3 Pelvic Organ Prolapse
Introduction, Nonsurgical Management, and Planning of Surgical Repair
Epidemiology and Pathophysiology
POP is a common worldwide problem, but data are conflicting on whether differences in prevalence exist based on race and culture. Most reports suggest a higher incidence in white and Hispanic women than in black or Asian populations, but no good comparison studies exist.
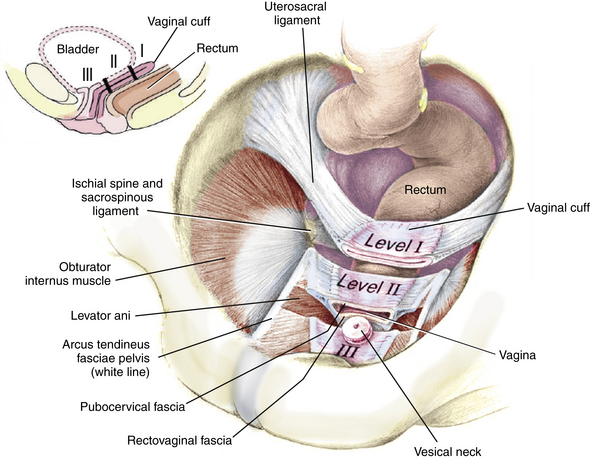
The apical portion of the vagina is supported by sheetlike extensions of the endopelvic fascia that attach it to the pelvic sidewall and levator ani fascia, referred to as the paracolpium. The paracolpium provides two levels of support. Level I, or upper support, suspends the vagina, attaching it to the pelvic sidewall. Level II, or midvaginal support, which includes the pubocervical fascia, attaches the midvagina more directly to the pelvic walls, including the levator fascia and arcus tendineus fasciae pelvis. Damage to midlevel support usually results in anterior and posterior defects, whereas damage to upper-level support results in apical prolapse, including enterocele and/or vault or uterine prolapse (Fig. 3-1).