Fig. 4.1
Postoperative photograph of patient’s abdomen at 6 months after single-port laparoscopic adrenalectomy. The patient has had excellent cosmetic results at postoperative follow-up
Single-port laparoscopic cholecystectomy was first attempted in the 1990s [4, 5]; however, it has not enjoyed widespread use to date. Recently, SPLS has experienced renewed interest and has developed as an extension of the standard laparoscopic, minimally invasive procedures. SPLS has the potential to provide patients with improved cosmesis, decreased pain, and higher satisfaction with having a single-wound [6–11]. SPLS obviates the need to space ports externally for triangulation, thus allowing for the creation of a small, solitary portal of entry into the abdomen. However, many laparoscopic surgeons have already tried, and found, the technique challenging. Additionally, questions remain regarding the safety of the procedure, real benefits, and the ideal patient population for these new techniques. Recently, reports of a reduced port laparoscopic surgery (RPLS), a hybrid operation of SPLS and conventional laparoscopic surgery, are increasing because of the better feasibility and safety than SPLS [12–15]. In this chapter, we will summarize the pros and cons of RPLS.
4.2 Indications and Contraindications
Although the benefits of SPLS over conventional MPLS have not been clearly elucidated, worldwide use of the technique is constantly increasing. Currently, the feasibility of SPLS or RPLS has been demonstrated in a clinical setting for almost every type of gastroenterological surgery. At experienced laparoscopic centers, results equivalent to those of conventional MPLS have been documented for many SPLS or RPLS procedures, including general, gastroenterological, urologic, gynecologic, and other abdominally-related surgeries [16–22].
The indications, contraindications, and preoperative preparation for SPLS and RPLS are almost identical to those for MPLS. SPLS is a challenging operation for even experienced laparoscopic surgeons. The newer SPLS procedure may someday be equally efficacious and feasible as MPLS in high-volume centers [23]. However, patients with risk factors such as previous abdominal surgery, history of severe or on-going inflammation, and obesity were thought to have a higher incidence of conversion to MPLS or open surgery [24].
From our own experience, cholecystectomy for non-inflamed gallbladder, partial gastrectomy for gastric gastrointestinal stromal tumors (GISTs) located anterior or on the greater curvature, appendectomy, or inguinal hernia repair were the ideal indications for SPLS when compared to MPLS [6]. Alternatively, adrenalectomy [10, 25, 26], the Heller–Dor procedure [8], Nissen fundoplication [27, 28], liver resection [29, 30], and colectomy [31–33] were indications for RPLS and were equally feasible for experienced laparoscopic surgeons in terms of perioperative and postoperative parameters compared with MPLS. Splenectomy for patients with splenomegaly remains challenging, even for laparoscopic surgeons in high-volume centers [34, 35]. The major problems were spleen retraction and the control of excessive bleeding. Additionally, obese patients may not always be suitable candidates for the SPLS technique.
4.3 Knack of Surgical Technique
Access to the abdominal cavity in SPLS and RPLS should follow accepted standards for safe entry, including avoidance and recognition of complications. The introduction of new instruments, access devices, or new techniques should be done with caution and under a study protocol. Prior to its use, any new instrument or device should be proven safe to the fullest extent possible. Adequate training should also be provided. During initial procedures, a low threshold for using additional ports should be maintained so as not to jeopardize a safe dissection and result [23].
Access into the peritoneal cavity to achieve SPLS or RPLS has not been standardized. We believe that a multichannel port is advantageous, and we support this approach over multiple ports through a single-incision. A multichannel port is beneficial in that it minimizes air leaks, promotes safe insertions, enables insertion of curved instruments, provides a wider insertion point for instruments, and has better triangulation. Based on our experience, a reduced port approach using the multichannel port, plus one puncture or port, also makes it possible to triangulate even with standard instruments to ensure immediate control of any bleeding site, if necessary (Fig. 4.2).


Fig. 4.2
Reduced port laparoscopic splenectomy. The patient was placed in the right semilateral position. GelPoint (Applied Medical, Rancho Santa Margarita, CA, USA) and 12 mm port were used for patient with splenomegaly
Needlescopic-assisted SPLS is a variation of SPLS. In advanced SPLS, we typically use a multichannel port and an additional “needle-like” 2–3 mm instrument (Figs. 4.3 and 4.4). Needlescopic instruments reduce the main limitation of SPLS, that is, the lack of instrument triangulation. Their assistance can prevent a conversion of the procedure to a conventional MPLS when failure to progress is noted. Moreover, they can significantly reduce operating time. Additionally, needlescopic-assisted SPLS could be considered as an approach that diminishes the steep learning curve of pure SPLS, as it resembles conventional MPLS. Needlescopic assistance does not negate at all the cosmetic outcome, which is still considered the main advantage of SPLS over MPLS.
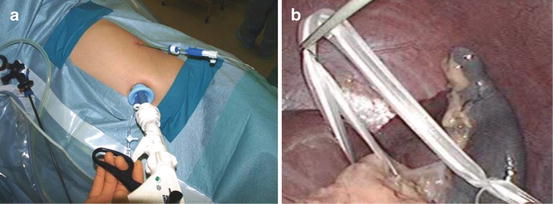
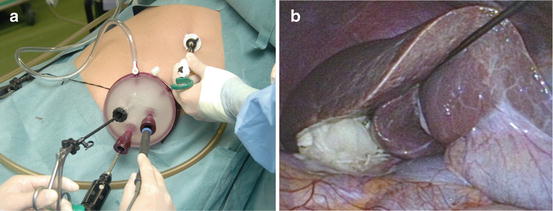
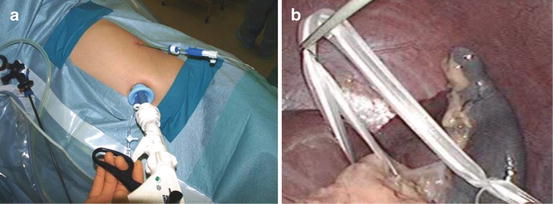
Fig. 4.3
Needlescopic-assisted single-port laparoscopic splenectomy. (a) The patient was placed in the right semilateral position. SILSTM port (Covidien, New Haven, CT, USA) and mini-loop retractor (Covidien) were used for idiopathic thrombocytopenic purpura. (b) The spleen was gently lifted up using a loop-shaped 4-mm Penrose drain, with traction supplied by a mini-loop retractor inserted from below the costal margin on the left midclavicular line
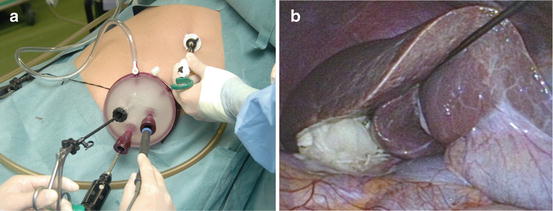
Fig. 4.4
Needlescopic-assisted single-port laparoscopic right adrenalectomy. (a) The patient was placed in the left semilateral position. GelPoint and MiniLap (Stryker, Kalamazoo, MI, USA) were used for primary aldosteronism. (b) The right liver lobe was evaluated using a MiniLap and small gauze, providing good visualization of the operative field surrounding the right adrenal gland
4.4 Tips and Tricks
Many important benefits of laparoscopic surgery result from preserving the integrity of the abdominal wall, including decreased operative trauma and complications, and improved cosmesis. For many operations, several attempts have been made to reduce operative trauma further by decreasing the number and size of the ports used in the procedure. The use of three ports instead of four, and the use of needlescopic instruments, is definitely a step in this direction. The use of a flexible scope, an articulating instrument, and a needlescopic instrument, along with standardization of the procedure, greatly reduces the “learning curve” for the procedure. Based on our experience, surgeons became familiar with both the technique and visualization of single-port laparoscopic cholecystectomy after about 20 cases. Other investigators have reported a similar learning curve in operating times for initial cases when single-port laparoscopic access was used [24, 36]. However, one of the concerns with SPLS and RPLS is that they are inherently one-operating-surgeon techniques. This may have a negative impact on resident education and the training of future surgeons. A formal course with collaborative learning, video simulations, “hands on” education with instrumentation, and in-operating room reservation would shorten the learning curve for new adopters.
In SPLS or RPLS, the control of bleeding is as important as it is in MPLS. Excessive bleeding must be dealt with and controlled immediately. While conversion may immediately lead to a conversion to an MPLS or open procedure, this is not a necessity. Controlling bleeding with a gauze compression or a grasper provides temporary control. Surgeons should not extend the damage by indiscriminately applying clips.
4.5 Recommendations for RPLS
RPLS is a safe and technically feasible procedure for patients with diseases of a general, gastroenterological, urologic or gynecologic fields. RPLS also offers cosmetic benefits and the potential for postoperative pain reduction. However, inexperienced surgeons performing SPLS should understand that the use of needlescopic instruments does not negate the cosmetic results for difficult cases. Additionally, obese patients may not always be suitable candidates for pure SPLS techniques. We should consider needlescopic-assisted SPLS as a valuable tool to employ whenever organ retraction or instrument triangulation for suturing is necessary.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








