RENAL HANDLING OF POTASSIUM
Potassium is a primarily intracellular ion, with skeletal muscle alone containing more than 75% of the body’s total load. Less than 2% of this load is found in the extracellular fluid. The normal plasma concentration is between 3.5 and 5.0 mmol/L.
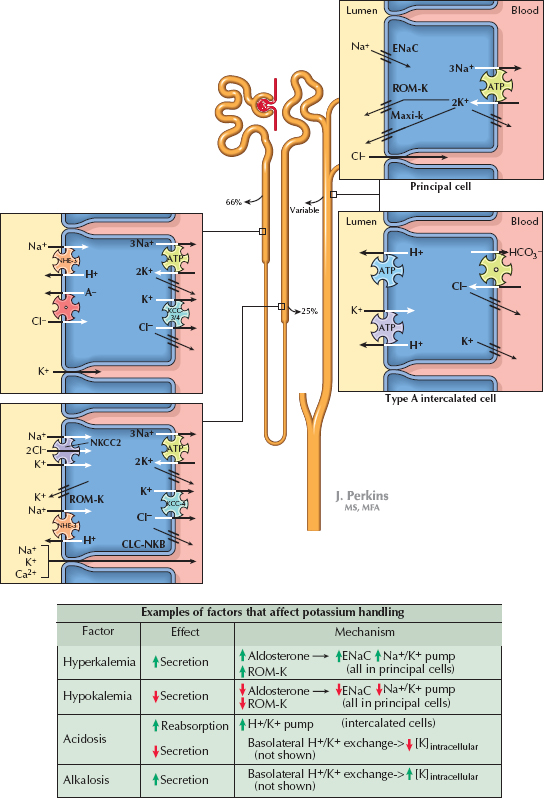
Extracellular potassium is freely filtered at the glomerulus. A large fraction of the filtered load is consistently reabsorbed along the proximal tubule (66%) and loop of Henle (25%). In the distal tubule, however, there is a variable degree of reabsorption or secretion that depends on input from homeostatic feedback mechanisms. In this manner, the kidneys make a crucial contribution to the regulation of the plasma potassium concentration.
TRANSPORT MECHANISMS
Proximal Tubule. In the proximal tubule, potassium is reabsorbed along a paracellular route. A chemical gradient is established as the reabsorption of sodium and water concentrates potassium in the tubular fluid. An electrical gradient is established as chloride is reabsorbed, which leaves a positive charge in the late part of the proximal tubule. There is some evidence that potassium also undergoes some transcellular reabsorption in this segment, but the details and relative importance of this pathway remain unknown.
Thick Ascending Limb. In the thick ascending limb, potassium undergoes transcellular reabsorption by crossing the apical membrane on the Na+/K+/2Cl−cotransporter (NKCC2), then crossing the basolateral plasma membrane via KCC4 K+/Cl− symporters and potassium channels. A subset of the potassium that enters the cells, however, is recycled back into the lumen through ROM-K channels. Such recycling creates a positive charge in the lumen that drives the paracellular reabsorption of potassium, sodium, and other cations.
Distal Nephron. Potassium handling is more variable from the distal convoluted tubule onward, with overall excretion rates depending on the net balance of secretion and reabsorption.
Secretion occurs primarily in the connecting tubule and cortical collecting duct. When sodium enters principal cells through apical ENaC channels, a negative charge is left in the tubular lumen. An electrical gradient thus established, potassium that has been brought into principal cells on basolateral Na+/K+ ATPases flows into the lumen through apical ROM-K and maxi-K (also known as BK) channels. K+ channels are also present in the basolateral compartment, as they are elsewhere in the nephron, to permit continuous operation of Na+/K+ ATPases.
Reabsorption occurs primarily in the outer medullary collecting duct. Type A intercalated cells possess apical H+/K+ antiport ATPases, which bring potassium into cells, and basolateral K+ channels, which allow it to enter the interstitium.
REGULATION OF POTASSIUM EXCRETION
Hyperkalemia promotes the release of aldosterone from the adrenal cortex, which up-regulates apical ENaC and basolateral Na+/K+ ATPases in principal cells. The resulting increase in sodium reabsorption enhances the electrical gradient for potassium secretion. Hyperkalemia also causes direct, aldosterone-independent stimulation of ENaC and ROM-K channels in principal cells, further enhancing potassium secretion.
Hypokalemia, in contrast, suppresses aldosterone release and down-regulates apical ROM-K channels in principal cells, thereby reducing potassium secretion. In addition, hypokalemia enhances expression of apical H /K ATPases in type A intercalated cells, promoting potassium reabsorption.
Acid-base disturbances also alter potassium secretion or reabsorption, largely because of basolateral H /K exchange. In acidosis, protons enter cells to be buffered, and potassium ions exit cells to maintain electroneutrality. The reduction in intracellular potassium levels decreases the chemical gradient for secretion into the tubules. In alkalosis, in contrast, protons exit cells, causing a rise in intracellular potassium levels that promotes secretion.
Finally, volume status has an important relationship with potassium handling. In volume contraction, AII promotes release of aldosterone, which enhances potassium secretion. In volume expansion, increased flow rates through the nephron stimulate greater potassium secretion through maxi-K channels. Thus potassium secretion is ensured during both volume expanded and contracted states.
< div class='tao-gold-member'>




