CHAPTER 15 Diarrhea
Diarrhea is a universal human experience. The average American has an estimated 0.65 episodes of acute gastrointestinal illness per year.1 For most persons, episodes of diarrhea last a day or two and rapidly subside without medical intervention. For others, diarrhea lasts for more than a few days or is complicated by fever, prostration, or rectal bleeding. Such persons are likely to visit their physicians. Over 3.5 million outpatient visits for diarrhea occur each year.2 Most patients can be managed successfully as outpatients; however, more than 150,000 hospital admissions each year are for gastroenteritis. Over the course of a year, chronic diarrhea (liquid stools for more than four weeks) may occur in 5% of the population and is thus a major cause of disability for Americans.3 In developing countries, acute infectious diarrhea remains an important cause of morbidity and mortality, particularly among children.
DEFINITION
Most patients consider increased fluidity of stool as the essential characteristic of diarrhea.4 Stool consistency is difficult to quantitate and visual scales may be helpful for patients to use in describing their diarrhea.5 Researchers also have used stool frequency or stool weight as a surrogate marker of diarrhea. Three or more bowel movements daily are considered to be abnormal, and the upper limit of stool weight is generally agreed to be 200 g daily in Western countries. Although stool weight often is cited as a “scientific” definition of diarrhea, diarrhea should not be defined solely in terms of fecal weight. Some persons have increased fecal weight as a result of fiber ingestion but do not complain of diarrhea because their stool consistency is normal. For example, stool output can be as great as 300 g when a high-fiber diet is consumed, as is customary in some developing countries. Conversely, about 20% of patients referred for evaluation of diarrhea may have a normal stool weight. Whether this is a result of hyperdefecation (i.e., more frequent passage of formed stool) or a change in consistency (i.e., passage of small-volume loose stools) is unclear.
In a study of the objective determinants of decreased fecal consistency,4 the ability of water-insoluble fecal solids, such as those derived from dietary fiber or bacterial cell walls, to hold or bind fecal water correlated well with fecal consistency. Too little water-holding capacity to bind all the water present resulted in loose stools, but when fecal solids had sufficient water-holding capacity to bind all the water present, stools remained thick or formed. Fecal consistency correlated best with the ratio of the water-holding capacity of insoluble solids to the total amount of water present and not simply to the amount of fecal water, further supporting the concept that stool weight should not be the sole criterion for diarrhea.
Fecal incontinence may be reported as “bad diarrhea” by some patients, especially older adults.6 Although many incontinent patients have loose stools, their major problem is with the mechanisms of continence and not with intestinal fluid or electrolyte absorption. Accordingly, all patients who complain of diarrhea should be asked about the presence of fecal incontinence. If incontinence is frequent, especially in the absence of rectal urgency or loose stools, the patient should be evaluated for incontinence and not for diarrhea (see Chapter 17).
PATHOPHYSIOLOGY
Diarrhea frequently represents a protective response to a variety of intestinal insults and assaults. Normally, the intestine absorbs most of the fluid that it secretes, and intestinal motility provides a favorable milieu for water, electrolyte, and nutrient absorption. When infectious agents, toxins, or other noxious substances are present in the intestine, fluid secretion and motility are stimulated to expel the unwanted material, thereby producing diarrhea. This protective response is valuable acutely but, when chronic, it is inappropriate and no longer serves an adaptive purpose. Historically, diarrhea was thought to be primarily a motility disorder. An improved understanding of intestinal electrolyte transport since 1970 has shifted the emphasis to epithelial function, rather than motility. Clearly, however, epithelial and motor functions are altered in a coordinated fashion to produce diarrhea.7
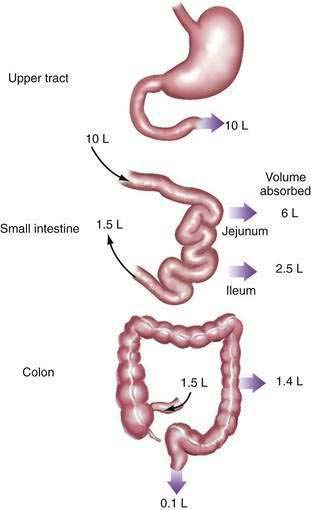
Diarrhea usually is the result of an excess of stool water rather than a decrease in the water-holding capacity of fecal solids, with the implication that water transport within the intestine is abnormal.4 Normally, the small intestine and colon absorb 99% of both oral intake and endogenous secretions from the salivary glands, stomach, liver, and pancreas—a total fluid load of approximately 9 to 10 L daily (Fig. 15-1). Diarrhea results from a disruption of this normally fine-tuned mechanism; reduction of water absorption by as little as 1% can result in diarrhea. Therefore, to understand the pathogenesis of diarrhea, one needs to understand normal water absorption by the intestine and the abnormalities that can impair water absorption.
Water itself is not actively transported but moves across the intestinal mucosa secondary to osmotic forces generated by the transport of solutes—that is, electrolytes and nutrients (see Chapters 99 and 100). The molecular pathways of ion and nutrient transport across the mucosa have been well characterized and are regulated by a complex communication system of extracellular and intracellular messengers that maintain fluid equilibrium throughout a wide range of physiologic conditions. Normally, absorption and secretion take place simultaneously, but absorption is quantitatively greater. Either a decrease in absorption or an increase in secretion leads to additional fluid within the lumen and diarrhea. Disruption of epithelial electrolyte transport or its regulatory system by toxins, drugs, hormones, and cytokines is a major cause of diarrhea.
Diarrhea resulting from disordered electrolyte transport is known as secretory diarrhea, even though it is more commonly caused by reduced absorption than by net secretion.8 Another major cause of diarrhea is ingestion of some poorly absorbed, osmotically active substance (e.g., magnesium ion, lactulose) that retains fluid within the lumen to maintain osmotic equilibration with body fluids, thereby reducing water absorption. Diarrhea resulting from this mechanism is known as osmotic diarrhea (Table 15-1). Few clinical situations produce pure secretory or osmotic diarrhea, but considering some conditions in which one or the other mechanism predominates is useful before considering more complex processes.
Table 15-1 Secretory versus Osmotic Diarrhea
| TYPE OF DIARRHEA | CAUSES | EXAMPLES |
|---|---|---|
| Secretory diarrhea | Exogenous secretagogues | Enterotoxins (e.g., cholera) |
| Endogenous secretagogues | Neuroendocrine tumors (e.g., carcinoid syndrome) | |
| Absence of ion transporter | Congenital chloridorrhea | |
| Loss of intestinal surface area | Intestinal resection, diffuse intestinal mucosal disease | |
| Intestinal ischemia | Diffuse mesenteric atherosclerosis | |
| Rapid intestinal transit | Intestinal hurry following vagotomy | |
| Osmotic diarrhea | Ingestion of poorly absorbed agent | Magnesium ingestion |
| Loss of nutrient transporter | Lactase deficiency |
OSMOTIC DIARRHEA
Ingestion of poorly absorbed cations and anions or poorly absorbed sugars or sugar alcohols (e.g., mannitol, sorbitol) accounts for most osmotic diarrheas.9 Ions that are poorly absorbed include magnesium, sulfate, and phosphate. These ions are transported actively by mechanisms that are saturated at low intraluminal ion concentrations and passively by mechanisms that are slow. Together, these processes limit total absorption to a fraction of the amount that can be ingested. Because neither the small intestine nor colon can maintain an osmotic gradient, unabsorbed ions (and their counter ions) that remain in the intestinal lumen obligate retention of water to maintain an intraluminal osmolality equal to that of body fluids (about 290 mOsm/kg). Therefore, approximately 3.5 mL of water (1000 mL/kg divided by 290 mOsm/kg) are retained for every 1 mOsm of retained ions or molecules.9–12
Sugars and sugar alcohols are the other category of substances that cause osmotic diarrhea.12 Monosaccharides, but not disaccharides, can be absorbed intact across the apical membrane of the intestine. When disaccharides such as sucrose and lactose are ingested, absence of the appropriate disaccharidase will preclude absorption of the disaccharide or its component monosaccharides (see Chapter 101). The most common clinical syndrome of disaccharidase deficiency is acquired lactase deficiency, which accounts for lactose intolerance in many adults.13 Lactase is present in the brush border of the small intestine of most immature mammals but disappears in adult mammals, including 70% of adult humans.14 The main exceptions are persons from the northern European gene pool, who typically maintain lactase activity into adult life. Lactase activity often falls with age even in this group, however. Congenital deficiency of lactase is rare and seems to be the result of a mutation in a gene distinct from that for lactase-phlorizin hydrolase (the gene affected in adult lactase deficiency).15 Acquired deficiencies also may be associated with mucosal diseases of the upper small intestine. Congenital sucrase and trehalase deficiencies are rare and prevent the adequate digestion of sucrose (table sugar) and trehalose (a sugar found in mushrooms), respectively. Lactulose is a synthetic disaccharide that cannot be hydrolyzed by the human intestine and is not absorbed intact in more than trace amounts. It thereby causes an osmotic diarrhea when given in sufficient quantity to overwhelm the metabolic capacity of colonic bacteria (about 80 g/day).
The essential characteristic of osmotic diarrhea is that it disappears with fasting or cessation of ingestion of the offending substance. This characteristic has been used clinically to differentiate osmotic diarrhea from secretory diarrhea, which typically continues with fasting. Electrolyte absorption is not impaired in osmotic diarrhea, and electrolyte concentrations in stool water are usually low.10–12
SECRETORY DIARRHEA
Secretory diarrhea has many causes, and the mechanism of this type of diarrhea is always net secretion of anions (chloride or bicarbonate) or net inhibition of sodium absorption.16 The stimuli for secretion arise from the intestinal lumen, subepithelial space, or systemic circulation and substantially alter the messenger systems that regulate ion transport pathways. In some cases, congenital absence of a specific transport molecule limits sodium or chloride absorption and results in diarrhea; in others, lack of sufficient absorptive surface area limits electrolyte, particularly sodium, absorption critically.
The most common cause of secretory diarrhea is infection.16 Enterotoxins from a host of infectious agents (primarily bacteria but also parasites and viruses) interact with receptors that modulate intestinal transport and lead to increased anion secretion. Enterotoxins also may block specific absorptive pathways in addition to stimulating secretion. Most enterotoxins inhibit Na+-H+ exchange in the small intestine and colon, thereby blocking one of the important driving forces for electrolyte and fluid absorption.17,18
Peptides, such as vasoactive intestinal peptide, produced by endocrine tumors, cause secretory diarrhea by stimulating secretion by epithelial cells, as do peptides released from subepithelial neurons and inflammatory cells (see Chapter 32).19 Neurotransmitters such as acetylcholine or serotonin (5-hydroxytryptamine, 5-HT) and other modulators such as histamine and inflammatory cytokines also are potent secretory stimuli.20,21 Most of these endogenous regulators of intestinal transport elicit diarrhea by altering intracellular messengers, such as cyclic adenosine monophosphate (cAMP), cyclic guanosine monophosphate (cGMP), and calcium, that control specific transport pathways.22 In addition, peptides and other regulators may affect the synthesis, localization, and degradation of individual transport proteins. Exogenous agents, such as drugs and some poisons, lead to secretory diarrhea, presumably by interacting with intracellular regulators or intracellular messengers of the enterocytes.
The absence or disruption of a specific absorptive pathway may cause diarrhea. For example, rare congenital syndromes, such as congenital chloridorrhea and congenital sodium diarrhea, are caused by the absence of a specific transport molecule.23 In chloridorrhea, Cl− -HCO3− exchange in the ileum and colon is defective, thereby transforming chloride into a poorly absorbed ion. Diarrhea resulting from chloridorrhea can be reduced by limiting oral chloride intake or chloride secretion (i.e., by reducing gastric acid secretion with a proton pump inhibitor) or by stimulating chloride absorption in the colon by enhancing short-chain fatty acid absorption.24 Several transporter defects have been proposed for congenital sodium diarrhea.25
-HCO3− exchange in the ileum and colon is defective, thereby transforming chloride into a poorly absorbed ion. Diarrhea resulting from chloridorrhea can be reduced by limiting oral chloride intake or chloride secretion (i.e., by reducing gastric acid secretion with a proton pump inhibitor) or by stimulating chloride absorption in the colon by enhancing short-chain fatty acid absorption.24 Several transporter defects have been proposed for congenital sodium diarrhea.25
More commonly, a relative shift in the balance of absorptive and secretory pathways may contribute to diarrhea in clinical settings associated with epithelial injury or changes in cell proliferation. For example, viral gastroenteritis and celiac disease may disproportionately compromise transporters (e.g., disaccharidases, Na+-coupled absorption) that mediate absorption on the villous surface, whereas secretory pathways in the crypt are unchanged or increased (see Chapters 104 and 107).
For intestinal fluid and electrolyte absorption to be complete, the intestine must have an adequate surface area and adequate contact time with luminal contents. Substantial loss of surface area, as in celiac disease or inflammatory bowel disease (IBD) or after resective surgery, may compromise water absorption. Even though the reserve absorptive capacity in the small intestine and colon is large, sufficiently long surgical resections inevitably cause diarrhea. In some cases, the problem is temporary, because over time the intestine may improve its capacity for absorption by the process of adaptation.26 Such compensation is impossible following resection of certain segments of the intestine with highly specific absorptive functions that simply cannot be assumed by other segments of the bowel. For example, ileocecal resection is followed by permanent inability to absorb sodium chloride against a concentration gradient27 and, if sufficient ileum is resected, by failure to absorb vitamin B12, intrinsic factor, and normal amounts of conjugated bile acids (see Chapter 103).
Abnormal motility may lead to diarrhea that has secretory and osmotic components.8 For fluid and electrolyte absorption to be complete, the contact time between luminal contents and the epithelium must be sufficient to permit absorption. In some patients, abnormal motility produces intestinal “hurry.”28,29 Because rapid transit prevents adequate time for absorption, diarrhea results despite intact mucosal absorptive capacity, as measured by intestinal perfusion studies during which contact time is maximized by rapid infusion of fluid into the intestine.8 In some patients with intestinal hurry, the oral-cecal transit time may be as short as 10 minutes. Under such circumstances, the diarrhea is exacerbated by malabsorption of nutrients that produces an osmotic component to diarrhea. In disorders such as diabetes mellitus and postvagotomy diarrhea, intestinal hurry has been linked to abnormal enteric nervous system function.30 In other clinical settings, such as amyloidosis, postprandial diarrhea, and irritable bowel syndrome (IBS), enteric nervous system dysfunction is suspected, but unproved.31,32 Many endocrine diarrheas, such as those caused by peptide-secreting tumors or hyperthyroidism, may lead to diarrhea not only by affecting intestinal electrolyte transport, but also by accelerating intestinal motility.33
Conversely, slow intestinal transit may lead to a secretory diarrhea by promoting small intestinal bacterial overgrowth.34,35 Excess bacteria in the small intestine disrupt digestion and may alter electrolyte transport. The best documented example of diarrhea related to this mechanism is scleroderma. Although diabetes mellitus is often suspected of causing diarrhea by slow transit and stasis, as seen in scleroderma, such a pathophysiology is not always established (see Chapter 102).36,37
Evaluation of the role of intestinal motility in the pathogenesis of diarrhea has been limited by the lack of the necessary tools to measure the interactions among motility, propulsive forces, and transit time. Except for intestinal perfusion studies, during which the effect of motility on electrolyte transport is eliminated, no methodology exists to dissociate the effects of intestinal transport and motility on net absorption.8 Thus, consensus has not been achieved on whether too much or too little motility causes diarrhea, nor on how luminal factors may alter intestinal smooth muscle function.
Reduced intestinal blood flow has an important but as yet poorly defined role in diarrhea. Whether mesenteric ischemia has a direct effect on absorption or whether low blood flow prompts secondary responses (e.g., via cytokines or neurotransmitters) that affect fluid transport and produce a secretory diarrhea is not clear. Radiation enteritis also produces an abnormal intestinal microcirculation associated with persistent diarrhea that may be difficult to treat (see Chapters 39 and 114).
COMPLEX DIARRHEA
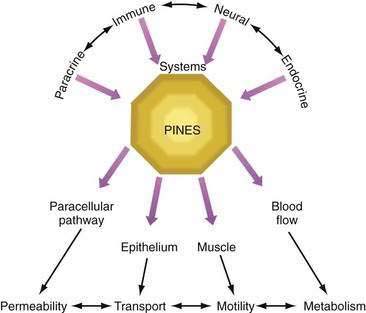
Although classification of diarrhea as osmotic or secretory may be instructive in thinking about the pathophysiology of diarrhea, cases of pure secretory or pure osmotic diarrhea are uncommon. Most clinically important diarrhea is complex in pathogenesis; rather than being produced by a single pathophysiologic mechanism, several mechanisms are involved. Causes may include the effects of substances released by enteric endocrine cells, cytokines released by local and remote immunologically reactive cells, activity of the enteric nervous system, and peripherally released peptides and hormones (paracrine, immune, neural, and endocrine systems; see Chapter 1).
Further complicating the understanding of diarrhea is the recognition that certain mediators affect not only epithelial or muscle function, but also each other. For example, enteric nerves may stimulate mast cells, and products released from mast cells (particularly histamine) may alter enteric neuron functions.38 A single agonist, such as prostaglandin, may have multiple simultaneous effects on epithelial function, muscle contraction, and the paracellular pathway, thereby leading to effects on ion transport, motility, and mucosal permeability.39 Therefore, a number of modulators and effectors contribute to the final clinical picture. A full appreciation of the pathophysiology of diarrhea requires consideration of a regulatory system known as PINES (paracrine, immune, neural, and endocrine system modulators; Fig. 15-2).
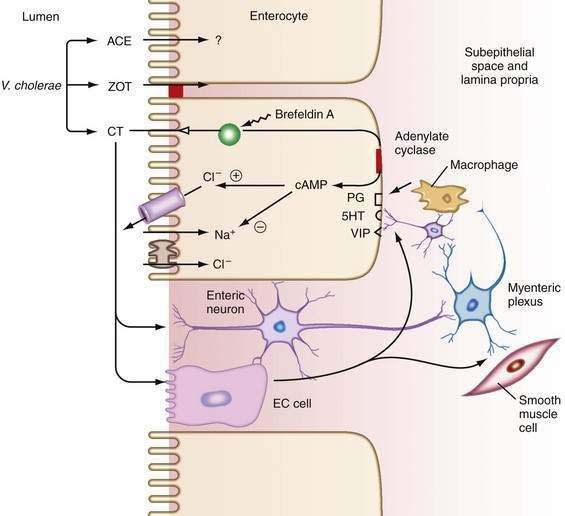
An example of the complexity of the pathophysiology of a diarrheal syndrome is cholera. Cholera is often cited as the paradigm of a pure secretory diarrhea: cholera toxin targets the epithelial cell, increases the second messenger, cAMP, which opens apical chloride channels to stimulate chloride secretion, and results in diarrhea; however, the actual mechanism whereby cholera induces diarrhea is far more complex.40 Cholera toxin stimulates endocrine cells and neural elements that reinforce its direct secretory effect on enterocytes.41 In addition, cholera toxin causes distinct changes in intestinal motility. Other toxins produced by Vibrio cholerae target tight junctions and thereby alter mucosal permeability (Fig. 15-3; see Chapter 107).42
Another example of dysregulation of PINES is IBD.43 Diarrhea in patients with IBD involves more than just exudation into the lumen as a result of destruction of the mucosa. Intact enterocytes are barraged by multiple secretagogues released by immune cells in the intestine and by bacterial toxins that may influence enterocyte function. Although initial models of diarrhea in IBD suggested altered fluid transport driven by chloride secretion, more recent studies have demonstrated that the diarrhea in IBD is mediated by an antiabsorptive effect associated with down-regulation of sodium channels and pumps.44–46 The pathophysiology of diarrhea in IBD is even more complex if we consider the role of luminal bacteria. Bacterial proteins, such as flagellin, may stimulate the production of cytokines, such as interleukin (IL)-8, which further attract inflammatory cells.47 Cytokines and immune cells also may influence tight junction barrier function and enterocyte secretory and absorptive pathways directly.48,49 Conversely, epithelial cells may secrete cytokines, such as IL-6, that enhance polymorphonuclear leukocyte (neutrophil) function.50
IBS is another example of a disorder with a complex pathophysiology. A constellation of factors, such as altered motility,32 bile acid malabsorption,51 and compromised rectal reservoir capacity,52 may aggravate symptoms in patients with IBS. At a more fundamental level, alterations in mast cell or enterochromaffin cell number, serotonin content, and serotonin reuptake and transport may contribute to the development of diarrhea (see Chapter 118).53–55
Complex pathophysiology also may be observed in malabsorption syndromes and functional disorders, particularly those characterized by rapid transit. Failure to absorb carbohydrates may lead to osmotic diarrhea, but failure to absorb long-chain fatty acids may complicate matters by impairing electrolyte absorption by the colon.12,56 Common postprandial functional diarrhea probably involves an interplay between motility and transport functions. Diarrhea caused by food allergy also involves activation of immunologic, paracrine, and neural mechanisms that regulate vascular permeability, electrolyte transport, and motility (see Chapters 9 and 101).57
CLINICAL CLASSIFICATION
ACUTE VERSUS CHRONIC DIARRHEA
The time course of diarrhea can help direct management. Acute diarrhea (<four weeks) usually is caused by an infection, which is generally self-limited or easily treated.58 Most common bacterial and viral causes of diarrhea run their course within seven days. Persistence of an acute diarrheal episode beyond seven days raises the possibility of a protozoal cause, such as giardiasis or cryptosporidiosis. Although few infectious agents (e.g., Aeromonas or Yersinia spp.) cause prolonged diarrhea in an immunocompetent person, chronic diarrhea is usually not caused by an infectious agent. Therefore, when confronted with a patient with chronic diarrhea, the clinician must consider noninfectious causes (see later).
LARGE-VOLUME VERSUS SMALL-VOLUME DIARRHEA
The daily total stool output may also provide hints about the cause. IBS often results in normal or only slightly elevated 24-hour stool weights, whereas diarrhea of other causes may produce greater stool weights. The stool weight can be estimated by the patient’s history: patients with diarrhea that produces dehydration (in the absence of vomiting or limited oral intake) typically have stool weights more than 1000 g and therefore are unlikely to have IBS (see Chapter 118).
OSMOTIC VERSUS SECRETORY DIARRHEA
Distinguishing diarrhea that results from intestinal malabsorption of ingested nonelectrolytes (osmotic diarrhea) from diarrhea that results from malabsorption or secretion of electrolytes (secretory diarrhea) helps separate the small number of cases of osmotic diarrhea from the much larger number of cases of secretory diarrhea. This distinction is based on the measurement of stool electrolyte concentrations.10 In secretory diarrhea, sodium, potassium, and accompanying anions account almost entirely for stool osmolality, whereas in osmotic diarrhea poorly absorbable solutes within the lumen of the intestine account for much of the osmotic activity of stool water (see later discussion). Because osmotic diarrhea is caused by the ingestion of some poorly absorbed substance, it abates with fasting. Secretory diarrhea typically continues during fasting, although stool output may decrease modestly because of reduced endogenous secretions.
WATERY VERSUS FATTY VERSUS INFLAMMATORY DIARRHEA
When diarrhea is chronic (>four weeks), the differential diagnosis can overwhelm even the most experienced clinician. By characterizing stools as watery, fatty, or inflammatory on the basis of simple stool tests, evaluation of the patient can be expedited by limiting the number of conditions that must be considered in the differential diagnosis.3 Watery diarrhea implies a defect primarily in water absorption as a result of increased electrolyte secretion or reduced electrolyte absorption (secretory diarrhea) or ingestion of a poorly absorbed substance (osmotic diarrhea). Fatty diarrhea implies defective absorption of fat and perhaps other nutrients in the small intestine. Inflammatory diarrhea implies the presence of one of a limited number of inflammatory or neoplastic diseases involving the gastrointestinal tract.
EPIDEMIOLOGIC FEATURES
One of the most useful clinical approaches to narrowing the differential diagnosis is to relate diarrhea to its setting. For example, a soccer mom and a backpacker from Nepal conceivably could have the same cause of the diarrhea but are more likely to have different causes. Some common clinical scenarios and the diagnoses that should be considered are shown in Table 15-2.
Table 15-2 Likely Causes of Diarrhea in Well-Defined Patient Groups or Settings
DIFFERENTIAL DIAGNOSIS
Many gastrointestinal and systemic diseases may present with diarrhea. To facilitate the differential diagnosis, the clinician should divide diarrheal diseases into acute and chronic and further subdivide chronic diarrhea by stool characteristics—watery, inflammatory, and fatty (Table 15-3).
Table 15-3 Differential Diagnosis of Diarrhea
| Acute Diarrhea |
| Chronic Diarrhea |
| Fatty Diarrhea |
| Inflammatory Diarrhea |
| Watery Diarrhea |
Acute diarrhea is defined as lasting less than four weeks, although many cases last shorter than four days.58 The usual cause is infection by bacteria, viruses, protozoa, or multicellular parasites (Table 15-4). Acute diarrhea also can be caused by food poisoning, food allergies, and medications. Diseases that lead to chronic diarrhea may present with an acute onset and therefore must be considered when acute diarrhea becomes persistent (see Chapter 107).
Table 15-4 Infections That Cause Diarrhea
Chronic watery diarrhea may be caused by ingestion of poorly absorbed, osmotically active substances (osmotic diarrhea) or, more commonly, conditions that cause secretory diarrhea. Ingestion of any of a limited number of osmotic agents, such as magnesium, phosphate, and sulfate laxatives, or poorly absorbed carbohydrates, causes osmotic diarrhea. By contrast, chronic secretory diarrhea, in which electrolyte malabsorption leads to retention of fluid within the lumen, is associated with many clinical conditions (see Table 15-3).
Although IBD typically produces diarrhea characterized by the presence of blood and pus, other diseases of inflammation without ulceration, such as microscopic colitis, cause diarrhea with the characteristics of chronic secretory diarrhea. Diarrhea in such cases is thought to be mediated by secretion of cytokines and other inflammatory mediators (see Chapter 124).
Chronic watery diarrhea can also be caused by the ingestion of drugs or poisons (Table 15-5).59–61 Identification of drugs as the cause of diarrhea depends on recognizing that the initiation of drug ingestion and the onset of diarrhea occurred coincidentally. Such a temporal correlation, however, is not always easy to identify and requires a detailed and carefully taken history. The pathophysiology of drug-induced diarrhea is complex and has not been carefully studied. Some drugs may activate specific receptors and transporters; for example, caffeine, like theophylline, may increase intracellular cAMP activity and fluid secretion. Clinically, this phenomenon can be seen in cases of what has been called “Starbucks diarrhea.” Erythromycin interacts with the motilin receptor, thereby stimulating propulsive motor activity in the gastrointestinal tract. Other antibiotics may alter the bacterial flora in the colon and lead to impaired colonic salvage of malabsorbed carbohydrate or overgrowth of toxin-producing Clostridium difficile. Some drugs such as cocaine may interfere with blood flow to the intestine. Chemotherapeutic agents are associated with a high frequency of diarrhea, which may result from disruption of the delicate balance between enterocyte proliferation and apoptosis, leading to what has been termed an apoptotic enteropathy. A diverse group of drugs (e.g., aspirin, mycophenolate mofetil, gold) can incite an inflammatory process in the intestine that may cause diarrhea. The problem of detecting drug-induced diarrhea is more difficult in patients with surreptitious laxative abuse, because these patients deliberately conceal vital information about the cause of their problem (see later discussion of factitious diarrhea).62
Table 15-5 Medications and Toxins Associated with Diarrhea
NSAIDs, nonsteroidal anti-inflammatory drugs.
Another category of chronic watery diarrhea involves disordered motility or dysregulation of intestinal function. Problems such as postvagotomy diarrhea, postsympathectomy diarrhea, diabetic autonomic neuropathy, amyloidosis, and probably diarrhea-predominant IBS belong in this category. In these situations, the diarrhea has the characteristics of a secretory diarrhea, because of primary dysregulation of electrolyte transport or of altered motility that speeds luminal fluid past absorptive sites in the intestine (see Chapters 35, 53, and 118).
Another large category of watery diarrhea is diarrhea caused by endocrine dysfunction. Relatively common endocrine disturbances, such as hyperthyroidism and Addison’s disease, can be complicated by chronic secretory diarrhea. Much rarer endocrine tumors also produce diarrhea, typically by altering electrolyte absorption or speeding intestinal transit. The rarity of these tumors makes the pretest probability of finding these conditions low, especially in the absence of liver metastases, and therefore screening tests often are falsely positive (see later and Chapters 31, 32, and 35).
Other tumors cause watery diarrhea by obstructing bowel, blocking lymphatic drainage, interfering with absorption, or causing electrolyte secretion. Examples of such conditions include colon carcinoma (bowel obstruction), lymphoma (lymphatic obstruction in the small bowel and mesentery), and villous adenomas of the rectum (secretion of a large amount of potassium-rich gelatinous fluid into the lumen). Villous adenomas found more proximally in the colon rarely cause this type of diarrhea (see Chapters 29, 122, and 123).
The last category of chronic watery diarrhea is idiopathic secretory diarrhea. This rubric includes two entities, epidemic secretory diarrhea (also known as Brainerd diarrhea) and sporadic idiopathic secretory diarrhea. Both disorders are protracted but self-limited conditions (see later discussion of idiopathic secretory diarrhea).63,64
Chronic inflammatory diarrhea is the designation for a diverse group of infectious or idiopathic inflammatory and neoplastic processes. Stools are characterized by the presence of mucus and pus and are usually associated with ulceration of the mucosa. Idiopathic IBD, including ulcerative colitis and Crohn’s disease, typically produces such stools. Less commonly, other inflammatory conditions such as diverticulitis or ulcerative jejunoileitis may be associated with blood or pus in the stool, as may infectious diseases that are invasive or ulcerating. Infections that cause chronic inflammatory diarrhea include bacterial infections, such as tuberculosis, yersiniosis, and Clostridium difficile–associated colitis, viral infections that ulcerate, such as cytomegalovirus and herpes simplex virus, and invasive parasitic infections, such as strongyloidiasis. In the immunocompromised person, a broader range of infectious agents should be considered. Noninfectious diseases that cause chronic inflammatory diarrhea include ischemic colitis, and neoplasms, such as colon cancer or lymphoma, that are complicated by ulceration of the mucosa (see Chapters 29, 107 to 112, 114, 115, 117, and 123).
Chronic fatty diarrhea results from malabsorption or maldigestion. Malabsorption syndromes caused by mucosal diseases, such as celiac disease or Whipple’s disease, typically produce fatty diarrhea. Short bowel syndrome or postresection diarrhea can also present with this pattern, although if the resection is relatively limited, the diarrhea may be watery secondary to nutrient or bile-acid malabsorption. Small intestinal bacterial overgrowth causes steatorrhea by deconjugation of bile acids. Mesenteric ischemia affecting the small intestine may impair intestinal absorption of fat, but weight loss is more often attributed to sitophobia (“fear of eating”) because of postprandial pain. Maldigestion as a result of pancreatic exocrine insufficiency or inadequate duodenal bile acid concentration produces steatorrhea. Although fatty, the stools may not be very loose in maldigestive conditions because, in the absence of fat digestion, triglyceride remains intact and has little effect on colonic electrolyte absorption. By contrast, malabsorption in the presence of normal digestion may produce fairly voluminous diarrhea because of the cathartic action of free fatty acids in the colon (see Chapters 59, 101, 103 to 106, and 114).61
EVALUATION OF THE PATIENT
HISTORY
Stool characteristics, such as the presence of blood, mucus, pus, oil droplets, or food particles, are also important. Blood in the stool signals the possibility of malignancy or IBD, although it is often caused by hemorrhoids in patients with frequent evacuations. In patients with acute infectious diarrhea, visible blood in the stool is highly specific for infection with an invasive organism.65 Watery stools suggest an osmotic or secretory process, and the presence of oil or food particles is suggestive of malabsorption, maldigestion, or intestinal hurry. The phenomenon of floating stools generally represents an increase in the gas content rather than the fat content of the stools. The physician should also ask about the relationship of defecation to meals or fasting, passage of stool during the day versus the night, and presence of fecal urgency or incontinence. Urgency and incontinence are not indicative of voluminous diarrhea but suggest a problem with rectal compliance or with the muscles regulating continence. Nocturnal diarrhea that awakens the patient from sleep strongly suggests an organic rather than a functional disorder such as IBS. Other coexisting symptoms such as abdominal pain, flatulence, bloating or gaseous distention, cramps, fever, and weight loss should be noted. Excessive flatus suggests increased fermentation of carbohydrate by colonic bacteria as a result of ingestion of poorly absorbable carbohydrate or malabsorption of carbohydrate by the small intestine.
Because iatrogenic causes of diarrhea, such as drugs, previous surgery, or radiation therapy, are common, the physician should explore the history thoroughly for prior abdominal surgeries and ingestion of prescription drugs and over-the-counter remedies, including nutritional and herbal therapies. The patient’s diet should be reviewed thoroughly because diarrhea may result from ingestion of large quantities of poorly absorbable carbohydrates, such as fructose, or sugar alcohols, such as sorbitol or mannitol, which may be consumed in fruit juices and soda (which contain fructose and high-fructose corn syrup) or as dietetic, sugar-free candies and chewing gums (which contain sorbitol and mannitol).66
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree