy require revision genital surgery [4]. Given that such a high proportion of female patients require revision surgery, routine vaginal assessment at puberty should be undertaken in order to evaluate the potential for further reconstruction. The earlier any potential problems are addressed, the better the chance of normal psychosexual and social development. A common functional complaint is of introital stenosis, inadequate vaginal length or introital stenosis can result in dyspareunia or an inability to have penetrative intercourse. In one series, 32 % of young women underwent revision genitoplasty for this problem alone [5].
Reconstruction Techniques
Revision genital surgery can be utilised either to improve upon an unsatisfactory cosmetic appearance, but this is not essential. Correction of an introital stenosis is the most important reconstructive procedure that is undertaken in these patients.
Monsplasty
Through excision of the midline scar, the non-hair-bearing skin is removed and replaced with hair-bearing skin flaps based inferiorly or laterally that can be rotated together with their underlying fat to cover the defect.
Vulvoplasty
As in monsplasty, the midline scar is excised down to the bifid clitoris; the anterior aspect of the labia can be brought together to form a fourchette. The two clitorides can be joined by approximating the soft tissues without the need for sutures to be directly placed on the clitorides, thus minimising the risk of damage to the neurovascular supply [5]. It is worthy of note, there are no data relating to clitoral sensation following such reconstruction in exstrophy patients.
Vaginoplasty
Due to the presence of a normal calibre vagina above the introital stenosis in pure bladder exstrophy, the majority of patients are suitable for a relatively simple perineal vaginoplasty. Anecdote suggests that very few patients are able to have intercourse without some form of introitoplasty. In exstrophy, a posterior episiotomy vaginoplasty or VY vaginoplasty is often all that is required to open the introitus. In the postoperative period, patients are taught to pass vaginal dilators to reduce the risk of re-stenosis. Other procedures, such as the laying in of a perineal flap, have been described—results are described as being good [5]. Whilst this may have the potential objective of reducing stenosis, this is not clear and sexual function is not detailed in their report.
Pelvic Organ Prolapse
The mean age to uterine prolapse in patients with exstrophy is 16 years [4] with a prevalence of 18 %; this can rise up to 50 % later in life. The prolapse is thought to occur due to the pelvic floor deficiency described above combined with a failure of the bony pelvis to form a complete ring anteriorly. Whilst the early osteotomy was not shown to decrease risk of prolapse, decreased pubic diastasis correlates to lower risk. It remains to be seen whether early mobilisation and reconstruction of the pelvic soft tissues (Kelly procedure) [6, 7] will reduce the incidence of prolapse. The traditionally described pessary treatment is often impossible due to a short vaginal length and the lack of pelvic floor musculature
Numerous techniques have been described for the treatment and prevention of prolapse, including fixing of the uterus to the abdominal wall in childhood [8]. This prophylactic measure proved to be a success and did not complicate pregnancy; however, this technique is not an effective treatment for existing prolapse. Robust long-term evidence regarding the correction of prolapse in the exstrophy population is sparse; a recent consensus suggests that suspension to the sacrum, when present, is likely to give the best results [9]. Various techniques have been described to achieve this, for example, the Gore-Tex® (W.L. Gore and Associates Ltd., Scotland, UK) wrap technique using a length of Gore-Tex® passed through the broad ligaments, around the cervix, and fixed to the sacral promontory. Data have shown a 75 % success rate over a mean follow-up of 8 years have been reported using this technique [10]. The technique of sacral suspension under its varied nomenclature (sacro-colpopexy, hysteropexy, sacrocervicopexy, etc.) is thought to have little or no deleterious effects on fertility; however, it should be deferred until a couple have completed their family. The risk is that during pregnancy or delivery the sacro-colpopexy would be disrupted leading to a recurrence of the prolapse and the need for a repeat procedure in a very complex surgical environment. When treating the prolapse, it is important not to remove the uterus as this not only renders the patient infertile, but is the only structure able to fill the pelvic floor defect. Without the uterus the potential for a large enterocoele exists, the treatment of which can be extremely challenging.
Revision Genitoplasty in Males
Historically, genital reconstruction in male patients was delayed until complete bladder closure or puberty but may now be undertaken with the initial surgery in the neonatal period [11]. Growing up with a normal appearing pendulous penis following reconstruction in the neonatal period has been said to have a positive effect on psychosexual and social development in these boys, the ‘true’ appearance and function of the penis is, however, not clear until puberty [12].
The classic appearance of the penis in a male with exstrophy is of a short (due to short corpora), broad, dorsally tethered penis, an open glans, absent dorsal prepuce, with a dorsal or ventral urethral meatus dependent upon the type and timing of reconstruction in infancy. Many erectile deformities have been described [13], but the majority are a consequence of surgery in infancy where the corpora may have been damaged, only dorsal chordee is an integral part of the exstrophy complex. Asymmetrical corpora are often encountered, where a scarred and fibrotic corpus can compound the deformity (Fig. 6.2).


Fig. 6.2
An example of the dorsal chordee described. This may be as a result of skin tethering or urethral length restriction. A butterfly needle needs placing in both corpora to achieve an artificial erection as there is no cross-circulation
Assessment of Deformity
Before embarking upon reconstructive surgery, it is important to gain a good understanding of current function in terms of sensation, erectile function, ability to orgasm and ejaculate, and the presence of chordee or deformity that may or may not affect function. Establishing whether a deformity precludes penetrative intercourse or is purely a cosmetic problem is relevant, but both factors can be equally as important to patients. Dorsal chordee is a common finding in adolescent and adult men with exstrophy—this may be simple skin tethering, or depending on the reconstruction, the urethra may be the tether. In considering reconstruction, it may be necessary to relocate the urethral meatus. It then becomes important to consider future urethral function, i.e. if the bladder neck is closed and the urethra is to act solely as a seminal conduit, then if the meatus needs to be located in a proximal or hypospadic location it will have to stay there—further attempts to terminalise a ‘dry’ urethra will be unsuccessful with a high risk of stricture. If the patient is voiding urethrally or catheterising, further urethral reconstruction may be of benefit. The cosmetic appearance of the penis can be a major concern to the patient and should be considered carefully alongside function. An objective anatomical assessment can be made by performing an examination under anaesthetic with artificial erection.
Reconstruction Techniques
The aims of genital reconstruction in the male exstrophy patient are to provide a penis that is symmetrical and straight enough for penetration with normal sensation and good erectile function. Urethral function is important—in our series 70 % had undergone urinary diversion [14]; therefore, the urethra is dry and acting only as a conduit for seminal fluid. If the bladder neck has been reconstructed and the patient is continent but either voiding or catheterising urethrally, the management of the adolescent and adult patient will be different. Cosmesis is important—patients will often raise concerns about this. The details below will discuss what is achievable and those factors that may limit the reconstructive options. This should be achieved without compromising sensation or erectile function; this in itself can be challenging due to the positioning of the neurovascular bundles. The location of the bundles may vary considerably depending upon previous reconstruction; the unpredictability of their position renders them vulnerable during further surgery [15] (Fig. 6.3).
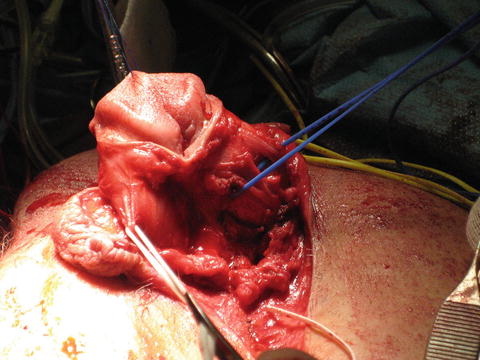
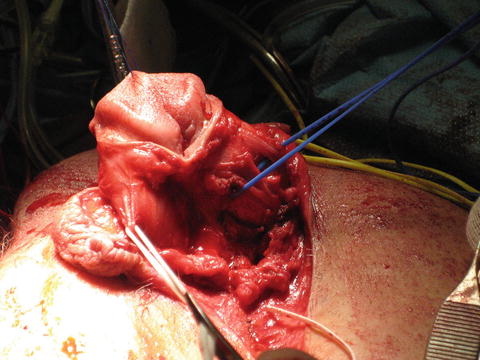
Fig. 6.3
Dissected exstrophy penis with the neurovascular bundles identified
Length
The corpora in men with exstrophy are 60 % shorter than normal corpora [16], and there are no buried corpora in the pelvis that can be utilised to increase true length. There is often asymmetry with one corpus scarred and fibrotic as a result of early surgery. Functional length may be improved by maximising exposure of the existing corpora; this can be achieved by releasing any corporal attachments to the body of the pubis and/or freeing of scar tissue that may be tethering the corpora. The former of these techniques does carry a risk of devascularising the corpora, especially if attempted in childhood [17]. An exstrophy penis can be reconstructed by complete disassembly—separating both corpora and as there is no cross-circulation between the two. In reconstruction, corporal tucks will straighten curvature and rotation either in or out of the corpora may improve length. In addition to these techniques, radial artery-free flap phalloplasty can be performed; this was first reported by de Fontaine et al. in 2001 with reasonable functional and cosmetic results [18]. Although it may be technically possible to perform a phalloplasty, this should be reserved for a patient whose penile anatomy or function prevents penetrative intercourse despite exploring the above penis-conserving techniques.
Chordee
The simplest form of correction of dorsal chordee is release of any scar tissue causing tethering using a VY or Z plasty technique. Correction of the corpora can either be achieved by shortening the convexity or lengthening, the concavity, or a combination of the two.
In shortening the convexity, some shortening of penile length is to be expected; the advantage of this method is that the urethra need not be disturbed. This is usually achieved by placing plication sutures in the corpora and has the advantage of requiring minimal dissection and little risk of damage to the neurovascular bundles; the clear disadvantage is the loss of length in an already short penis. In undertaking this type of surgery, the potential for complete disassembly needs to be available, and there may be a need to relocate the urethral meatus further proximally on the penile shaft. If this is a dry, seminal conduit, it should remain here. If it is used for urethral voiding, a further two-stage reconstruction may be possible. The issue of shortening and loss of sensation needs to be discussed during consent, but if there is a fixed dorsal chordee this needs correction in order to achieve any functional length.
In lengthening of the concavity, the corpora are incised transversely and closed longitudinally, ideally to each other after rotating the corpora towards each other (the Cantwell–Ransley technique [19]). When using this technique, good apposition needs to be achieved; if the corpora are spread too far apart and apposition is not optimal, a new hourglass deformity can result. If the urethra is functional, complete, and dorsal, lengthening the concavity can result in apparent urethral shortening that requires urethroplasty to correct. In addition to Ransley’s modification of Cantwell’s technique first described in 1895 [20], various other methods for epispadias repair and correction of chordee have been published. Techniques such as those described by Mitchell [21] and Kelly [22] both involve complete penile disassembly with subsequent anatomical reconstruction. In Mitchell’s procedure, the penis is divided into two separate hemicorporeal glanular bodies and a separate urethral plate. The advantage of this technique is that it does not require mobilisation of the neurovascular bundles or corporotomy, but does allow anatomical reconstruction of the penis with correction of rotational deformity and of chordee. The associated morbidity and necessity of these more invasive and complex procedures should be carefully considered when selecting the best reconstructive options [16].
Sexual Function and Fertility
The beginning of relationships and sexual function become important to all during adolescence. It is normal for any adolescent to question their function in relation to this and for many there will be moments or periods of insecurity. This is part of normal development. It is also normal to ask how a congenital anomaly and the treatment of it, including surgery, will affect sexual function. There is often a significant focus on cosmesis and in the case of a male patient penile size. In exstrophy, the bony diastasis may lead to a significant dip in the skin and a midline separation of the pubic hair. The long-term management issues with respect to sexual function have not been extensively studied but disorders or anxiety surrounding sexual function in adolescence can have a significant psychological impact on patients. Reports suggest that some 1/4–1/2 of patients are dissatisfied with penile length or chordee [16]. Libido in exstrophy patients is normal and they form normal relationships; in the author’s experience a key component in sexual function is the partner’s understanding and acceptance of the patient’s reconstructive history. In a society where casual sexual encounters are more common, this can create a pressure on these patients. A desire on their part to conform to the behaviour of their peer group is met with a fear that a new partner may not understand their condition and rejection may result. The treating urologist needs to be aware of this background and prepared to manage it. A multidisciplinary approach, including psychosexual counselling and support, should be adopted as discussing and addressing issues around sexual function can be challenging for both the patient and clinicians.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





