Fig. 20.1
Patient draped and positioned with the perineum parallel to the floor
20.4 Surgical Technique
An inverted horseshoe incision is made with clearance of the anal verge by roughly 2 cm all round. A curved Lowsley retractor is passed down the urethra into the bladder. The incision is roughly square shaped with rounding of the edges. This gives a broad based flap and has been found to have less of an incidence of midline wound break down due to ischemia with retraction of the skin margins.
Following the development of the ischio-rectal fossa the central tendon is identified and a finger passed beneath the central muscle/tendon anterior to the rectal wall and the central tendon divided allowing the rectum to drop away, opening the approach to the prostate. Following the division of the central tendon, the space either side of the central tendon is developed exposing the anterior rectal wall and the recto-urethralis muscle which is placed on stretch by double gloving and placing the index finger of the left hand (right handed surgeon) through the anus and retracting directly posteriorly towards the floor. The central tendon is then cut back with sharp dissection (this is usually an avascular structure and provided it is thinned out and only the tendon is cut). Within two to three centimeters back the midline space opens up and the prostate can usually be visualized in the depths of the incision. The two lateral wings of remaining muscle either side of the central tendon are divided a short way back, but not as far as the central tendon. These muscular structures are continuous with the layer in which the neuro-vascular bundle is housed and it is felt that by not cutting them back against the prostate that the neuro-vascular bundle is afforded some protection (see Fig. 20.2).
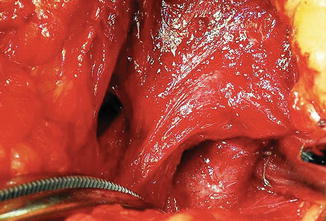
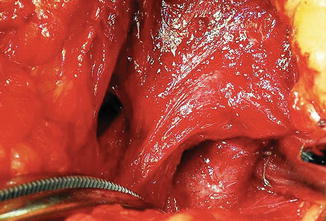
Fig. 20.2
Exposure of the urethra under the neuro-vascular bundles
The down side of this is that the visualization of the prostate is slightly more limited. It has been our policy over the last 8 years not to use any instrumentation for retraction as this places the nerve bundles on stretch and although it may improve the visualisation of the prostate for the surgeon, it is usually not necessary with the instruments we use. I find it very useful to use two small stainless steel pediatric spatula (1 and 1.5 cm wide) which can be bent and hooked in behind the neuro-vascular bundles to gently retract these off the prostate while the connections with the prostate are divided with or without small liga-clips on visible blood vessels. The urethral prostatic junction is then cleaned and the length of urethra below the sphincter exposed. A right angle Mieke or Lahey clamp passed behind the urethra between the urethra and the dorsal vena complex, gently opened to separate the dorsal complex off the urethra and the urethra is then divided against the Lowsley retractor. The retractor is withdrawn and a holding suture placed through the urethra before it is totally divided (Fig. 20.3). A long Ellis clamp placed in the urethral opening into the prostate allows the prostate to be manipulated and the dorsal venous complex to be gently shifted back towards the bladder neck. The alternative is the placement of straight Lowsley retractor into the bladder which then can be used to manipulate the prostate and also to clearly delineate the vesico-prostatic junction. This is recommended in the early learning phase of one’s surgical experience. Hereafter the plane is developed between the prostate and the bladder by cutting down at 90° with a right-angled scissors opening the bladder neck area and visualizing the internal surface of the bladder. This automatically creates two lateral pedicles between the bladder and the prostate, which can then be clipped and sharply divided or cut with a Harmonic scalpel. The tissue lateral to the seminal vesicles represents the vascular pedicles which are clipped and divided. The prostate is lifted and approached from the posterior aspect with division of Denonvilliers and the anterior rectal fascia covering the posterior aspect of the prostate. This fascia and with it the rectum can then be gently swept off the vesicles, allowing the rectum to drop away out of harm’s way. The seminal vesicles can either be dissected out completely or truncated, clipped and divided. We seldom remove more than two-thirds of the vesicles as we believe if there is infiltration beyond this point, the surgery becomes a non-curative procedure and the risk of disturbing the vesical nerve plexus at the apex of the vesicle does not justify the wide dissection posterior to the bladder. We perform a circumferential bladder neck frozen section biopsy to establish a clear bladder neck margins particularly in patients with suspected T4 cancer infiltrating the bladder neck. We routinely use a posterior racket handle reconstruction, and don’t believe preservation of the bladder neck plays a major role in the regaining of urinary incontinence. Sutures are placed after visualizing the ureters and progressed from the 6 o’ clock position towards 12 o’ clock. After two to three stitches have been placed, a running 4-O monocryl suture everts the mucosal lining from 12 to 4 o’clock and 12 to 8 o’clock. An 18 French Biocath urethral catheter is then passed and the anastomotic sutures in the urethra placed at 1, 11, 5, 7, 3 and 9 o’clock positions. The 3 o’clock and 9 o’clock sutures are placed at a later stage once the racket handle has been completed and the urethral opening closed to the required caliber from posterior. The urethral-vesical anastomosis is then carried out under direct vision (this is one of the big advantages of the perineal approach) and once completed can be inspected and additional sutures placed to stabilize the anastomosis. The rectal wall is the checked for any possible injuries. The wound is irrigated and checked for any residual bleeding from the lateral pedicles. The wound is closed in layers with zero absorbable glycolic acid fat sutures with an 8 mm pencil drain in the right lower corner of the wound, caprosyn sutures in the vertical arms of the suture and a 4-O V-lock suture sub-cuticularly along the apex of the wound. The legs are then lowered and the patient, after leaving the operating room, is returned to the post-surgical ward and depending on the facilities, either to a general surgical ward or to a high care ward [2, 18, 19].
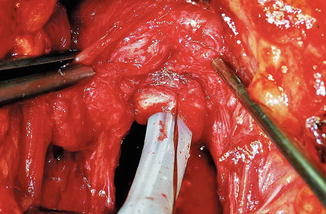
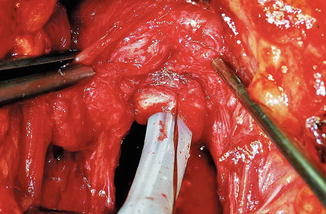
Fig. 20.3
Divided urethra with a Foley catheter in place (tagged with suture) between the neuro-vascular bundles. The limited space available working between the neurovascular fascia is visible
Lymphadenectomy
In the high risk patients, Gleason 7 or higher, PSA above 15 and clinical T3 cancers, or patients with suspected seminal vesicle infiltration, a pre-radical prostatectomy mini laparotomy is done through a 5 cm suprapubic incision and frozen sections is done on the lymph nodes. Although it is very rare that in a patient who otherwise qualifies for a radical prostatectomy due to clinical organ confined disease and acceptable risk profile, would be disqualified due to bulky nodal disease and this is done mainly as a staging procedure. It is done under the same anesthetic and adds roughly 30 min to the surgery.
20.5 Post-operative Management
Patients can usually start eating and drinking immediately as there is no abdominal wound in the majority of cases (even with a small extraperitoneal mini-lap incision). The risk of deep vein thrombosis is extremely low because the legs are at a higher level than the heart during the time of the entire procedure, the patient is still covered with prophylactic anti-coagulation with low molecular weigh heparins and elasticated stockings for the first few days of the hospital stay and in high-risk patients the first 14 days following their surgery.
The patients are mobilized and resume normal diet on day 1 and encouraged to walk actively. Emphasis is placed on wound care and keeping the wound dry especially the apical part of the incision in the midline raphae which can, because of its poor blood supply, sometimes show slight delayed healing. Since using the sub-cuticular V-lock suture over the last 2–3 years, we have seen very few problems in this area. An oral stool softener (not a laxative) is given daily until the first bowel movement. The patients are usually discharged on the second or third post-operative day once they have had their first bowel movement. It is important allow the patient access to the surgeon/nurse practitioner if he has any concerns about wound infection, pain control, bowel activity etc. The Foley-catheter is usually removed between 10 and 14 days depending on the size of the patient, the ease of the surgery and the general confidence level of the surgeon following the procedure with regards to the vesico-urethral anastomosis. We now seldom do a retrograde urethrogram/cystogram prior to removing a catheter, unless concerned in very obese patients for example, about the integrity of the anastomosis.
20.6 Complications and Their Management
Overall the peri-operative variables show the safety of the perineal approach (Table 20.1) The risk of peri-operative of complications is low as summarized in our series of over 1,700 cases (Table 20.2). The incidence of rectal injury in our combined series of 1,786 patients over a 17 year period is 0.003 %. Two of these patients had a loop colostomy for 6 weeks. The others were repaired primarily during the operation and recovered uneventfully. This is well below the quoted incidence of 1 % and significantly below the 4 % incidence reported by Bishoff et al. [20]. Rectal injuries not recognized at the time of surgery usually require a loop diverting colostomy for 6–8 weeks. Important is to confirm closure of the fistula prior to the closing of the colostomy. Those injuries recognized intra-operatively are closed in two layers using absorbable sutures. Anal stretch and a period of bowel rest with antibiotic cover followed by a low residue diet for a week allows the majority of these injuries to heal without incident.
Table 20.1
Peri-operative variables after 1,764 consecutive
Variable | Result (mean and range) |
|---|---|
Age | Mean 61 years (42–78) |
PSA | Mean 8 ng/ml (0.2–37) |
Operative time
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





