CHAPTER 52 Peptic Ulcer Disease
Decades of research focused on the role of acid secretion and the effects of stress, personality type, and genetics in the pathogenesis of ulcer disease. The discovery of histamine-2 (H2) receptors1 and development of H2-receptor antagonist drugs, and the subsequent development of proton pump inhibitor drugs led to major changes in the management of peptic ulcer disease. The discovery of H. pylori and its treatment led to dramatic changes in the prevalence and recurrence of peptic ulcer disease, transforming peptic ulcer from a chronic recurrent disease to a curable one.2 H. pylori infection remains an important cause of peptic ulceration in the developing world. In the developed world, the use of NSAIDs has emerged as a leading cause of peptic ulcer disease, especially in the aging population in whom these drugs are often prescribed. Through all of these developments, the role of acid and pepsin in the genesis and perpetuation of mucosal injury remains a unifying aspect of the pathogenesis of peptic ulcer disease.
EPIDEMIOLOGY
The epidemiology of peptic ulcer disease has undergone a remarkable change in the past century. The incidence of duodenal ulcer and gastric ulcer has declined in parallel with the decline in H. pylori prevalence, likely as a result of improved sanitary conditions and a safer food and water supply. The risk of developing peptic ulcer disease and the risk of dying from peptic ulcer disease increased in successive cohorts born between 1840 and 1890 and then declined thereafter.3 A peak in the incidence of gastric ulcer in the first half of the 19th century and a subsequent peak in the incidence of duodenal ulcer in the second half of the 19th century remain unexplained, although a number of theories have been proposed, among them the widespread adoption of smoking after the commercial manufacture of cigarettes in a setting of widespread H. pylori infection.
POPULATION-BASED STUDIES
In northern Sweden, a random sample of 1001 people underwent upper GI endoscopy after filling out symptom questionnaires.4 The prevalence of peptic ulcer disease in this sample was 4.1%, with 20 gastric ulcers and 21 duodenal ulcers. In a prospective Danish study of 2416 subjects, the 11-year cumulative incidence of peptic ulcer was 2.9%: 1.6% for duodenal ulcer, 1.3% for gastric ulcer, and 0.04% for combined ulcers.5 In countries with a high prevalence of H. pylori infection, the ratio between duodenal and gastric ulcers may be quite different. In a case-control study from Shanghai, China, in which the prevalence of H. pylori infection was 76%, recurrent or new peptic ulcers occurred in 3.6% of the population over 2 years and 85% of the ulcers were duodenal.6
TIME TRENDS
There has been a significant decline in mortality from peptic ulcer disease over time in most age groups.7,8 A notable exception is older adults, in whom peptic ulcer bleeding remains a life-threatening condition. A study based on the U.S. National Discharge survey reported that from 1992 to 1999, the annual rate of hospitalization for peptic ulcer disease declined 20%, from 205/100,000 population to 165/100,000 population. Mortality also declined 22%, from 7.7/100,000 to 6/100,000, respectively. Sales of acid-inhibitory drugs correlated with a decrease in peptic ulcer disease hospitalizations and mortality,9 although this correlation does not prove causality. The observed decline in ulcer-related mortality was probably related to improvements in the general health of the population and the availability of effective treatment for peptic ulcer disease.
In an analysis of the Canadian Institute of Health Information database, the prevalence of acute nonvariceal upper GI bleeding (largely ulcer-related bleeding) declined by 31%, from 77/100,000 population to 53/100,000 population over the 10-year period from 1993 to 2003.10 The need for surgical intervention also declined but the mortality rate remained unchanged. In the United Kingdom, overall hospital admission rates for peptic ulcer disease have also declined, as has mortality, but admission rates for peptic ulcer hemorrhage and perforation have increased.11 Peptic ulcer bleeding is most often seen in older adults, with 68% of patients presenting older than age 60, and 27% older than age 80.12
RISK FACTORS
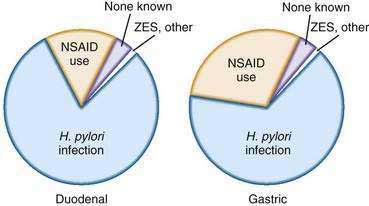
The principal risk factors of peptic ulcer disease are H. pylori infection and NSAID use (Fig. 52-1). However, some patients with peptic ulcer disease have neither of these risk factors.
HELICOBACTER PYLORI INFECTION (see Chapter 50)
H. pylori is a gram-negative bacillus that is uniquely adapted to life in the stomach. It is a major cause of peptic ulcer disease and accounts for a large proportion of peptic ulcers in countries where H. pylori infection is highly prevalent such as in Asia. In the United States and in western Europe, the original estimates that H. pylori infection was the cause of 90% or more of duodenal ulcers, and 60% or more of all gastric ulcers have been lowered by the declining prevalence of H. pylori infection.13 It is estimated that close to 70% of duodenal ulcers are related to H. pylori in Western populations. For example, in an analysis of patients who participated in H. pylori eradication trials in the United States, the proportion of patients with peptic ulcer disease and H. pylori infection was 73%.14 In Rochester, New York, the prevalence of H. pylori infection in patients with duodenal ulcer disease was 61%.15
ASPIRIN AND NONSTEROIDAL ANTI-INFLAMMATORY DRUGS (see also Chapter 51)
Aspirin is increasingly used in the prevention of cardiovascular disease.16,17 Aspirin and clopidogrel are frequently used in combination in patients who have had ischemic cardiac events or in patients who have recently had a stent placed in the coronary arteries.18 NSAIDs are used by approximately 11% of the U.S. population on a regular basis.19 This frequency is likely to increase as the population ages. Regular use of NSAIDs increases the odds of gastrointestinal bleeding five- to six-fold compared with persons not taking NSAIDs.20 Serious ulcer-related complications occur in 1% to 4% of NSAID users and NSAID-related complications are thought to account for 100,000 admissions every year.21 NSAID users who also take aspirin are at an especially high risk for complications. In a population-based study from Denmark, the odds ratio for GI bleeding if a person was taking low-dose aspirin was 2.6, and this risk increased to 5.6 in patients who were also taking an NSAID.22 In Spain, the death rate attributed to NSAID-aspirin use was 15.3/100,000. Up to one third of all NSAID-aspirin–related deaths in that study were attributable to low-dose aspirin use.23
H. pylori and NSAIDs may have a synergistic role in causing peptic ulcer disease. In a meta-analysis, the odds ratios for the development of a peptic ulcer in patients with H. pylori infection or NSAID use were 4.05 and 2.99, respectively, but the odds ratio increased significantly to 15.4 if both factors were present.24 The risk factors for peptic ulcer disease among patients taking NSAIDS and their risk ratios are listed in the next chapter (see Table 53-1).
OTHER ULCEROGENIC DRUGS
Deep ulcers and perforations of the stomach and duodenum have been described in cocaine and methamphetamine users, presumably due to mucosal ischemia.25 Bisphosphonates have also been associated with gastroduodenal ulceration,26 although esophageal injury with bisphosphonates in clinically more of a concern (see Chapter 45). There is little if any risk for peptic ulcer disease in patients taking glucocorticoids.27 In combination with NSAIDS, however, glucocorticoids increase the risk of peptic ulcer disease above the risk with NSAIDs alone.28
OTHER RISK FACTORS
Smoking has been implicated in the pathogenesis of peptic ulcer disease for decades, but its importance as a risk factor has declined after the discovery of H. pylori. A population-based study evaluated the risk factors for peptic ulcer disease in 2416 Danish adults who were interviewed between 1982 and 1994.29 As expected, H. pylori seropositivity was a significant risk factor for ulcer disease; smoking increased the risk of peptic ulcer only in H. pylori–infected subjects. A large body of literature suggests that smoking may predispose to peptic ulcer disease, but H. pylori infection remains a confounder that was not addressed in earlier studies. It is noteworthy that cigarette smoking does not increase the risk of recurrent ulceration once H. pylori has been eradicated, suggesting that smoking may only play a role in infected subjects.30
The role of alcohol remains uncertain. Alcoholic beverages stimulate gastric acid production. Moreover, direct application of high concentrations of alcohol to the gastric mucosa causes demonstrable mucosal injury. In the Danish study alluded to previously,29 intake of spirits increased the risk of peptic ulcer disease in H. pylori–infected patients.
With regard to diet, ulcer prevalence rates differ considerably in the north of India, where the principal cereal in the diet is wheat, and in the south, where rice is the predominant cereal. However, many other potential confounders were not accounted for in these populations.31 An association between the ingestion of spicy foods and peptic ulcer disease is weak, at best.32
Emotional stress was proposed as a major cause of ulcer disease or as a precipitant of ulcer complications,33 and much was written about its relationship to peptic ulcer disease prior to the description of H. pylori. Personality types and psychological profiles have been proposed to be linked to ulcer, but much of this literature is confounded by the lack of information on H. pylori infection. Well-documented descriptions of an increase in ulcer disease after natural calamities such as earthquakes suggest that emotional stress among those not physically injured may play a role in triggering overt manifestations of peptic ulcer disease, especially in individuals who may be otherwise predisposed to ulcer (e.g., patients infected with H. pylori).33,34
PATHOGENESIS
GASTRIC ACID SECRETION
Gastric acid and pepsin have long been considered the principal inciting agents in the pathogenesis of peptic ulcer disease.35 The control of gastric acid secretion in health and disease has been reviewed in detail36 and is discussed in Chapter 49.
HELICOBACTER PYLORI INFECTION (see also Chapters 50 and 51)
Most patients who have a chronic infection with H. pylori have a pan-gastritis in which the body and the antrum are equally involved. Gastritis results in inhibition of acid secretion, and various mechanisms have been proposed.37,38 These include direct inhibition of the parietal cell by lipopolysaccharides or toxins secreted by H. pylori or an indirect effect through stimulation of cytokines caused by the inflammation.1 Due to the decreased output of acid, these individuals with pan-gastritis do not usually develop ulcer disease related to H. pylori infection.39 The reduced acid production in H. pylori–infected individuals has been suggested as a factor that may protect against the development of reflux disease and its complications such as Barrett’s esophagus (see Chapters 43 and 44).
Another pattern of H. pylori infection affects approximately 10% to 20% of patients with chronic infection and consists of an antrum-predominant gastritis (see Chapters 50 and 51). In these individuals, through a series of steps not well understood but possibly involving reduced somatostatin concentrations in the antrum, basal and meal-stimulated acid secretion often increases. The increased acid output from the stomach results in increased acid delivery to the duodenum that can result in gastric metaplasia in the duodenal bulb. Some investigators believe that the metaplastic epithelium then becomes infected with H. pylori from the stomach, resulting in focal duodenitis, sometimes followed by ulcer formation. In contrast with patients with duodenal ulcer disease who often have increased acid secretion, patients with gastric ulcer typically have normal or decreased acid production, suggesting that the mechanism for the development of ulceration is a failure in the gastric mucosal protective mechanisms, described in more detail below. Acid antisecretory medication heals ulcers in patients with gastric ulcer and hypochlorhydria because acid changes the balance in favor of mucosal defense factors that restore mucosal integrity (see Chapter 53).
GASTRIC AND DUODENAL MUCOSAL DEFENSE MECHANISMS
As described in Chapter 49 the gastric mucosa has multiple defense mechanisms to protect it from digestion by acid and pepsin.40 These include the gastric surface epithelium,41–43 the mucus/phospholipid and bicarbonate barrier (mucus layer),44,45 epithelial cell renewal and regeneration,46,47 mucosal blood flow and the alkaline tide, and prostaglandin production.48–51 Prostaglandins also stimulate mucus, bicarbonate, and phospholipid production. Many prostaglandins also increase mucosal blood flow and stimulate epithelial regenerative processes. Inhibition of these protective effects by NSAIDs increases the likelihood of injury to the epithelium and decreases its ability to respond and regenerate.
Cyclooxygenase-1 (COX-1) and COX-2 are the enzymes responsible for the synthesis of prostaglandins. COX-1 is expressed in the stomach and is responsible for the maintenance of the integrity of gastric epithelium and the mucous barrier. COX-2 is not expressed in the healthy stomach but is rapidly expressed in response to the cytokines generated by inflammatory processes. Conventional NSAIDs such as ibuprofen inhibit the COX-1 and the COX-2 enzymes. It is believed that COX-1 inhibition reduces prostaglandin synthesis, which leads to a reduction in mucosal blood flow, hypoxia, and a reduction in mucosal defense. Neutrophil-endothelial interactions then occur as a result of the vascular disturbances and neutrophil activation. In experimental studies, COX-1 inhibition alone is not sufficient to cause ulceration.52 The inhibition of COX-1 up-regulates the expression of COX-2 that suppresses the neutrophil endothelial interaction that is stimulated by COX-1 inhibition. Inhibition of COX-1 and COX-2 enzymes is therefore important in the generation of gastric injury.
Some studies have suggested that a prostaglandin-independent mechanism may also contribute to damage by NSAIDs. One such mechanism is increased leukotriene production that occurs because arachidonic acid metabolism shifts to the alternative 5-lipooxygenase pathway when the COX-1 pathway is inhibited.40
The duodenum, like the stomach, secretes bicarbonate that neutralizes acid arriving into the duodenum.53 Decreased duodenal bicarbonate secretion has been reported in patients with duodenal ulcer.54 A protective role has also been postulated for pancreatic juice but the results have been conflicting.