Fig. 10.1
Preoperative upper endoscopy: dilated and tortuous esophagus
Fig. 10.2
Preoperative esophagram: retained contrast column and narrowing at the esophagogastric junction (EGJ)
Fig. 10.3
Preoperative HRIM showing elevated integrated relaxation pressure (IRP) and panesophageal pressurization consistent with type II achalasia
10.2 Operation
10.2.1 Patient Preparation and Operative Setup
Prior to surgery, the patient was kept on a clear liquid diet for 48 h and completed a 5-day course of oral nystatin for Candida prophylaxis.
The patient was positioned supine with the right arm abducted and the left arm tucked at the side, with the abdomen prepped in case needle decompression was required for the presence of capnoperitoneum (Fig. 10.4). The POEM was performed under general anesthesia with endotracheal intubation and skeletal muscle paralysis. Special care was taken at the time of anesthesia induction and endotracheal intubation to prevent aspiration.


Fig. 10.4
Operative setup
10.2.2 Operative Procedure
Step 1
Initial endoscopy
Initial endoscopy was performed using a single-channel, high-definition gastroscope with CO2 insufflation. The air insufflation was confirmed to be turned off. The esophagus and stomach were aspirated of any retained fluid and food, the stomach was desufflated, and the esophageal body was examined for Candida or stasis esophagitis. The endoscope was then fitted with an oblique transparent cap (longer end of bevel posterior) and the distance from the squamo-columnar junction to the incisors was measured on the scope shaft (Fig. 10.5).


Fig. 10.5
Initial endoscopy showed a narrow EGJ. The endoscope was fitted with an oblique transparent cap, and the location of the squamo-columnar junction was measured on the endoscope shaft
Step 2
Mucosotomy and entry into the submucosal space
A submucosal bleb was created in the esophageal wall 12 cm proximal to the esophagogastric junction (EGJ) at the 1 o’clock position, using a sclerotherapy needle containing a solution of 0.9 % saline, 10 mL of indigo carmine (0.2 mg/mL), and dilute epinephrine (5 μg/mL) (Fig. 10.6). An endoscopic cautery knife was used to create a 2-cm longitudinal mucosotomy over the submucosal bleb (Fig. 10.7). The submucosal areolar tissue was cleared to expose the circular muscle layer. The endoscope was then bluntly maneuvered into the submucosal space, utilizing the oblique scope cap.



Fig. 10.6
Submucosal bleb created with a solution of saline, indigo carmine, and dilute epinephrine

Fig. 10.7
Longitudinal mucosotomy performed by electrocautery over the submucosal bleb
Step 3
Creation of the submucosal tunnel
Creation of the anterior submucosal tunnel required a combination of electrocautery (Fig. 10.8) and hydrodissection using a solution of saline and indigo carmine without epinephrine (Fig. 10.9). The orientation was checked periodically by evaluating the meniscus of injected fluid within the tunnel. The tunnel was extended 3 cm distal to the EGJ. Narrowing of the submucosal tunnel and the appearance of palisading vessels and aberrant muscle bundles (Fig. 10.10), as well as markings of the shaft of the endoscope, signified transition to the EGJ. The patient’s systolic blood pressure was kept under 120 mmHg to avoid bleeding during progression of the submucosal tunnel. The epinephrine-containing solution was used again in the distal portion of the tunnel. After completion of the submucosal tunnel (Fig. 10.11), the scope was withdrawn from the tunnel and advanced through the esophageal body to the gastric lumen. Blanching of the gastric cardia mucosa, seen upon retroflexion, was recognized as a sign of extension of the submucosal tunnel onto the stomach (Fig. 10.12).
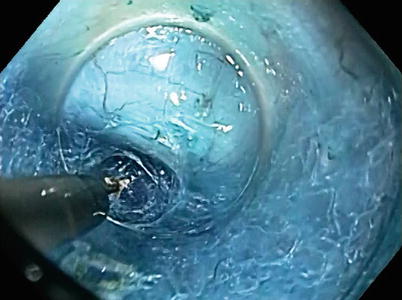
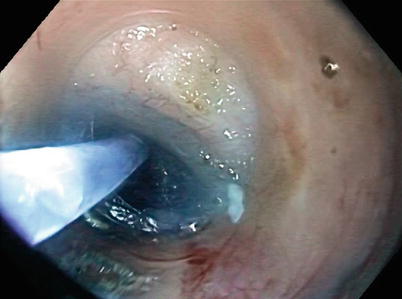

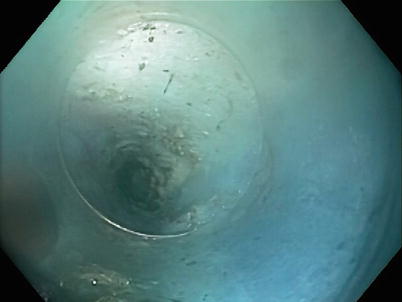
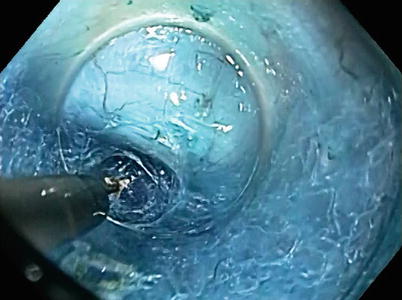
Fig. 10.8
Division of the submucosal tissue using electrocautery. The circular muscle layer can be seen in the background
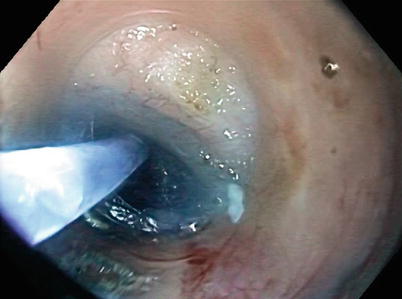
Fig. 10.9
Hydrodissection with saline and indigo carmine solution during the creation of the submucosal tunnel

Fig. 10.10
Submucosal tunnel appearance approaching the EGJ, including palisading vessels (red arrow) and oblique muscle-fiber bundles (black arrow)
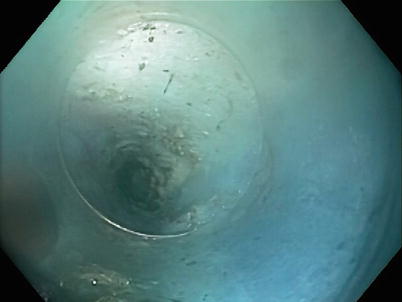
Fig. 10.11
Inside view of completed submucosal tunnel
Fig. 10.12




(a) Mucosal blanching after submucosal tunnel extension onto the stomach. (b) Blanching of the gastric cardiac mucosa seen upon retroflexion at the end of the submucosal tunnel creation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








