Neutropenic Enterocolitis (Typhlitis)
Neutropenic enterocolitis, also known as typhlitis, agranulocytic colitis, neutropenic enteropathy, and ileocecal syndrome,
traditionally affects children treated for leukemia and other conditions. It may complicate chemotherapy for solid tumors (377). However, the disorder also affects healthier, nonterminal, neutropenic children and adults with solid tumors and other conditions including AIDS. The incidence of neutropenic colitis is increasing, particularly in patients with acute myelogenous leukemia undergoing high-dose cytosine arabinoside chemotherapy. Although direct mucosal cytotoxicity from cytotoxic drugs may contribute to the disorder, it is not a prerequisite for neutropenic enterocolitis to occur.
traditionally affects children treated for leukemia and other conditions. It may complicate chemotherapy for solid tumors (377). However, the disorder also affects healthier, nonterminal, neutropenic children and adults with solid tumors and other conditions including AIDS. The incidence of neutropenic colitis is increasing, particularly in patients with acute myelogenous leukemia undergoing high-dose cytosine arabinoside chemotherapy. Although direct mucosal cytotoxicity from cytotoxic drugs may contribute to the disorder, it is not a prerequisite for neutropenic enterocolitis to occur.
Most patients are profoundly granulocytopenic, with their neutrophil count measuring <500 to 1,000 cells/mm3. Patients are typically neutropenic for at least a week before symptom onset (378). Patients usually present with a dramatic onset of fever, watery or bloody diarrhea, right abdominal quadrant pain, abdominal distention, rebound tenderness, nausea, and vomiting (378). The presence of fever, rigors, and shock suggest the development of sepsis or colonic perforation. The disorder is often fatal unless aggressively treated, usually with resection of the involved bowel segment. Mortality rates range between 5% and 100% and average 40% to 50%. Death results from cecal perforation, bowel necrosis, and sepsis.
The pathogenesis of the syndrome is illustrated in Figure 13.134. The chemotherapy damages the GI mucosa by destroying the rapidly dividing epithelium. Alternatively, mucosal neoplastic infiltrates may cause breaks in the mucosal barrier. Loss of mucosal integrity coupled with the neutropenia allows bacteria to invade the bowel wall and sepsis to develop. In children, the infections usually result from Pseudomonas or E. coli, whereas in adults C. septicum is the most common infecting organism. Ischemia also plays a role in the genesis of the lesion. The ischemia likely results from vascular invasion by bacteria or the production of bacterial toxins followed by the development of a disseminated intravascular coagulopathy. One often sees small thrombi within the mucosal and submucosal capillaries. Other causes of ischemia include perivascular neoplastic infiltrates, episodes of hypotension following sepsis, or mucosal hemorrhage complicating severe thrombocytopenia or the presence of angioinvasive fungi. The process preferentially involves the cecum due to the luminal stasis that occurs at this site. The relatively poor vascular supply of the cecum further predisposes to ischemic injury. Rarely, other bowel segments become involved.
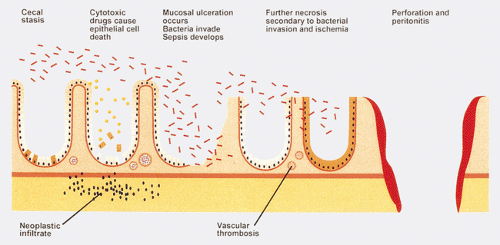 FIG. 13.134. Pathogenesis of neutropenic enterocolitis (see text).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





