Chapter 48 PREGNANCY AND LIVER DISEASE
ABNORMAL LIVER FUNCTION TESTS IN PREGNANCY
Determine the stage of pregnancy, and whether there is anything in the history to indicate a liver disorder. A pregnancy-related liver disorder should be considered in the event of any relevant past history, or history of medications or in the presence of features of pre-eclampsia.
NORMAL PHYSIOLOGICAL CHANGES IN PREGNANCY
Normal physiological changes in pregnancy are shown in Table 48.1. The mother’s blood volume increases by 40%, and her total body water increases by 20%. This is reflected in a 10%–60% fall in serum albumin and also a fall in haemoglobin. Up to 50% of women develop spider naevi and palmar erythema during pregnancy, which is thought to be due to the increasing levels of oestrogen. This reverses quickly post delivery. Serum alkaline phosphatase increases 2–4-fold in the third trimester (placental) and gamma-glutamyltranspeptidase decreases slightly. No change is observed in the aminotransferases (alanine aminotransferase and aspartate aminotransferase) or the prothrombin time. A rise in the transaminases should lead to further investigation.
TABLE 48.1 Normal changes in liver function tests during pregnancy
| Blood test | Change during pregnancy |
|---|---|
| Alkaline phosphatase | Increases 2–4-fold (placenta) |
| Gamma-glutamyl transpeptidase | No change or slightly decreases |
| Aspartate aminotransferase | No change |
| Alanine aminotransferase | No change |
| Bilirubin | No change or slightly increases |
| Bile salts | No change |
| Albumin | Decreases by 10%–60% |
| Globulin | Increases |
| Caeruloplasmin | Increases |
| Prothrombin time | No change |
| Cholesterol | 2-fold increase |
| Triglycerides | 2–3-fold increase |
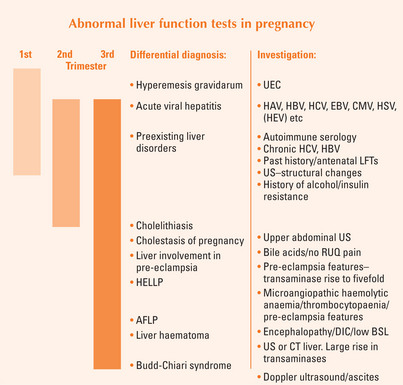
Up to 3% of pregnancies are complicated by abnormal LFTs at term. The best guide in determining the cause of abnormal LFTs is the timing of the problem during pregnancy (Figure 48.1). The differential diagnoses include:
Pregnancy is associated with an increased rate of gallstone formation. Hence cholecystitis and cholelithiasis need to be excluded in any pregnant woman presenting with right upper quadrant pain, nausea and abnormal LFTs. The differential diagnosis of right upper quadrant pain (Table 48.5) in late pregnancy includes pregnancy-related liver problems, such as liver involvement in pre-eclampsia, even hepatic infarction or rupture. It should be remembered that the gravid uterus pushes up the appendix, and appendicitis in late pregnancy can present with right upper quadrant pain.
TABLE 48.5 Differential diagnosis for right upper quadrant pain in the third trimester of pregnancy
| Diagnosis | Incidence during pregnancy |
| Pyelonephritis | 1%–2% |
| Cholelithiasis/cholecystitis | 3%–5% have biliary sludge |
| Acute appendicitis | 1/1500 |
| Pancreatitis | 1/1439 |
| AFLP | 1/10,000–1/15,000 |
| Pre-eclampsia + liver involvement | <1% |
| HELLP syndrome | 0.1% |
| Hepatic haematoma/rupture | 1/45,000 |
| Acute viral hepatitis | Same as in the general population |
| Acute Budd-Chiari syndrome | Rare |
AFLP = Acute fatty liver of pregnancy; HELLP = haemolysis elevated liver enzymes and low platelet syndrome.
LIVER DISEASES UNIQUE TO PREGNANCY
Cholestasis of pregnancy
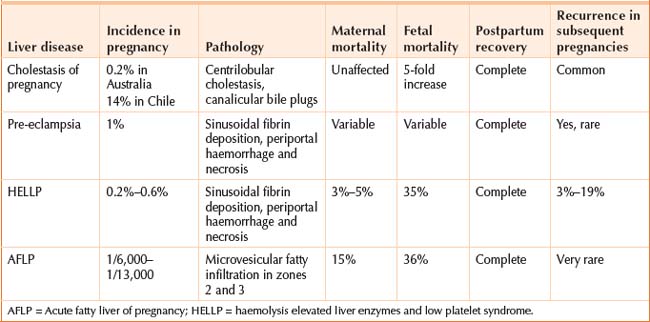
Cholestasis of pregnancy is the most common liver disease unique to pregnancy. The incidence is about 1/500 pregnancies (0.2%) in Australia. A higher prevalence is seen in Scandinavia and South America (14% risk in Chile). The condition is characterised by pruritus, and an increase in the serum bile acid, and is usually seen in the third trimester. Women present with an itch, without any skin lesions (apart from scratch marks). There may be a history of mothers or sisters with the same problem, and it may have occurred in previous pregnancies. The itch normally goes within days after delivery.
Risks to the baby
There is a five-fold increase in the risk of preterm labour and stillbirth. Fetal monitoring does not predict the babies at risk, as there is no problem with placental blood flow. The fetal risk is not understood; high bile acids appear toxic to the baby, and cause myometrial irritability. When the total bile acids are 40 μmol/L or greater, fetal complications can occur. Women with this condition will usually have an induced delivery at 38 weeks, to decrease the fetal risk.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree