Chapter 45 NUTRITION IN PATIENTS WITH LIVER DISEASE
NUTRITIONAL ASSESSMENT IN CIRRHOSIS
Protein–energy malnutrition
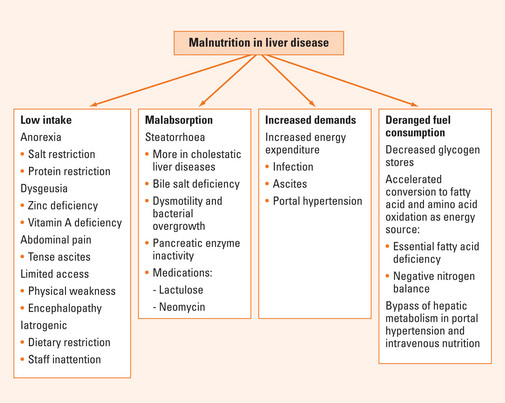
Multiple factors may be involved in the development of PEM in advanced liver disease (Figure 45.1). Inadequate dietary intake has been described in up to 87% of patients. This may be caused by anorexia and dysgeusia, which may be related to zinc and vitamin A deficiencies. Commonly prescribed salt and protein dietary restrictions may also affect appetite. In addition, patients with large ascites may experience early satiety and abdominal pain, limiting food intake, and generalised weakness and encephalopathy may limit physical access to adequate intake. In the hospital, deficient intake is commonly iatrogenic. Malabsorption may be another factor contributing to PEM. Steatorrhoea has been reported in both cholestatic and non-cholestatic liver disease and may be caused by decreased intestinal bile salt pool, pancreatic insufficiency and bacterial overgrowth associated with impaired intestinal motility. The use of lactulose and neomycin in encephalopathy may exacerbate malabsorption. It has been suggested that increased nutritional requirement may exacerbate malnutrition in cirrhosis. However, studies comparing measured energy expenditure using indirect calorimetry and that calculated by Harris Benedict equations (Table 45.1) suggest the presence of large variability among patients with cirrhosis, with both hypermetabolism and hypometabolism equally observed in about one-third of patients (more than 20% discrepancy). Of significance, patients with increased energy expenditure experienced increased rates of morbidity and mortality. The mechanism of hypermetabolism in some cirrhotic patients may be related to infection, ascites and portal hypertension. Both the removal of ascites and the reduction of portal hypertension by transjugular intrahepatic portosystemic shunt (TIPS) have been associated with reduction of energy expenditure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree