Fig. 1 a–d
Acute cholecystitis. a, b Longitudinal ultrasound (US) shows a large stone impacted in the gallbladder neck, gall bladder wall thickening (arrow), and gall bladder wall hyperemia on color Doppler. c, d Contrast-enhanced computed tomography (CT) with intrave nou sly and orally administered contrast media shows a distended gallbladder containing a stone, gallbladder wall thickening (arrowhead), pericholecystic inflammation, and hyperenhancement of the adjacent liver (arrow)
Gangrenous cholecystitis is another form of severe inflammation that results in gallbladder wall ischemia and necrosis. The diagnosis should be suggested when intraluminal membranes from sloughed gallbladder mucosa are seen on US. The gallbladder wall may appear striated and have irregular thickening. Often, a sonographic Murphy sign is absent in patients with gangrenous cholecystitis; CT findings are more specific. The absence of gallbladder wall enhancement is the most important feature and is indicative of ischemia (Fig. 2). Intraluminal membranes, hemorrhage, and gallbladder wall disruption are additional findings.
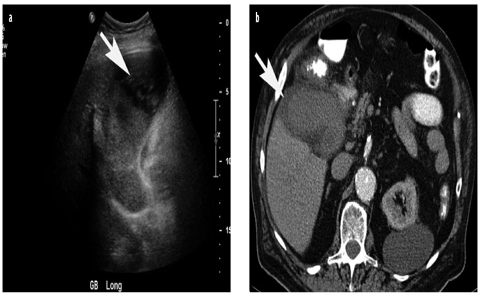
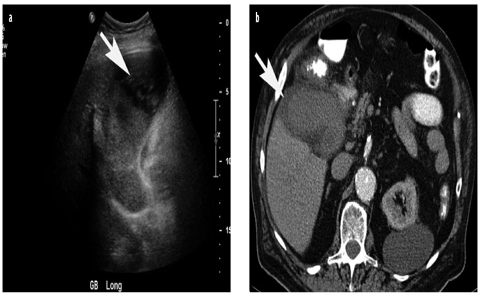
Fig. 2 a,b
Gangrenous cholecystitis. a Longitudinal ultrasound (US) shows a distended gallbladder containing sludge and intraluminal membranes (arrow). b Contrast-enhanced computed tomography (CT) using intravenously and orally administered contrast media shows nonenhancing, thick gallbladder wall (arrow). The high attenuation in the gallbladder lumen represents blood products
Xanthogranulomatous cholecystitis (XGC) is a rare form of chronic cholecystitis that resembles gallbladder carcinoma on imaging studies. The presumed etiology is intermittent cystic duct obstruction from stones. During episodes of obstruction, increased intraluminal pressure within the gallbladder causes intravasation of bile into the gallbladder wall. The intravasated bile causes a chronic, lipid-laden, inflammatory process. There is a significant overlap in CT features of XGC and gallbladder carcinoma. Both entities may demonstrate wall thickening, infiltration of the surrounding fat, hepatic invasion, and lymphadenopathy. XGC can be suggested when nodular foci are observed in the gallbladder wall (Fig. 3). Foci are hypoechoic on US and hypoattenuating on CT and represent foci of lipid-laden inflammation in the gallbladder wall. In most cases, this is difficult to differentiate prospectively from degeneration or necrosis that may be found in gallbladder carcinoma.
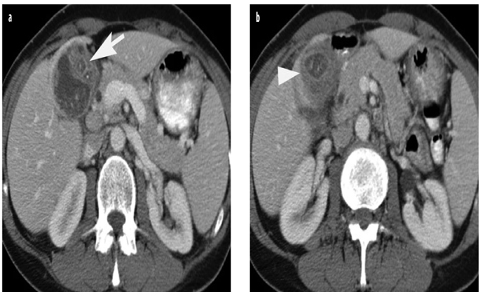
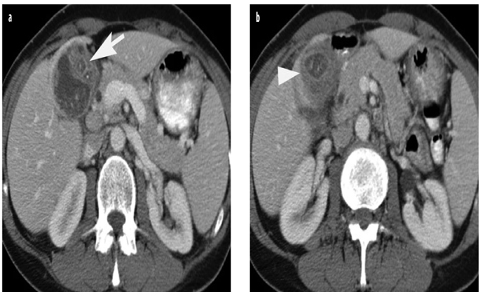
Fig. 3 a,b
Xanthogranulomatous cholecystitis. Contrast-enhanced computed tomography (CT) using intravenously and orally administered contrast media shows asymmetric thickening of the gallbladder wall. Round foci of hypoattenuation (a, arrow) are visible within the thickened wall. The process invades the adjacent liver (b, arrowhead)
Adenomyomatous hyperplasia, also called adenomyomatosis, is a common benign tumor-like lesion of the gallbladder that may produce focal, segmental, or diffuse mural thickening. Pathologically, adenomyomatosis is characterized by hyperplasia of all layers of the gallbladder wall. Epithelial hypoplasia results in the formation of exaggerated invaginations called Rokitansky-Aschoff sinuses. Muscular hyperplasia thickens the gallbladder wall. Sonographically, adenomyomatous hyperplasia is characterized by echogenic foci that produce a characteristic reverberation artifact, commonly called ring-down artifact, emanating from the gallbladder wall. The ringdown artifact produces twinkle artifact on color Doppler (Fig. 4). Echogenic foci represent bile salts, cholesterol crystals, or small stones in Rokitansky-Aschoff sinuses. Focal or diffuse gallbladder wall thickening commonly accompanies the ring-down artifact. Focal adenomyomatosis is often localized in the gallbladder fundus. On MR, Rokitansky-Aschoff sinuses are best visualized on breath-hold T2-weighted MRI sequences as small, round foci of high T2 signal (Fig. 4) that in severe cases are visible throughout the gallbladder wall. This appearance is called the pearl-necklace sign. In cases with significant wall thickening, the finding of Rokitansky-Aschoff sinuses on MRI may be a helpful distinguishing feature from gallbladder carcinoma, which also may cause significant wall thickening.
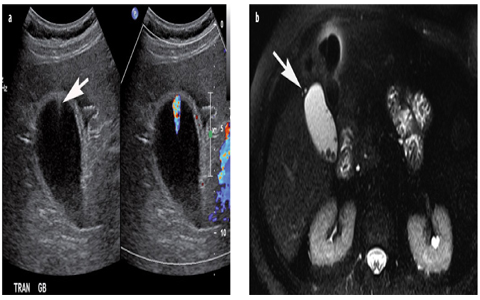
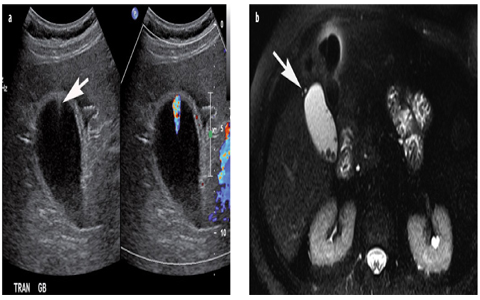
Fig. 4 a, b
Adenomyomatosis. a Ultrasound (US) shows ring-down artifact (arrow) emanating from a mildly thickened gallbladder wall, with twinkle color artifact on color Doppler. b Fat-saturated T2-weighted magnetic resonance imaging (MRI) shows two bright foci (arrow) in the wall of the gallbladder fundus that represent Rokitansky-Aschoff sinuses. Gallstones are also present
Gallbladder Polyps and Masses
Gallbladder polyps are commonly demonstrated as incidental findings when the gallbladder is imaged on sonography and are estimated to be present in approximately 3% of gallbladders. The differential diagnosis for a gallbladder polyp includes cholesterol polyp, adenoma, focal adenomyomatous hyperplasia, inflammatory polyp, heterotopia, neurofibroma, carcinoma, carcinoid tumor, lymphoma, and metastasis. The majority of gallbladder polyps are benign, the most common type being the cholesterol polyp, which accounts for approximately 50% of all polypoid lesions. Cholesterol polyps are not neoplastic and consequently have no malignant potential. They represent focal accumulation of lipid-laden macrophages and are covered by normal gallbladder epithelium. On sonography, cholesterol polyps are typically brightly echogenic round or slightly lobulated lesions that do no produce acoustic shadowing (Fig. 5). Larger cholesterol polyps are usually less echogenic and may contain an aggregation of echogenic foci.
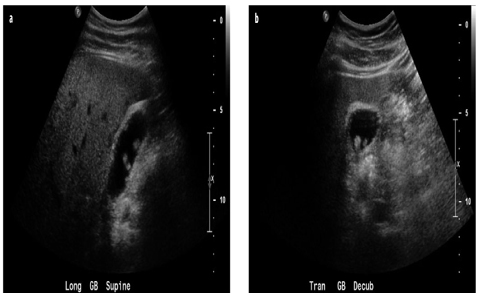
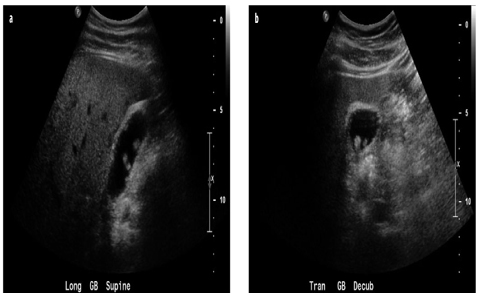
Fig. 5 a, b
Cholesterol polyps. Longitudinal (a) and transverse (b) ultrasound (US) images show multiple small, hyperechoic, intraluminal gallbladder polyps
Adenomas and small polypoid adenocarcinomas are usually much larger than cholesterol polyps and tend to be less hypoechoic on US, presenting with a more lobular appearance. Because the incidence of neoplastic polyps increases with the increasing size of a polyp, managing gallbladder polyps is based on size. Studies show that the risk of malignancy increases for polyps >10 mm in size and in patients >60 years. The incidence of malignancy in polyps >10 mm ranges from 37% to 88%. Therefore, it is recommended that patients undergo cholecystectomy for asymptomatic polyps >10 mm. Polyps between 5 mm and 10 mm should be followed periodically by US; those >5 mm with classic features of cholesterol polyps can be left alone. However, at sonography, careful attention should be paid to other features that suggest malignancy, such as thickening or nodularity of the gallbladder wall; evidence of hepatic invasion, such as an indistinct margin between the liver and gallbladder; biliary duct dilatation; and peripancreatic hepatoduodenal ligament adenopathy (Fig. 6). If any features are suggestive of malignancy, MDCT or MRI should be considered to further characterize and potentially stage the mass.
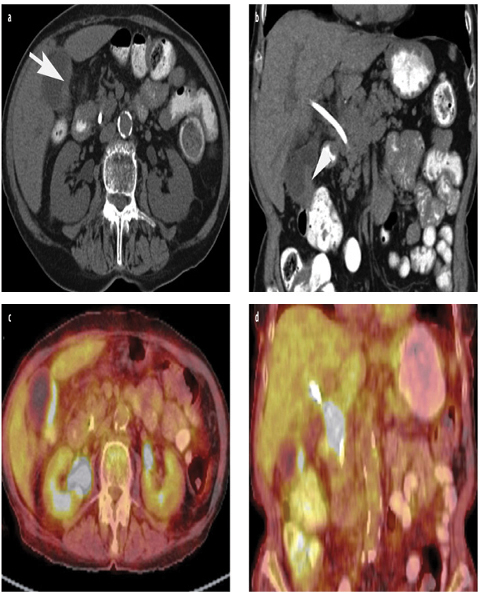
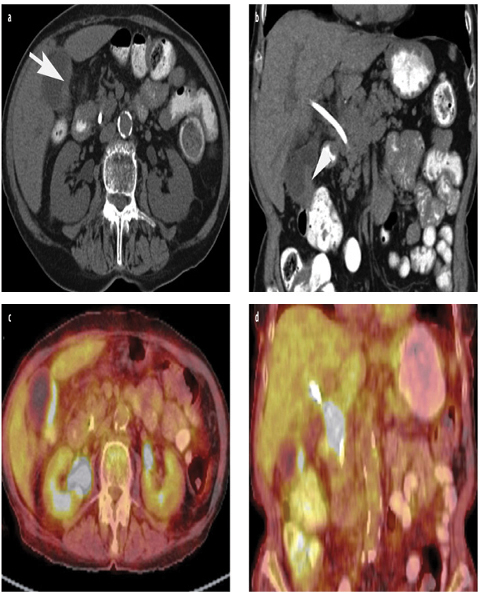
Fig. 6 a–d




Gallbladder carcinoma. a, b Contrast-enhanced computed tomography (CT) using orally administered contrast medium shows focal gallbladder wall thickening (a, arrow) with irregular margins that extends to invade the adjacent transverse colon (b, arrowhead) and hepatoduodenal ligament. A bile duct stent is in place. c, d Fluorine-18-deoxy-glucose ([18F]-FDG) positron emission tomography computed tomography (PET-CT) shows metabolically active gallbladder wall thickening and a mass encasing the common bile duct that most likely represents metastatic disease
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








