Fig. 17.1
Left lateral decubitus positioning for thoracoscopy
We employ a four-port or five-port thoracoscopy, minimizing the use of 10-mm trocars to decrease the risk of intercostal nerve bundle injury (Fig. 17.2). In lieu of 10-mm port sites, we use small wound protectors. Our trocar placements are the following:
1.
Fifth intercostal space, anterior axillary line: 1-cm incision with a wound protector, used for a 30° camera and retracting instruments
2.
Third intercostal space, anterior axillary line: 2.5-cm incision with a wound protector, utilized for the Osugi retractor and suctioning device
3.
Fourth and seventh intercostal spaces, posterior axillary line: two 5-mm operating ports
Fig. 17.2
(a) Trocar sites for thoracoscopy. (b) Use of an Osugi retractor facilitates lung retraction through wound manager
After the patient is placed in reverse Trendelenburg with slight rotation anteriorly, mobilization of the thoracic esophagus is performed from the thoracic inlet to the diaphragm, and infracarinal mediastinal lymph node dissection is completed (Fig. 17.3). Retraction of the lung and airway is facilitated with an Osugi retractor. The pleura is initially divided anteriorly and posteriorly along the length of the esophagus with hook cautery, using an atraumatic grasper to provide tension on the esophagus. Further dissection is completed with a harmonic scalpel, and a Penrose drain is used to encircle the esophagus to provide countertraction. Dissection with energy devices near the trachea is performed with great care, as inadvertent injury may result in airway fistulization. The azygous vein is circumferentially dissected and divided with an Endo GIA™ stapler (Covidien, Minneapolis, MN) at the level of the carina. ENDOLOOP® ligatures (Ethicon, Somerville, NJ) are placed on each end of the divided azygous vein and retracted through the chest wall with a suture passer to increase exposure of the mid and upper mediastinum.
Fig. 17.3
(a) Esophageal mobilization. (b, c) Subcarinal dissection
Once the esophagus is fully mobilized from the thoracic inlet to the diaphragm, with all nodal tissue swept into the specimen, it is divided at a level proximal to the tumor, usually cephalad to the azygous vein, consequently also dividing the vagi below the bifurcation of the recurrent laryngeal nerves with a single firing of the Endo GIA™ stapler (Fig. 17.4). The proximal and distal margins are secured to a common umbilical tape to facilitate retrieval via the neck and laparoscopy. The chest is copiously irrigated and a large-capacity closed suction drain (Jackson-Pratt) is inserted in lieu of a chest tube (Fig. 17.5). The trocar sites are closed in layers, and the double-lumen endotracheal tube is exchanged for a single-lumen tube to enhance mobility of the airway during the cervical portion of the operation.
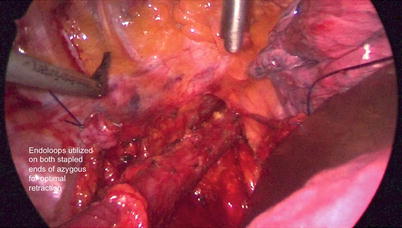

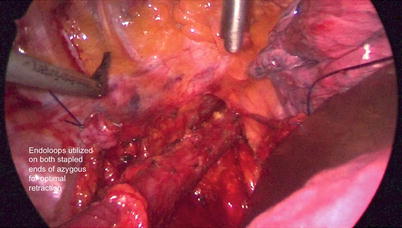
Fig. 17.4
Completion of thoracoscopy

Fig. 17.5
Use of large-capacity Jackson-Pratt drains in lieu of chest tubes
The patient is repositioned in the supine, split-leg position for laparoscopy. The neck is extended, with a roll placed between the scapula. A five-port laparoscopy is employed (Fig. 17.6): A 10-mm Hasson port is placed supraumbilically, a 12-mm port is placed in the left upper quadrant mid-clavicular line, a 5-mm port in the left costal margin for operating instruments, a 5-mm port in the right flank for the liver retractor, and a 5-mm operating port in the right upper quadrant at the midclavicular line. A 5-mm, 30° camera is employed.
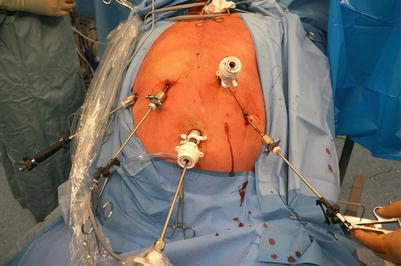
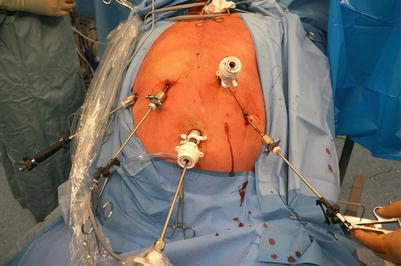
Fig. 17.6
Port placement
The gastrohepatic omentum is opened and the right and left crura are circumferentially dissected without complete division of the phrenoesophageal membrane, in order to preserve pneumoperitoneum.
We perform a complete D2 celiac lymph node dissection by skeletonizing the splenic artery, the hepatic artery, and the splenic vein (Fig. 17.7). The left gastric pedicle is dissected, skeletonized, triplely clipped, and divided. We do not staple the left gastric pedicle, as it may provide an inadequate lymph node dissection. All lymph node–bearing tissue is included with the specimen (Fig. 17.8). We also proceed along the entire celiac axis down to the aorta to include the periceliac lymph nodes en bloc with the specimen.
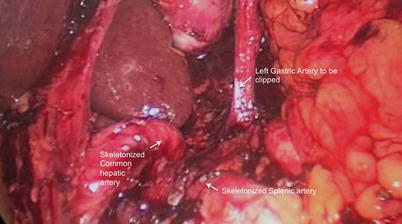

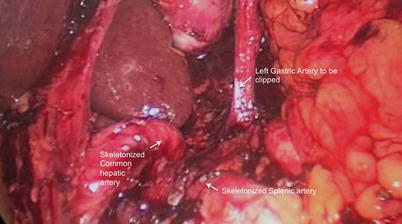
Fig. 17.7
D2 dissection and dissection of the left gastric pedicle to be divided

Fig. 17.8
Completed D2 dissection demonstrating skeletonized hepatic and gastroduodenal arteries
The greater curve is dissected after creation of a window in the gastrocolic omentum, and the lesser sac is entered. Dissection proceeds 5 cm from the greater curvature, with extreme caution taken to preserve the gastroepiploic arcade, the dependent blood supply to the future conduit (Fig. 17.9). The retrogastric attachments are freed and dissection is carried up to the left esophageal hiatus. A Kocher maneuver is completed, with adequate mobilization of the pylorus ensured by testing its extension to the caudate lobe or right crus. After ensuring satisfactory hemostasis, the esophageal hiatus is completely mobilized and the phrenoesophageal membrane is divided.