Fig. 11.1
Ia-APR specimen

Fig. 11.2
Defect following Ia-APR. Notice that the entire posterior wall of the vagina has been removed
With this procedure, there is an extensive tissue loss of the levator plate and the perineum within an irradiated field.
In these cases we always reconstruct the perineum with a vertical rectus abdominis myocutaneous flap (VRAM), to cover the defect in the pelvic floor and perineum. This flap is large and bulky and has a safe blood supply to the skin and subcutaneous tissue.
Generally the VRAM flap has been harvested from the right site of the abdominal wall. If there is a transverse incision on the right site of the abdominal wall, we perform Doppler ultrasonography to document that the inferior epigastric arteries are patent, since the flap is depending on its blood supply (Figs. 11.3 and 11.4).
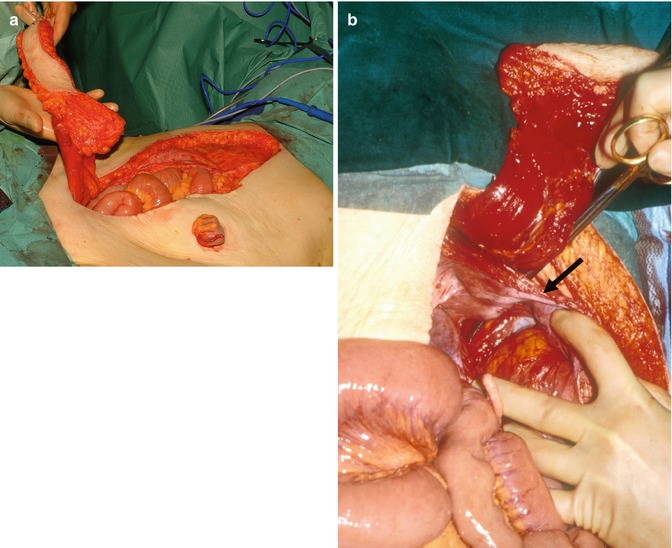

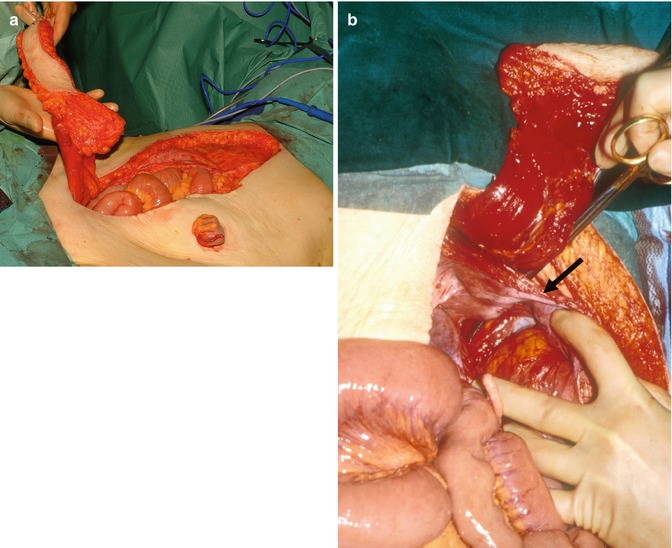
Fig. 11.3
(a) VRAM flap harvest. The flap includes skin paddle, subcutaneous fat, a cuff of anterior rectus sheath fascia and one rectus abdominis muscle. (b) The rectus sheath is divided caudally to the pubic bone raised on inferior epigastric artery (arrow) serving as the vascular pedicle for the VRAM flap

Fig. 11.4
The large VRAM flap inserted for reconstruction of the posterior vaginal wall and perineum
The harvest of flap and the perineal reconstruction have always been performed by a dedicated plastic surgeon. The VRAM flap has several advantages:
1.
The muscular part can cover catheters in the pelvic cavity and thereby protect the small bowel against irradiation damage if postoperative brachytherapy is used.
2.
It can be used for reconstruction of the vagina.
3.
It can cover a large defect in the perineum. In cases where there is very extensive loss of skin, the peripheral part can be left open and secondarily repaired by a split skin transplant.
4.
The reported primary healing rate of the perineum is very high, and in a consecutive series of Ia-APR for anal cancer salvage surgery, no perineal surgical intervention was needed in 49 cases [21].
The main drawback of this flap is that it prolongs the operation time and that a plastic surgeon has to be involved.
Furthermore, there are some donor site morbidities with herniation.
The flap is denervated and this might lead to atrophy of the muscle and sensory disturbances of the skin.
An alternative would be the use of one or two myocutaneous gluteal flaps, but we have never used it in these cases due to our good results with the VRAM flap (Fig. 11.5).


Fig. 11.5
Use of a Permacol mesh for reconstruction of the pelvic floor following E-APR
Conclusion
I would recommend standardised APR procedures.
For In-APR no pelvic floor reconstruction is needed.
Following E-APR we prefer a mesh reconstruction, but an alternative might be a myocutaneous gluteal flap. Randomised studies are needed to document which procedure is best and whether a biological mesh has an advantage.
In the author’s experience, the VRAM flap is the method of choice when extensive defects of the perineum have to be repaired.






