and Christopher Isles2
(1)
Institute of Cardiovascular and Medical Sciences, University of Glasgow, Glasgow, UK
(2)
Dumfries and Galloway Royal Infirmary, Dumfries, UK
Q1 When should a patient be considered for a renal transplant?
Renal transplants have been shown to improve survival and quality of life in patients who are under 75 years of age. This is not to say that patients over 75 will not benefit, simply that no evidence exists of a survival advantage. Older patients are certainly at more risk of having a heart attack or stroke at the time of their surgery or shortly afterwards. Risks and benefits should be considered carefully in all age groups.
Q2 What different types of renal transplant are there?
Cadaveric transplantation remains most common and still accounts for around two thirds of all transplants, though living donor transplantation is increasing. Simultaneous pancreas-kidney transplants are a treatment option for patients with kidney failure and type 1 (but not type 2) diabetes. Pre-emptive transplantation means receiving a kidney before starting dialysis. Altruistic donation is the giving of a kidney from a living person to a friend or to a stranger. The different types of transplant are summarised in Fig. 39.1
Fig. 39.1
Categories of renal transplantation
Q3 What is meant by donation after brain death (DBD)?
Donation after brain death is also known as heart beating kidney donation. The typical donor is a patient with a significant brain injury requiring life support by ventilation in whom brain stem death has been confirmed by the following criteria:
Box 39.1 Criteria for Brain Stem Death
No pupil reflexes.
No corneal reflex.
No nystagmus when ice cold water is run into each ear.
No response to painful stimulus.
No gag reflex.
No attempt to breathe unaided when the ventilator is switched off and the PaCO2 is allowed to rise over 6.5 kPa at a time when the patient continues to receive oxygen.
The incidence of brain stem death is declining year on year due to tighter road safety regulations. In clinical practice the brain stem death tests are conducted by two doctors on two separate occasions usually 10 or 15 min apart. Neither doctor should have anything to do with the transplantation. Sedatives should be withdrawn for 24 h before conducting brain stem death tests. Once brain stem death has been established, the patient is taken to theatre and the kidneys are removed while the heart is still beating, before complications occur. Complications of brain stem death include hypotension, diabetes insipidus, DIC and arrhythmia.
Q4 What is meant by donation after cardiac death (DCD)?
Donation after cardiac death is also known as non-heart beating kidney donation. This is an altogether more difficult area. The doctors looking after the patient, who will invariably be in the intensive care unit, need to separate discussion about futility from discussion about organ donation. There is then a 2 h window after stopping therapy during which retrieval of a viable kidney is possible, provided the patient dies during that time. Not all patients in whom active treatment is withdrawn will die and not all of those who do die will do so within 2 h.
Q5 How is consent obtained from the relatives?
In the UK the relatives still have the right of veto even if the patient has carried a donor card. In order to donate a kidney, the family must ‘opt in’. Many doctors believe more kidneys would be donated if patients were asked to ‘opt out’ instead ie it is assumed they will donate their kidneys unless they have specifically signed a register to say they will not do so. For the time being the opt-in system remains in place in the UK.
Q6 How are cadaveric organs allocated?
By blood group and tissue typing. Donors and recipients should be blood group and tissue type compatible. The four blood groups are A, B, AB and O and the way in which the matching works is as follows:
Box 39.2 ABO Compatibilities
A can receive from A or O.
B can receive from B or O.
AB can receive from anybody.
O can only receive from O.
Patients are also tissue typed by their HLA (Human Leukocyte Antigen) antigens. We use three of these for tissue typing: the A, B and DR antigens. Each of us has 2 A, 2 B and 2 DR antigens, one from each parent. The best tissue matches are A, B and DR identical. This is referred to as an OOO mismatch. Mismatches for the A and B antigens are not as important as mismatches on the DR antigen. Fewer mismatches allow for a lower dose of immunosuppressant drugs and a lower risk of acute rejection. In addition, a better match lowers the risk that the patient will develop antibodies to the donor antigens (donor specific antibodies) – a phenomenon which could increase the chances of rejection and also make future transplants more difficult.
Q7 What written information is a transplant surgeon likely to give a patient before adding their name to the waiting list?
Having established that the patient is likely to benefit from a renal transplant the surgeon will explain that the waiting time can be 3–4 years if the patient has to wait for a cadaveric transplant. He/she will then discuss surgery and how the kidney is placed superficially in the left or right iliac fossa with blood vessels plumbed into the iliac vessels and the donor ureter into the recipient bladder. There will be a ureteric stent at the time of surgery and this will remain in place for approximately 6 weeks in order to hold the ureteric surgical suture line open until it has fully healed (Fig. 39.2).
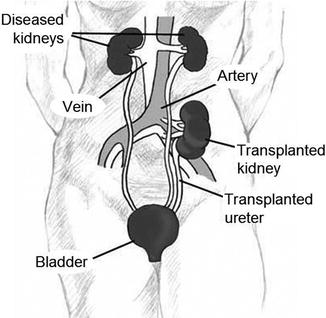
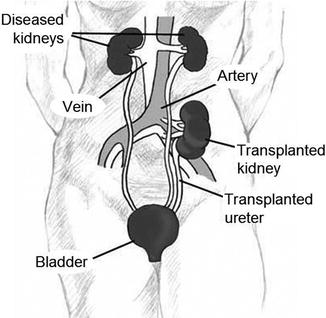
Fig. 39.2
Placement of renal transplant
Patients can expect to be in hospital for at least a week and in some cases several weeks depending on how long the transplant kidney takes to work. Living kidneys usually start to work immediately but a cadaveric kidney can take several days or even weeks (Fig. 39.3). Patients will be told that at least 90 % of grafts will be working at 1 year, and that 50 % will still be working at 10 and 15-years following cadaveric and living donor kidney transplants respectively.
Fig. 39.3
Intra-operative urine production
The reasons for failure of a transplant will also be discussed. Less than 1 % of kidneys will never work and a similar number will fail early on due to blood clot. The surgeon will discuss the mechanisms of rejection and how repeated episodes of rejection can damage the kidney. It will also be mentioned that some of the medication used to prevent rejection, particularly ciclosporin and tacrolimus, can in the long term fur up the small blood vessels within the kidney and cause it to fail. Patients must accept these risks before proceeding to transplantation.
Q8 Name the immunosuppressive drugs that are commonly used to prevent rejection?
Box 39.3 Commonly Used Immuosuppresive Drugs
Prednisolone.
Mycophenolate mofetil/ azathioprine
Tacrolimus/ciclosporin
Nearly all patients will receive initial triple therapy with prednisolone, mycophenolate and tacrolimus. Mycophenolate is an anti-proliferative drug and tacrolimus a calcineurin inhibitor (CNI). They are more potent, more modern and more expensive than their predecessors azathioprine and ciclosporin respectively. Occasionally a dose reduction or drug switch to one of the less common immunosuppressant drugs is necessary if a patient develops an unacceptable drug side effect (eg switch to sirolimus in a patient with recurrent skin malignancy).
Q9 Discuss the side effects of the immunosuppressive drugs.
The main risk is that of infection, not only in the perioperative period, but for the duration of immunosuppression ie the life of the transplant (see Q11 below). There are in addition some drug specific side effects (Box 39.4).
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








