Optimizing Computed Tomography Technique
Judy Yee
The computed tomography (CT) parameters specifically used to examine the colon for CT colonography (CTC) has evolved with the advancement of CT technology. Helical CT allows volumetric data acquisition and is a requirement for CTC. Helical scanning is based on slipring CT technology, which couples continuous motion of the gantry with synchronous table feed.
Single-detector CT enables the performance of CTC. However, multidetector computed tomography (MDCT) is preferred for optimizing the acquisition of data and improving the performance of CTC. Each detector acts as a single unit in single-detector CT and section thickness is determined by the collimation of the x-ray beam. MDCT segments the detectors in the z-axis (longitudinal) plane so that multiple slices per rotation may be acquired. Section thickness is determined by the thickness of each detector row on a MDCT scanner.1 The number of data channels present in a specific CT scanner determines the actual number of slices that may be obtained.
MULTIDETECTOR COMPUTED TOMOGRAPHY
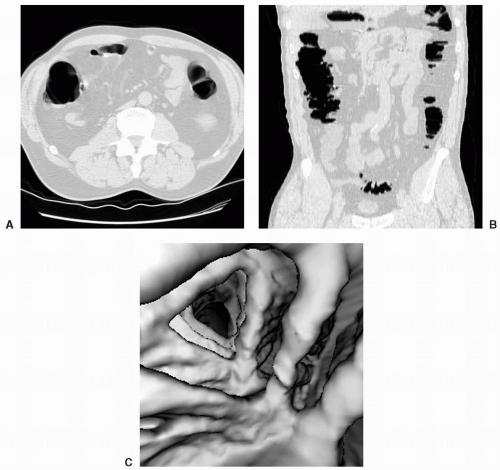
The use of MDCT is an advantage for CTC because the entire abdomen and pelvis may be scanned in a shorter amount of time using thinner slices. Shorter scan duration translates into a more tolerable breath hold for the patient and subsequently results in a decrease in respiratory and motion artifacts (see Figs. 3.1, 3.2 and 3.3). Hara et al. performed a study comparing respiratory artifacts, colonic distention, and polyp detection at CTC by using single- and multidetector row helical CT systems.2 Seventy-seven patients underwent CTC with single-detector CT and 160 patients were scanned on MDCT followed by optical colonoscopy. Mild respiratory artifacts were identified in 61% of patients who were scanned on single-detector CT compared with only 16% of patients who underwent MDCT. Similarly, there was a statistically significant larger number of patients with suboptimal colonic distention with single-detector CT involving at least one colonic segment in 52% of examinations versus only 16% of multidetector row CT examinations. There was no statistically significant difference in the sensitivity for detection of large polyps comparing single-detector CT versus MDCT at 89% (8/9) versus 80% (8/10) respectively although it was noted that there were a relatively small number of large polyps in each group.
SECTION THICKNESS
The acquisition of thin sections allows for less partial volume averaging and improved image quality of the multiplanar reformatted views and the three-dimensional (3D) endoluminal images. This has been evaluated in both phantom models and patient studies. An early study by Power et al. evaluated a phantom containing 10 spherical polyps between 1 mm and 10 mm in size using single-detector CT.3 The phantom was scanned at slice thicknesses of 3 mm, 5 mm, and 7 mm and various pitches ranging between 1.0 and 2.0. It was found that a slice thickness of 3 mm with a pitch of 2 on single-detector CT provided optimal polyp conspicuity with a relatively low radiation dose. Laghi et al. used a colonic phantom containing 27 simulated polyps of various morphologies to evaluate the optimal scanning technique for CTC using a MDCT scanner.4 Three different scanning protocols were tested—collimation and slice thickness of 1.0 mm, collimation of 2.5 mm with a slice thickness of 3.0 mm, and collimation of 2.5 mm with a slice thickness of 5.0 mm. Sensitivity for detection of lesions was 100% for protocol 1, 96% for protocol 2 and dropped to 85% for protocol 3. There was progressive blurring of polyp borders and worsening of image quality when slice thickness was increased. Increased stair-step and rippling artifacts were identified with increasing slice thickness. On the basis of these results it was recommended that CTC be performed with the use of a high-resolution CT protocol when using a MDCT scanner (1.0-mm effective slice thickness).
Lui et al. performed a study evaluating the effect of various section thicknesses at CTC and results showed improved specificity for thin sections.5 Twenty-five patients
underwent MDCT colonography and colonoscopy. The CT images were reconstructed using a “thin protocol” consisting of 1.25-mm sections reconstructed every 1.0 mm and a “thick method” consisting of 5.0-mm sections reconstructed every 2.0 mm. There was no statistically significant difference in sensitivity for polyp detection comparing thin and thick sections although there were only a total of 12 polyps in this study. However, it was found that the number of false-positive findings was significantly lower for thin sections compared with the thick sections for two readers. Specificity ranged between 80% and 93% for thin sections compared with 73% to 80% for thick sections. Mean interpretation time was significantly longer using thin sections for one reader and was 13 minutes for both thin and thick sections for the second reader.
underwent MDCT colonography and colonoscopy. The CT images were reconstructed using a “thin protocol” consisting of 1.25-mm sections reconstructed every 1.0 mm and a “thick method” consisting of 5.0-mm sections reconstructed every 2.0 mm. There was no statistically significant difference in sensitivity for polyp detection comparing thin and thick sections although there were only a total of 12 polyps in this study. However, it was found that the number of false-positive findings was significantly lower for thin sections compared with the thick sections for two readers. Specificity ranged between 80% and 93% for thin sections compared with 73% to 80% for thick sections. Mean interpretation time was significantly longer using thin sections for one reader and was 13 minutes for both thin and thick sections for the second reader.
With the evolution from single-detector to 4-, 8-, 16- and 64-detector row CT scanners, the collimation and the section thickness used for CTC has decreased. The typical collimation ranges between 3 and 5 mm for single-detector CT with a large percentage of overlap in the data acquisition. For 4- and 8-detector row CT, the collimation is approximately halved and ranges between 1 and 2.5 mm depending upon the specific CT scanner used. The collimation ranges between 0.625 and 1.25 mm for 16-and 64-detector CT (see Table 3.1). The American College of Radiology Practice Guidelines for the Performance of CTC in Adults recommend optimal slice collimation ≤3 mm with a reconstruction interval of ≤1.5 mm.6 A breath hold of 25 seconds or less is suggested. A thicker slice collimation of up to 5 mm with a reconstruction interval of ≤2.5 mm is less preferable.6
RADIATION DOSE
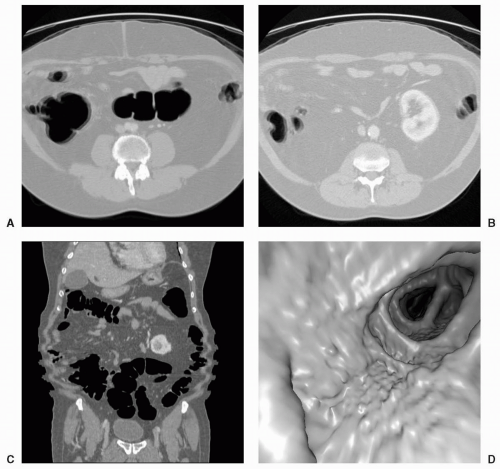
One of the challenges facing CTC particularly as a screening examination is to maintain acceptable radiation
dose to the patient without compromising the diagnostic ability for lesions. The International Commission on Radiological Protection (ICRP) requires that radiation doses to patients are as low as reasonably achievable (ALARA).7 There are multiple factors that affect radiation dose and the image quality of a CT scan. Better image quality is typically associated with increased radiation dose to the patient. Reducing radiation dose decreases the number of photons that reach the detectors and this consequently increases image noise (see Figs. 3.4, 3.5 and 3.6).
dose to the patient without compromising the diagnostic ability for lesions. The International Commission on Radiological Protection (ICRP) requires that radiation doses to patients are as low as reasonably achievable (ALARA).7 There are multiple factors that affect radiation dose and the image quality of a CT scan. Better image quality is typically associated with increased radiation dose to the patient. Reducing radiation dose decreases the number of photons that reach the detectors and this consequently increases image noise (see Figs. 3.4, 3.5 and 3.6).
 Get Clinical Tree app for offline access 
|