Radiation Injury
Radiation injury causes two types of gastrointestinal damage. The first is the radiation damage itself; the second is the long-term consequence of radiation (i.e., ischemic changes or cancer development). Even though the colon and rectum are relatively radioresistant, they have a high incidence of radiation damage due to both the large radiation doses used to treat tumors arising in the pelvic area and the fixed position of the sigmoid colon. Many patients receiving radiotherapy also receive drugs with radiosensitizing effects. These drugs are directly toxic to the mucosa, predisposing it to further radiation damage. Between 75% and 90% of all intestinal complications affect the distal colon (177), with the rectum being most commonly involved (178,179).
Recent evidence suggests that microvascular endothelial apoptosis represents the primary lesion in gastrointestinal radiation damage (180,181). A single large dose of radiation preferentially damages the endothelial cells and epithelial cells die following the endothelial damage. The pathophysiology of radiation injury is discussed in detail in Chapter 6.
About 75% of patients develop clinical symptoms, usually by the middle of the second week of therapy. These include diarrhea, a mucoid discharge, tenesmus, abdominal distention, and abdominal pain. Mucosal edema, duskiness, and loss of the normal vascular pattern develop. Severe proctosigmoiditis follows radiation therapy in 2.4% to 5% of
patients; it is more common in patients treated with >6,000 rads over 6 weeks. Diffuse pancolitis may develop, as may ulcerations, stenosis, necrosis, and fistulas, all caused by progressive intramural vasculitis with submucosal and subserosal fibrosis. Delayed lesions include strictures, perforation, intestinal pseudo-obstruction, vascular obliteration, and mural fibrosis. Delayed proctosigmoiditis with intermittent bleeding of mild to moderate severity occurs 6 months to 5 years following therapy but can be delayed for as many as 30 years.
patients; it is more common in patients treated with >6,000 rads over 6 weeks. Diffuse pancolitis may develop, as may ulcerations, stenosis, necrosis, and fistulas, all caused by progressive intramural vasculitis with submucosal and subserosal fibrosis. Delayed lesions include strictures, perforation, intestinal pseudo-obstruction, vascular obliteration, and mural fibrosis. Delayed proctosigmoiditis with intermittent bleeding of mild to moderate severity occurs 6 months to 5 years following therapy but can be delayed for as many as 30 years.
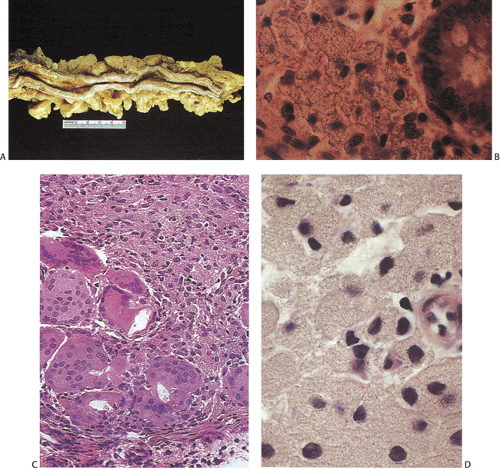
Early colorectal changes include mucosal edema (Fig. 13.91), mucosal discoloration or duskiness, and loss of the normal mucosal vascular patterns. Pallor, loss of mucosal folds, and irregular shallow ulcers, fistulae, and abscesses may also be present. Chronic radiation-induced colitis often manifests as strictures that may be long or short and generally have tapered and smooth margins.
During acute injury, characteristic changes usually remain confined to the mucosa. They include crypt cell damage, crypt abscesses, inflammatory cell infiltrates, nuclear
atypia, reduced mitotic activity, loss of nuclear polarity, crypt loss, and mucosal sloughing. Eosinophils are often prominent (Fig. 13.92). Other acute effects consist of prominent submucosal edema often with a myxoid appearance, ulcers, inflammatory polyps, mucosal telangiectasia, and sometimes ischemia. There may be glandular proliferation with mild cellular atypia. The changes may simulate dysplasia. Most of the changes resolve within a month, although mild atrophy and inflammatory cells may remain and be present at 3 months following treatment cessation (182), but they eventually regress.
atypia, reduced mitotic activity, loss of nuclear polarity, crypt loss, and mucosal sloughing. Eosinophils are often prominent (Fig. 13.92). Other acute effects consist of prominent submucosal edema often with a myxoid appearance, ulcers, inflammatory polyps, mucosal telangiectasia, and sometimes ischemia. There may be glandular proliferation with mild cellular atypia. The changes may simulate dysplasia. Most of the changes resolve within a month, although mild atrophy and inflammatory cells may remain and be present at 3 months following treatment cessation (182), but they eventually regress.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree