Fig. 3.1
Neurotransmitter mechanisms regulating urinary bladder and EUS function. Distribution of different autonomic and somatic axons
The afferent Aδ fibers, lightly myelinated, and the unmyelinated C fibers travel through pelvic and hypogastric nerves. While Aδ fibers respond to active contraction and passive distension, conveying information about bladder filling, C fibers are insensitive to bladder filling under physiological conditions and activated only in pathological conditions.
These fibers convey nociceptive, volume, and tension information in the somatosensory pathways from the sacral dermatomes through the spinal cord to the CNS. The activity of volume and tension mechanoreceptors during bladder filling is conveyed to the dorsal horns by the pelvic nerves. A rostral intersegmental pathway projects to the thoracolumbar cord, stimulating sympathetic preganglionics, thus promoting continence via the hypogastric nerves. The persistence of low detrusor pressure, the absence of involuntary contractions, and the increased pressures at urethral level are the result of storage reflexes. Pelvic organ afferents can inhibit the sacral preganglionics to the bladder and induce increased urethral pressure. This guarding reflex is known as visceral-visceral reflex. This fact explains the possible therapeutic utility of intravaginal electrostimulation in the treatment of urgency-frequency syndrome. Another guarding reflex exists, in which afferents from pelvic organs and bladder filling stimulate ON to increase the outlet urethral resistance.
Urinary bladder and the other functional unit consisting of bladder neck, urethra, and EUS are controlled and regulated by various central neural circuits, involving midbrain periaqueductal gray (PAG), cell groups in the preoptic and caudal hypothalamus, pontine micturition center (PMC), also known as Barrington nucleus, and medial frontal cortex. PMC is activated during voiding (M-region) and bladder filling (L-region or pontine storage center) and appears to initiate and coordinate lower urinary tract function. This notion is supported by neurophysiological data; moreover, PET scanning of the human brain during micturition documents increased metabolic activity in the pons as well as in cortical and subcortical areas, giving further evidence for pontine involvement in urinary storage and release (Fig. 3.2).
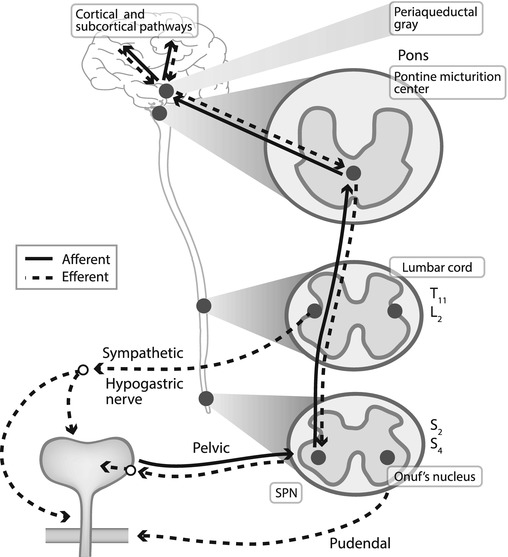
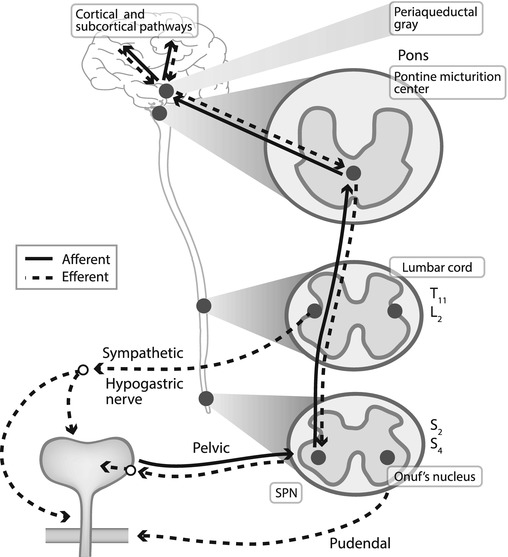
Fig. 3.2
Central and peripheral pathways involved in functional neural control of the urinary tract
The cortical (prefrontal cortex, insula, anterior cingulate cortex, cerebellum), subcortical (basal ganglia, thalamus, hypothalamus), and pontine circuitry accomplishes three major functions: amplification of bladder contraction to allow complete micturition, control of micturition frequency, and coordination of the activity of lower urinary tract muscles (Fig. 3.3). Overlapping between voluntary control and a reflex mechanism is allowed by sympathetic, parasympathetic, and somatic peripheral innervation of bladder and urethra. Higher centers in the CNS induce a modulatory effect over PMC, primarily mediated by an inhibitory input. The PMC appears to initiate and coordinate lower urinary tract function, pairing detrusor contraction with inhibition of urethral outlet, while sacral micturition center triggers an involuntary reflex detrusor contraction in response to bladder filling. In fact, two distinct voiding reflex pathways exist: a suprasacral reflex physiologically active in normal subjects and a sacral reflex which allows voiding in pathological conditions.
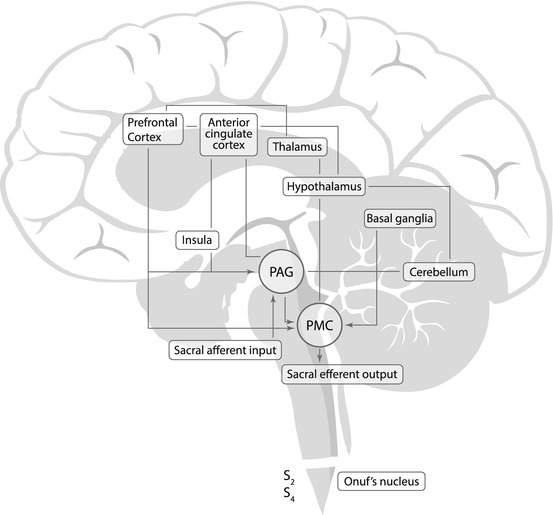
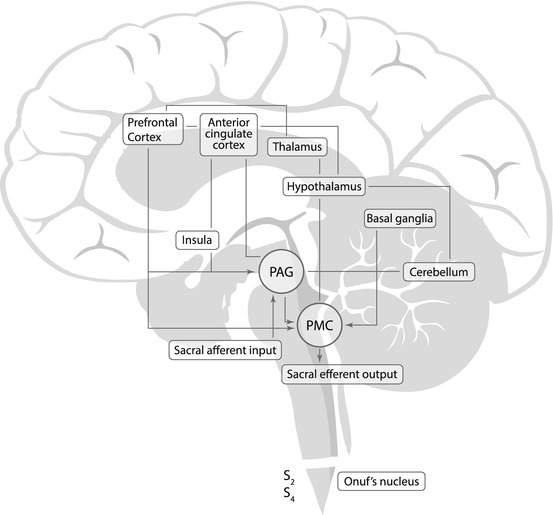
Fig. 3.3
Scheme of the neural interconnections between different cortical and subcortical areas involved in urinary storage and release
Such an anatomo-functional complexity allows to define urinary continence, as suggested by C.J. Fowler, “a severe test of neurological integrity” [1].
In fact, neurogenic lower urinary tract (LUT) disorders are neuroanatomically divided into suprapontine, spinal (infrapontine-suprasacral), sacral, and peripheral, showing different patterns of voiding dysfunctions. Based on knowledge of voiding centers, these different clinical features can be explained. The suprapontine, supraspinal neurological lesion induces a detrusor hyperreflexia with normal sphincter synergy (DHSS), caused by the loss of inhibition of sacral micturition center. The patient with DHSS has a volume trigger point, at which the bladder contracts, which is considerably lower than the normal bladder capacity, complaining urinary frequency, urgency, and incontinence. Spinal (infrapontine-suprasacral) lesions induce a disruption of connections between the PMC and the sacral center, causing loss of PMC activity and subsequent loss of coordinated relaxation of the EUS during bladder contraction. This loss results in detrusor sphincter dyssynergia (DSD), paired with detrusor hyperreflexia (as with suprapontine, supraspinal lesions) due to uninhibited bladder contractions. DHSS and DSD are dangerous pathological conditions, commonly leading to upper urinary tract damages, reflecting high intravesical pressures needed to obtain urinary flow, progressively impairing kidney function to the point of kidney failure.
Those with suprasacral injuries and intact bladder sensation usually complain of urgency-frequency syndrome; incontinence without awareness may be shown.
Patients with sacral lesions usually complain of suprapubic fullness, inability to void, and incontinence. Traumas are the most common cause responsible for conus and cauda equina lesions. Clinical findings reflect urinary retention with overflow incontinence and elevated post-void residual (PVR).
Peripheral nerve lesions may involve parasympathetic, sympathetic, and/or somatic nerves.
Usually, parasympathetic involvement results in detrusor areflexia; large bladder capacities and chronic bladder overdistension with increased PVR may be seen in case of motor and sensory nerve impairment. Sympathetic lesions alone may cause incontinence due to impaired internal sphincter closure. Patients with peripheral nerve diseases usually complain of suprapubic fullness and inability to void, showing urodynamic findings of detrusor areflexia.
Urinary symptoms and signs may differ from expectations because of incomplete suprapontine, spinal, sacral, and peripheral lesions, coexisting involvement of central and peripheral neurological pathways or other factors, such as drugs, prostate obstruction, or cognitive impairment.
3.2 Neural Control of Intestinal Tract
Bowel activity and secretion in the gastrointestinal (GI) tract are connected and modulated by the cortical activity and controlled by intrinsic and extrinsic GI innervation of smooth muscle layers and glands. Intrinsic innervation relays on the enteric nervous system (ENS), which is the largest nerve cells accumulation outside the brain, having about 100 million neurons and extending throughout the length of GI tract. The neurons of the ENS are organized into two plexuses, myenteric or Auerbach plexus, between the longitudinal and circular smooth muscle layers, and submucosal or Meissner plexus, that influences the absorptive and secretory functions of the enteric mucosa. Extrinsic innervation depends on parasympathetic and sympathetic preganglionics. Sympathetic output originates in the prevertebral ganglia, while parasympathetic innervation is allowed by dorsal motor vagal nucleus (DMV) of the medulla oblongata and sacral parasympathetic nucleus of the spinal cord.
Despite the close anatomical relationship between the rectum and anal canal, there are clear differences in their innervation. Afferent innervation of the rectum derives from the pelvic nerve (Aδ and C fibers), sensitive to rectal distension. Aδ fibers rapidly adapt to changes in rectal distension, while C fibers are slowly adapting and respond to the intensity of rectal distension [2]. Sensations from the rectum can be poorly localized, while the high density of afferent pathways and receptors in the anal canal allows localization of the sensations and sensory definition of the quality of content.
The motor control of anorectum and pelvic floor results from parasympathetic, sympathetic, and somatic nerves. Parasympathetic pathways originate from the parasympathetic nucleus located at S2–S4 segments, having both excitatory and inhibitory components. The excitatory part induces colonic propulsive activity during defecation, while the inhibitory part permits adaption of colonic volume to the content and relaxation of the colon ahead of fecal material.
Rectoanal inhibitory reflex, consisting of anal relaxation, induced by rectal distension, is mediated by a nitric oxide pathway involving intrinsic nerves. Tonically active sympathetic excitatory neurons that innervate internal anal sphincter allow closure of the anal canal at rest. Anal sphincter and pelvic floor somatic innervation originates from Onuf’s nucleus motor neurons at S2–S4 levels. The external anal sphincter (EAS) contributes 30–50 % of resting anal tone, while internal anal sphincter (IAS), regulated by sympathetic nerves, provides most of the resting anal pressure. The puborectalis muscle (PRM) is, moreover, tonically active and permits maintenance of the resting anorectal angle. PRM contraction in fact is fundamental to preserve fecal continence, and its relaxation is necessary for normal bowel emptying. The rectum is functionally different from colon because of its function as a reservoir opposed to a transit function. The rectal compliance is the adaptive capacity of this reservoir to increase its distension to luminal content.
Small volumes of feces propulsed slowly to an almost empty rectum result in an increased rectal compliance, while rapid and large masses distending the rectal wall induce activation of rectoanal inhibitory reflex and the desire to void.
Defecation is mediated by a coordinated relaxation of pelvic floor, IAS and EAS, and an increase in rectal pressure. However, evidence is emerging of an existing association between symptoms of impaired defecation and psychological state.
Gastrointestinal symptoms are also the most important non-motor manifestation of Parkinson disease (PD) and parkinsonism, with constipation as the most prominent manifestation resulting from poor colonic peristalsis and defecatory dysfunction [3]. A wide pattern of cortical areas is involved in anorectal stimulation, including areas that process cognitive and affective aspects of sensation (prefrontal cortex, anterior cingulate cortex and insula) and areas activated during spatial discrimination (primary and secondary somatosensory cortex). Anal canal stimulation results in activation of similar cortical areas than those involved during rectal stimulation, but the former results in activation at a more superior level of primary somatosensory cortex without anterior cingulate cortex activation. It seems that viscera have a greater limbic cortex representation than somatic structures, thus explaining the greater autonomic responses evoked by visceral sensation in comparison with somatic sensation [4].
3.3 Neurophysiological Evaluation of Pelvic Floor
Neurophysiological evaluation of patients affected by urinary, fecal, and sexual disorders usually follows surgical and clinical evaluation and, almost always, other investigations. Although neurophysiological investigations are performed worldwide, their application to pelvic floor disorders is limited to a few centers. In patients with pelvic floor disorders, EAS EMG is the single most useful diagnostic test, particularly for focal sacral lesions. EAS muscle is, in fact, readily accessible and evaluated without discomfort. However, no consensus statement for a standardized approach to LUT and anorectal neurogenic disorders has been reached, and the role of different tests has not been clearly defined yet.
Clinical history and neurological examination should always be performed to propose a diagnosis of neurogenic pelvic dysfunction and to plan further electrophysiological tests [5, 6]. Examination usually includes anal sphincter tone, strength in the S1–S2 innervated muscles (gastrocnemius, gluteal muscles), sensation extending from the soles of the feet to the perianal area, and presence of anal and bulbocavernous reflexes. Anal reflex is induced by pricking or scratching the perianal skin area, whereas bulbocavernosus reflex is evoked by a nonpainful clitoral or gland squeeze [7, 8]. Clinically elicited reflexes may be extinguished by mild or severe nerve lesions, whereas the same reflexes can be recorded neurophysiologically, though with a prolonged latency and reduced amplitude, also in almost complete nerve lesions.
Extensive neurophysiological investigations should be performed in any patient with LUT and anorectal disorders of suspected central or peripheral neurogenic etiology. These tests include concentric needle EMG of different pelvic floor muscles, measurement of sacral reflex latency (pudendo-anal or bulbocavernosus reflex) [9], pudendal and anal somatosensory-evoked potentials (SEPs), and motor-evoked potentials (MEPs) from pelvic floor and EAS muscles by transcranial and lumbosacral magnetic stimulation. Pudendal nerve terminal motor latency (PNTML) has been used in different clinical conditions, but its clinical value has been questioned because the reproducibility, sensitivity, and specificity are uncertain. The recording of a sympathetic skin response (SSR) from the saddle region is useful for testing the lumbosacral autonomic sympathetic system. Unfortunately, a clinically useful test for evaluating the sacral parasympathetic system, which is crucial for LUT and anorectal functioning, has not been found yet.
Tests are usually capable of demonstrating neuropathic lesions and helping to define the specific affected sensory, motor, or autonomic pathway. Severity of lesions can be also assessed, and the underlying mechanisms can be revealed. Even when all other functional tests do not show altered findings, the electrophysiological tests can be positive, therefore leading to a surgical or conservative approach and assessing the prognosis.
3.3.1 Electromyography (EMG)
Needle EMG is the most important neurophysiological technique for evaluating patients with suspected neurogenic etiology of pelvic floor dysfunction [10]. EMG assessment of the pelvic floor, EAS, and EUS muscles is mainly indicated to evaluate: (1) the presence of pathological spontaneous activity, fibrillation potentials and positive sharp waves, and denervation of muscle fibers, (2) the presence of muscle fiber reinnervation [11], (3) normal mild continuous tonic contraction in the EAS, PRM [12], and EUS and adequate contraction or relaxation during squeeze or straining, and (4) recruitment pattern and motor-unit potential (MUP) waveform [13]. It is sometimes difficult to discriminate MUPs from fibrillation potentials and positive sharp waves in partial denervation of sphincter muscles during relaxation; in this case, the needle evaluation of bulbocavernosus muscle is useful as no ongoing activity of motor units is recorded [14]. The most important parameters in the analysis of MUP are amplitude, duration, area, number of phases and turns, and firing rate that can be automatically evaluated by advanced EMG systems provided with special software of analysis.
However, in the EAS muscle the best diagnostic parameters seem to be MUP duration, area, and number of turns [15]. Completely or partially denervated pelvic muscles may be reinnervated by axonal regrowth from the proximal nerves; thus a recording of bi and triphasic motor units, soon becoming polyphasic with prolonged duration, can be shown. The EAS muscle needle EMG examination is the test most commonly used to assess the functional state of pelvic floor and sacral myotomes; in fact EAS is easy to access, its needle evaluation is not very painful and very useful information can be acquired. EAS examination holds the central position in Podnar and Vodusek’s algorithm for electrodiagnostic evaluation of the sacral nervous system [6]. With the patient in a comfortable Sims position with knees and hips flexed, after grounded electrically at the thigh, a standard concentric needle EMG electrode is inserted into the subcutaneous portion of the EAS muscle to a depth of 3–5 mm under the mucosa, 1 cm from the anal orifice [6, 16]. Both left and right halves of the subcutaneous EAS muscle must be examined separately, starting on the side with the clinical evidence of sphincter dysfunction (episiotomy scar tissue, patulous anus). If partial or complete atrophy of the subcutaneous EAS muscle is appreciated, a concentric needle electrode can be introduced 1–3 cm deeper through the skin to evaluate spontaneous activity, recruitment pattern, and functional contractile capacity of the deeper EAS and 4–5 cm deeper for examination of the PRM. In the presence of fibrosis, there is a loss of pelvic floor muscle contractile capacity, and consequently, no spontaneous activity or MUP is recognized. When the needle advances in the EAS muscle, continuous firing of low-threshold MUPs is normally appreciated, and during a brief period of relaxation, the presence of spontaneous activity, fibrillation, or jasper potentials can be recorded.
EMG recordings from the EAS are performed at rest and during squeezing, coughing, and straining that simulates rectal evacuation. In healthy subjects, squeeze and cough increase the MUP recruitment pattern, whereas strain decreases or inhibits MUP firing.
Needle examination of the bulbocavernosus muscle is indicated when no EMG signals are recorded in the subcutaneous or deeper EAS muscles [17].
Kinesiological EMG (KEMG) is used to assess and record patterns of individual anterior or posterior muscles during functional maneuvers. An abnormal pattern during bladder filling or emptying, anal closure, squeezing, coughing, and straining can be recorded by surface or needle electrodes. The utility of this technique is to reveal possible dyssynergic contraction pattern of EUS concomitant with detrusor contraction (during urodynamic test) and analogous inappropriate PRM activation on attempt of evacuation. In patients with anal incontinence, during manometric balloon retaining test, KEMG can show absent or insufficient EAS activation.
3.3.2 Sacral Reflexes
Sacral reflexes are motor responses, derived from pelvic striated floor and sphincter muscles, to electrical stimulation of the dorsal penile or clitoral nerve, perianal skin, bladder neck, or proximal urethra. Sacral reflexes evaluate the functional status of the afferent neural fibers of the clitoris or penis, the S2–S4 spinal segments, and the efferent pathways to EAS and bulbocavernosus muscles [7, 9, 18]. The central circuit at the spinal level is complex and probably involves many sacral interneurons.
The motor response in EAS and BC muscle is recorded either with a concentric needle or wire electrodes and can be analyzed separately for each side of both muscles. These sacral reflexes, named pudendo-anal and bulbocavernosus reflex, reveal two components with different thresholds at the electrical stimulation: a first component with a shorter latency of 28–45 ms, probably oligosynaptic, and a second component with a longer latency at about 50–75 ms, typical for a polysynaptic response (Fig. 3.4). The first component is morphologically constant, is stable, and does not habituate, while the second component or long latency response is not always demonstrable and rapidly habituates [19]. The cutaneoanal reflex, described in 1891 by Rossolimo, like the other two reflexes consists of two or three motor contractions (early response at 5 ms, intermediate at 15 ms, and late at about 50 ms) of EAS muscle in response to scratching or pricking the perianal skin. This reflex, which is abolished by transection of the posterior S4 roots, shows marked habituation, is quite variable (35–80 ms), and therefore cannot be used as a diagnostic tool [20].
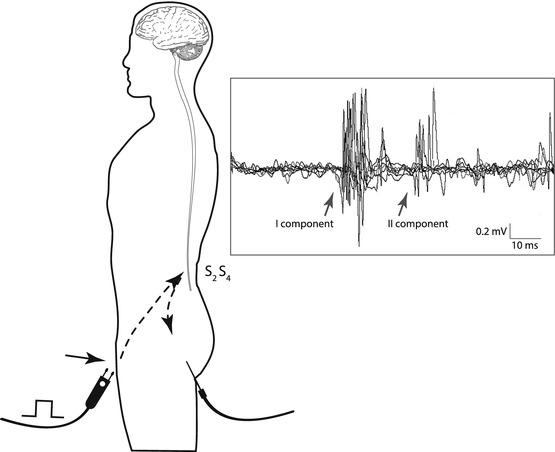
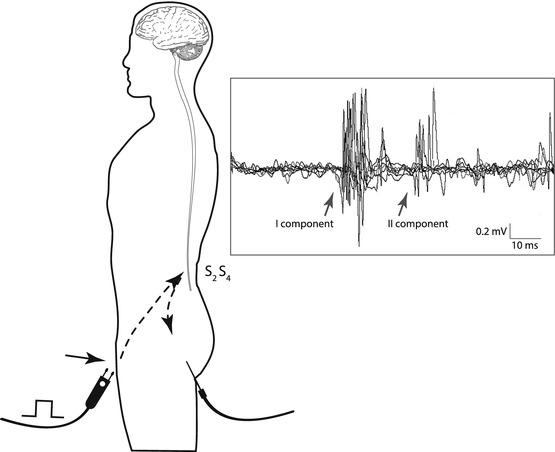
Fig. 3.4
Neurophysiological recording of the pudendo-anal reflex elicited in a healthy man by single electrical stimulation of the dorsal penile nerve. Responses are recorded by a concentric needle electrode inserted in EAS muscle. Note the two different components of the sacral reflex
Vesicourethral and vesico-anal reflexes are described following stimulation of the bladder neck and mucosa, but their usefulness as a diagnostic tool is considered to be limited.
Recently, a technique for transcutaneous electrical stimulation of the S3 motor root, recording from EAS muscle, has also been described [21].
Method: A common scheme of sacral-evoked responses consists in the anterior electrical stimulation (penile/clitoral, bladder neck site) and recording by needle electrode from different pelvic muscles (BC, EAS, levator ani). Sacral reflexes are useful in different pelvic floor disorders and have been recommended for the assessment of cauda equina, conus, and medullaris lesions. In the presence of unilateral/asymmetrical lesions of pudendal nerves, sacral roots, or lumbosacral plexus, these reflexes may show a reduction of responses amplitude and/or increased latencies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





