Fig. 9.1
Barium swallow showing distal esophageal narrowing, an air-fluid level, and very slow emptying of barium from the esophagus into the stomach
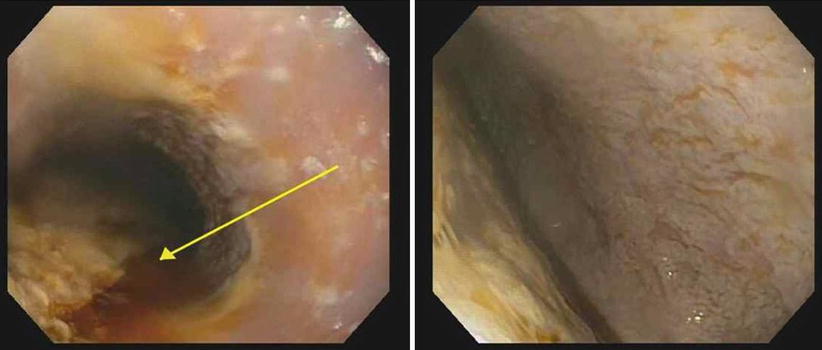
Fig. 9.2
Endoscopy showing retained food in the esophageal lumen (arrow), and confirmation that the distal esophageal narrowing on Fig. 9.1 was not due to a peptic stricture or cancer
Fig. 9.3
Esophageal manometry showing type II achalasia (Chicago classification)
9.2 Operation
9.2.1 Patient Position and Placement of Trocars
The patient was positioned supine on the operating room table and the legs were extended on stirrups. Five trocars were inserted into the peritoneal cavity, as discussed in Chap. 5 (Fig. 9.4). The surgeon performs the procedure standing between the patient’s legs.
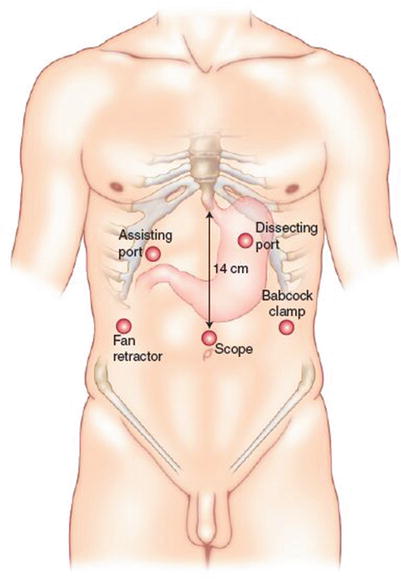
Fig. 9.4
Location of trocars for laparoscopic operations for achalasia
9.2.2 Operative Procedure: Heller Myotomy and Dor Fundoplication
Step 1
Divide the gastrohepatic ligament
The gastrohepatic ligament is divided (Fig. 9.5), beginning above the caudate lobe of the liver, all the way to the right pillar of the crus. An accessory left hepatic artery (from the left gastric artery) is frequently present in the gastrohepatic ligament and should be clipped to have proper exposure.
Fig. 9.5
(a, b) Division of the gastrohepatic ligament
Step 2
Identify the right crus of the diaphragm and posterior vagus nerve
After opening the gastrohepatic ligament, the right pillar of the crus is separated from the right side of the esophagus by blunt dissection (Fig. 9.6). The posterior vagus nerve is identified.
Fig. 9.6
(a, b) Identification of the right crus of the diaphragm and posterior vagus nerve
Step 3
Divide the peritoneum and phrenoesophageal membrane above the esophagus
The peritoneum and the phrenoesophageal membrane above the esophagus are transected with the electrocautery, and the anterior vagus nerve is identified (Fig. 9.7). The left crus of the diaphragm is dissected downward toward the junction with the right crus.
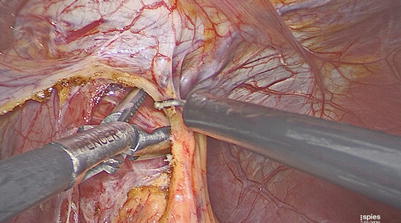
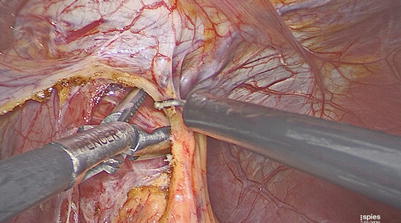
Fig. 9.7
Division of peritoneum and phrenoesophageal membrane above the esophagus
Step 4
Divide the short gastric vessels
The short gastric vessels are divided using a bipolar instrument (Figs. 9.8 and 9.9). This step allows full mobilization of the fundus of the stomach to avoid any tension when the partial fundoplication is constructed.
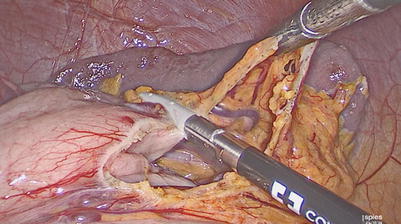

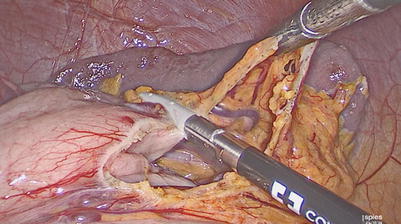
Fig. 9.8
Division of short gastric vessels

Fig. 9.9
Division of short gastric vessels
Step 5
Perform esophageal dissection in the mediastinum
Using the bipolar instrument, further dissection is done in the posterior mediastinum in order to have about 4 cm of esophagus below the diaphragm without any tension (Figs. 9.10 and 9.11). No posterior dissection is performed.
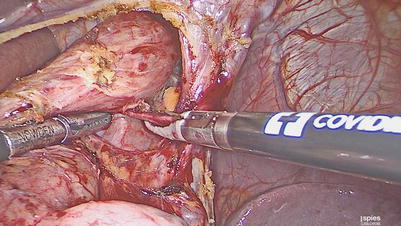
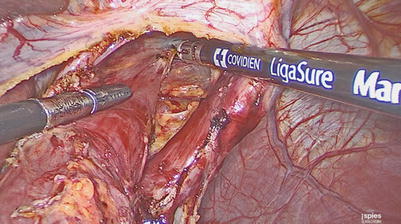
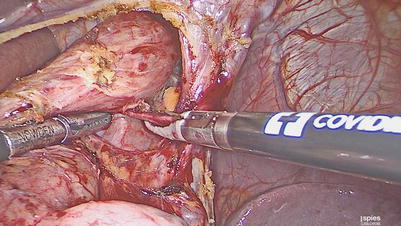
Fig. 9.10
Esophageal dissection in the mediastinum
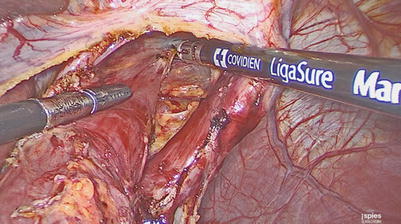
Fig. 9.11




Esophageal dissection in the mediastinum
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








