Overlapping Repair
Brooke Gurland
Tracy Hull
In otherwise healthy younger women, direct sphincter trauma or neuropathic injuries from vaginal deliveries are the principal causative factors in the development of fecal incontinence (1). Prospective studies using anal physiologic testing have shown that anal sphincter injuries can occur after vaginal deliveries without any visible signs of perineal trauma in 11.5–35% of patients (2). A delayed presentation of fecal incontinence can also occur as the effects of menopause summate with those of pelvic muscular and neurologic injuries to produce overt symptoms of urinary incontinence, pelvic organ prolapse, and fecal incontinence (3,4).
In the United States, sphincteroplasty is the most commonly performed procedure for fecal incontinence. Overlapping anal sphincter repair is the operation of choice for the incontinent female with an anatomically disrupted external anal sphincter (EAS) muscle. It can be performed for any type of injury to the EAS muscle, such as those due to anorectal surgery or trauma, but is most commonly performed for obstetric injury.
Transanal ultrasound, manometry, and pudendal nerve latencies are important diagnostic studies in the evaluation of patients with fecal incontinence. These tests help to delineate other etiologies of fecal incontinence. These tests provide us with objective evaluation of anal neuromuscular function that would not be otherwise detected on clinical examination. Anal sphincter injuries are detected by a break in the muscular ring visualized on 2-D or 3-D anal ultrasonography. Defects may be reported as EAS, internal anal sphincter (IAS), or combined injuries.
Bilateral, not unilateral, pudendal neuropathy is associated with diminished sphincter function and higher incontinence scores. In some studies, bilateral prolonged pudendal nerve latencies have been shown to be a poor prognostic indicator in patients undergoing anal sphincter repair and are a relative contraindication to sphincter repair (5). However, the significance of pudendal nerve terminal latencies has been debated by others.
A detailed bowel history is performed to assess stool consistency and frequency of bowel movements (BMs). Loose watery BMs may be difficult to control even in the setting of normal sphincter function and evaluation of diarrhea should be initiated
before considering sphincter repair. Bulking agents and constipating medications are recommended as first-line therapy to minimize BMs, thus decreasing incontinent episodes.
before considering sphincter repair. Bulking agents and constipating medications are recommended as first-line therapy to minimize BMs, thus decreasing incontinent episodes.
The following information should be collected regarding fecal accidents: urgent versus passive incontinence, type of incontinence (gas, liquid, solid, mucus), frequency, and quantity of fecal incontinnce (FI). A validated incontinence scoring system should be used (6). Women with more predictable bowel habits but with FI of solid stool tend to improve postoperatively compared to women with bothersome gas incontinence that is frequently not corrected with sphincter repair. It is very important to set realistic expectations with the patients about their anticipated postsphincteroplasty bowel control.
Physical examination of the perineum should reveal visible contraction of the sphincter muscle, and no evidence of rectal prolapse. Absence of sphincter contractions during perineal examinations can be a poor prognostic indicator.
Overlapping sphincter repair is generally performed without a diverting stoma unless there is a complex injury with a cloacal defect, redo sphincter repair, or complex rectal-vaginal fistula.
Preoperative management includes the following:
Appropriate patient selection
Setting realistic postoperative continence expectations
Mechanical bowel preparation 24 hours before the onset of surgery
A single dose of intravenous antibiotics administered prior to the surgery
Operative Positioning
The patient is positioned in the prone jackknife position on a Kraske Roll.
The procedure is performed under general or spinal anesthesia.
Large tapes are used to separate the buttocks for exposure of the anus.
Although we prefer prone jackknife position, this procedure can also be performed in lithotomy, which may be preferable if the patient is undergoing a concomitant urinary or prolapse procedure.
Operative Technique
A number of different techniques have been described for sphincteroplasty and the choice of technique is operator-dependant. Some authors advocate an en bloc overlapping sphincteroplasty, avoiding separating the internal and external sphincters (7) (see sphincteroplasty video), while others deliberately try to restore normal anatomy (8).
Sterile preparation of the perianal area, vagina, and perineum is performed.
A foley catheter is placed in the bladder.
Injection of the perineal body with 0.25% bupivacaine with 1:100,000 epinephrine.
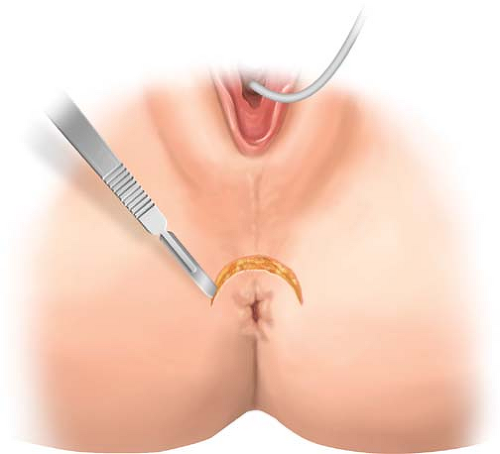
An anterior 120-degree curvilinear incision is made along the perineum with a 15-blade scalpel to allow dissection and mobilization of the sphincter muscle and scar.
Sharp dissection is used until we adequately identify the anatomy.
The skin edges are grasped with Allis clamps for exposure and flaps are developed toward the anal verge and the vagina. Care is taken not to “button hole” the skin.
Lateral dissection, where the muscle anatomy is intact, can help to identify the proper plane of dissection. The EAS is the medial border of the ischiorectal fossa and identification of the ischiorectal fat is useful landmark to identify the lateral border of dissection.
The scar tissue is divided through the midline if the sphincters halves are joined by scar. It is important to preserve all scar tissue in order to anchor the sutures. In other cases, the muscles edges are retracted laterally and grasped with Allis clamps.
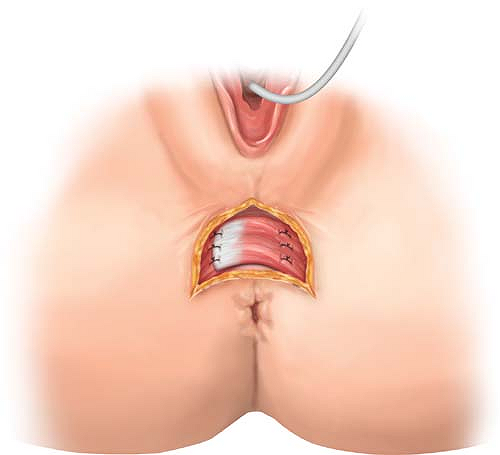
After adequate mobilization, an en bloc overlapping of the EAS/IAS complex is performed.
Incision and dissection are performed as noted during EAS/IAS overlap (Fig. 11.1).
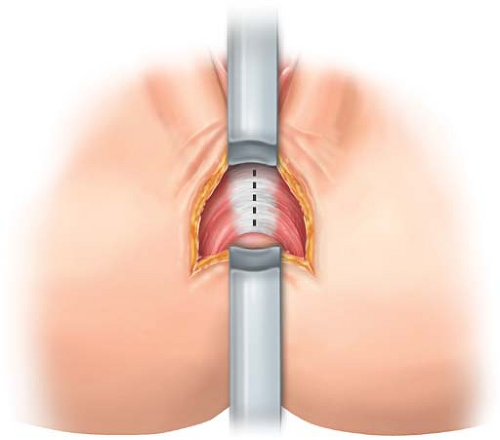
The intersphincteric space is then mobilized from lateral to medial to the area of the midline scar and external and internal anal sphincters are separated (Fig. 11.2).
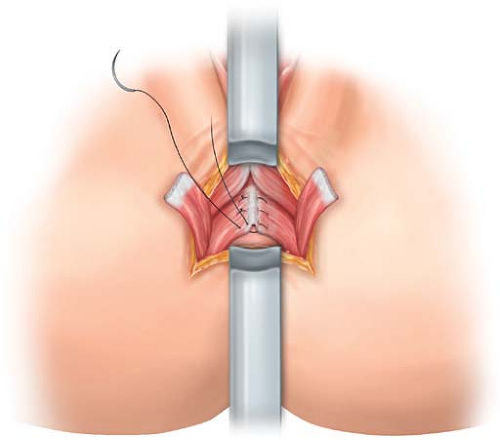
The repair starts with apposition of the levator muscles with interrupted 3, 2.0 polydioxanone monofilament delayed absorption suture.
The internal muscle fibers are identified and imbricated with 3, 3.0 sutures (Fig. 11.3).
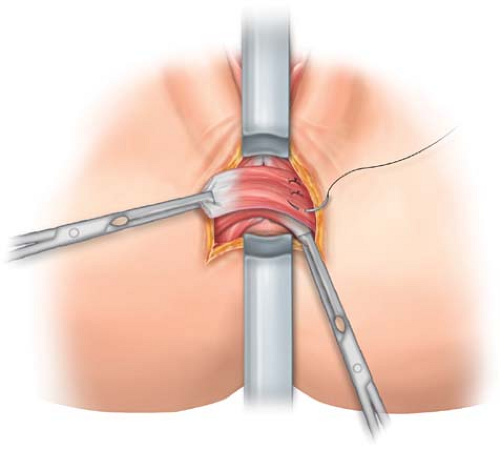
The EAS is overlapped and four mattress sutures are used to approximate the ends 2.0 sutures (Fig. 11.4).
Careful hemostasis is maintained with electrocautery throughout the procedure.
The wound is irrigated with tetracycline infused antibiotic solution.
The tapes are loosened prior to skin closure.
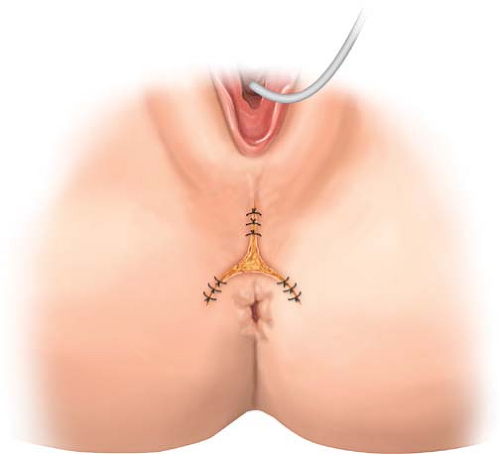
The edges of the wound are approximated in a V-shape or longitudinally with interrupted 3.0 absorbable mattress sutures (Fig. 11.5). The center of the wound can be left open, a small drain inserted, or the wound can be closed (Fig. 11.6).
The perineal body is bulkier than it was preoperatively.
Postoperative management requires keeping the stools soft, the area clean, and pain tolerable; patients are kept overnight 1–2 days. There is no consensus on the routine
administration of postoperative oral antibiotics at discharge. The patient is discharged on stool softeners. Maintaining the patient nothing by mouth and constipated does not have any proven benefit (10).
administration of postoperative oral antibiotics at discharge. The patient is discharged on stool softeners. Maintaining the patient nothing by mouth and constipated does not have any proven benefit (10).
Complications that may occur in the early postoperative period include formation of a hematoma or seroma. This complication can be treated by opening the wound and evacuating the hematoma or seroma. Fecal impaction can cause disruption of the repair. Late complications include abscess formation and wound breakdown. Abscesses require drainage, wound breakdown usually heals secondarily, and rarely does this require secondary suturing. The patient’s main complaint after surgery is pain from the perineal wound.