LYMPHOMA
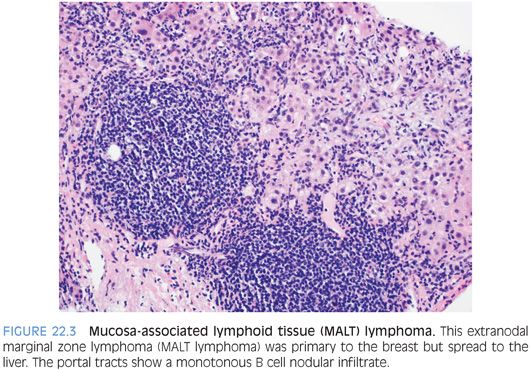
Most lymphomas involving the liver are not primary lymphomas. Essentially, any lymphoma can, at some point, involve the liver as it spreads from its site of origin (Fig. 22.3, eFigs. 22.2 to 22.5). In the adult who is not immunosuppressed, primary liver lymphomas are rare and most commonly seen in middle-aged men. Most primary liver lymphomas are either diffuse large B-cell lymphomas or are hepatosplenic T-cell lymphomas.1,2 However, rare primary cases of many different types of lymphoma have also been reported.1 The etiology is unknown in most cases, although a potential link with chronic hepatitis C infection has been reported.1 Diffuse large B-cell lymphomas of the liver can form mass lesions (eFig. 22.6) or more diffusely infiltrate the portal tracts or lobules (eFig. 22.7).
The diagnosis of lymphoma is made following usual criteria, which for space constraints cannot be completely reviewed here. However, a few important diagnostic pitfalls will be discussed. In most cases that present with a mass lesion, the atypical lymphoid infiltrates will suggest the correct diagnosis. However, in some cases, especially on biopsy, the cells may appear epithelioid and mimic a carcinoma. Because the mass-forming B-cell lymphomas often have entrapped hepatocytes, a Hep-Par stain or other keratin stains can further confuse the issue and lead to an incorrect diagnosis if not carefully examined.
Hepatosplenic T-cell lymphomas manifest as atypical lymphoid cells in sinusoids with absent or minimal portal tract involvement. The infiltrates are typically moderate to marked in their cellularity but can be somewhat patchy. The individual cells tend to have moderate eosinophilic cytoplasm and have larger and more irregular nuclei than typical lymphocytes. The nuclei usually have small basophilic nucleoli.
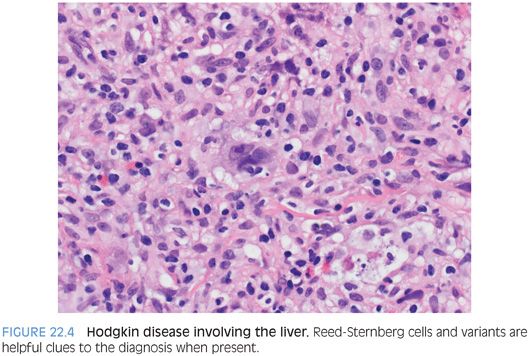
Hodgkin disease can appear as a nodular infiltrate in the liver, involving both the portal tracts and the lobules (eFig. 22.8). The nodules are often fibrotic and have mixed inflammation including lymphocytes, plasma cells, and eosinophils. The nodules can vary in size from small portal-based nodules to large aggregates that fill several low-power microscope fields. Plasma cells can be prominent, and the findings can mimic an inflammatory pseudotumor. Other cases can mimic hepatic parenchymal collapse. Reed-Sternberg cells and variants are helpful when present (Fig. 22.4).