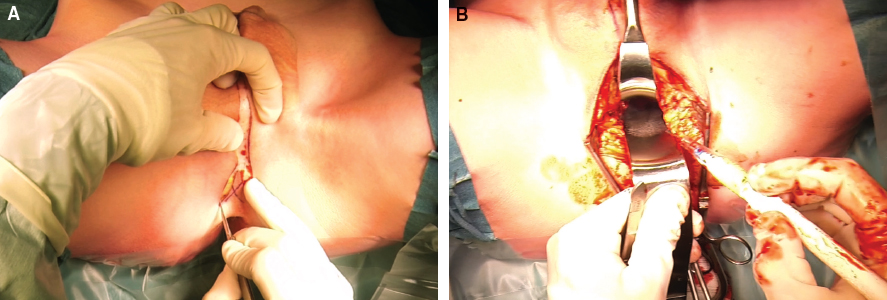
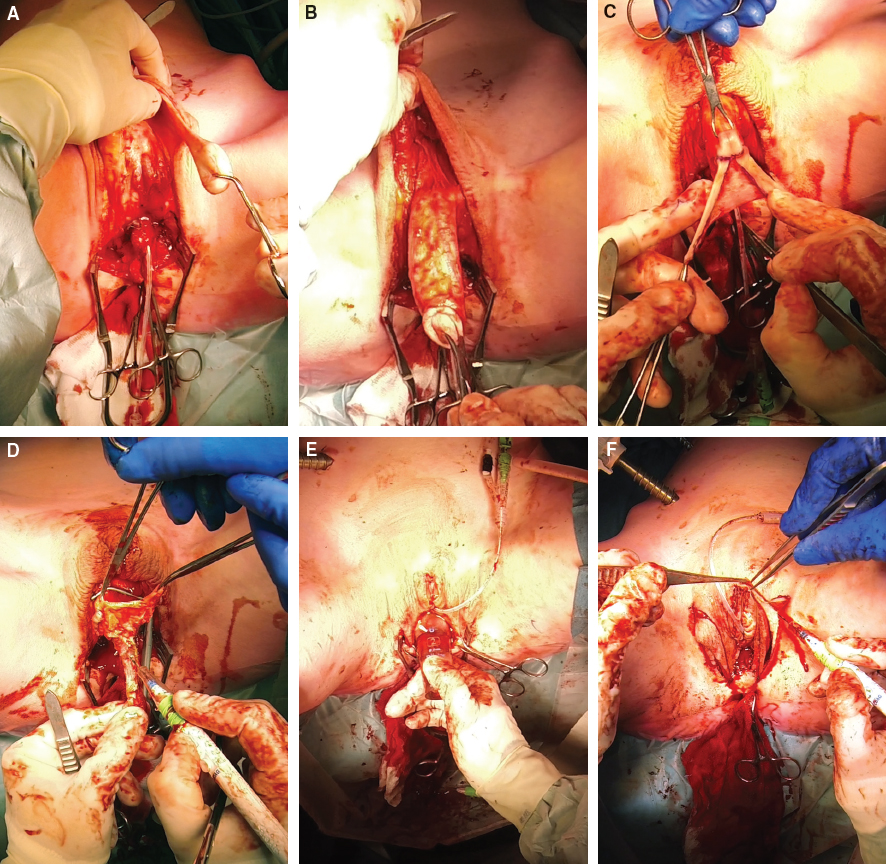
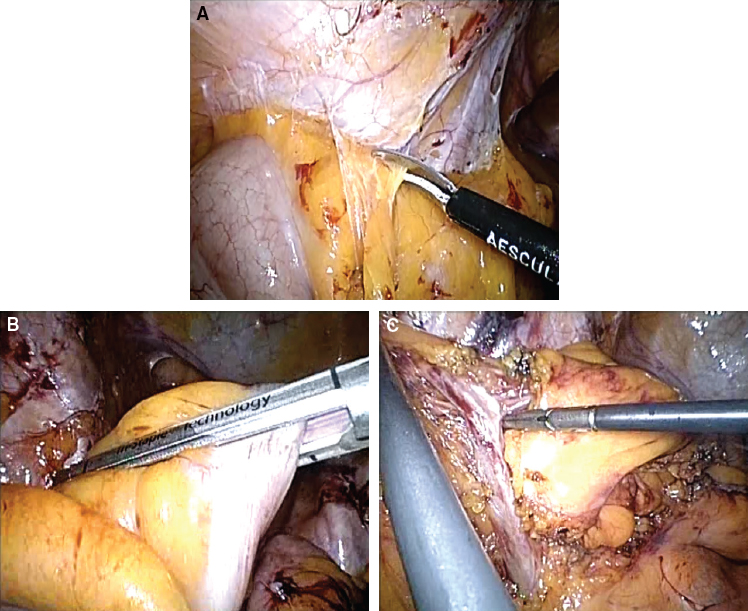
CHAPTER 6 Vaginal reconstruction is of major importance for the psychological and sexual well-being and quality of life in transgender women and biologic women with congenital or postablative absence of the vagina.1 Different types of grafts can be used in vaginoplasty, each of which has its own advantages and disadvantages.2 The advantages of intestinal vaginoplasty are providing sufficient vaginal depth, self-lubricating, and a lesser tendency to shrink.2.3 However, the disadvantages are the need for intestinal surgery and bowel anastomosis with concomitant risks. In this chapter we will focus on the surgical technique for primary total laparoscopic sigmoid vaginoplasty. Secondary laparoscopic intestinal vaginoplasty will also be discussed. There are three distinct groups of patients with indications to undergo total laparoscopic sigmoid vaginoplasty: 1. Transgender women with penoscrotal hypoplasia: These are transgender women who cannot undergo penile-inversion vaginoplasty because of a lack of sufficient penile skin. Penile and scrotal hypoplasia, which is potentially caused by puberty inhibition and subsequent cross-sex hormonal treatment and/or previous circumcision, may cause such a shortage. 2. Transgender women with a failed primary vaginoplasty: This group includes patients who previously underwent vaginoplasty, which failed to provide sufficient neovaginal depth; for example, as a result of total or partial neovaginal stenosis. These patients are eligible to undergo laparoscopic sigmoid vaginoplasty as a revision or redo vaginoplasty. 3. Biologic women with either acquired or congenital absence of a functional vagina: Genital trauma or vaginal surgery for malignancy can result in acquired vaginal absence. Congenital vaginal absence is observed in patients with Mayer-Rokitansky-Küster-Hauser syndrome, androgen insensitivity syndrome, gonadal dysgenesis, bladder exstrophy, hermaphroditism, and common urogenital sinus syndrome. Contraindications, although relative, include an inability to safely undergo general anesthesia, a history of intestinal malignancy, inflammatory bowel disease, extensive abdominal surgery, smoking, and obesity (BMI greater than 30 kg/m2). If laparoscopic intestinal vaginoplasty is performed by an experienced team with the right medical infrastructure and laparoscopic equipment, successful and reproducible results can be achieved. This includes preoperative screening of patients by a specialized psychologist in the gender field. This approach requires two surgeons in different surgical fields, working simultaneously on the same patient. The laparoscopic portion can only be performed by a surgical expert in advanced laparoscopy, and the genital portion is done by a gender surgeon with vast experience in vaginoplasties. For the laparoscopic procedure, we use basic laparoscopic instruments, including bowel graspers and a needle driver. Regarding the devices, these should at least include an HD camera and screen, 30-degree optics, and a range of laparoscopic staplers and a sealing device. Preferably, we use three-dimensional cameras/screens and goggles. An infrared camera system in combination with a preoperative injection of indocyanine green can also be of great help in identifying the vascular anatomy, especially in obese patients. It is recommended that a specialized psychologist with experience in the gender field perform an assessment of psychological eligibility for transgender women to undergo surgery. This also includes sexual history to establish the patient’s postoperative sexual expectations and desires. Sigmoid intestinal vaginoplasty is not indicated for patients who merely wish a feminine genital appearance and do not desire penile neovaginal penetration. Both the plastic surgeon and laparoscopic gastrointestinal surgeon assess surgical eligibility and obtain informed consent for the procedure. If one third or less of the desired vaginal depth can be covered with inverted penile skin, intestinal vaginoplasty is indicated. Patients should be informed about the surgical alternatives with scrotal, abdominal, or groin full-thickness skin grafts (FTGs). By overstretching the penile skin, extra neovaginal centimeters can be achieved, but vulvoplasty with the labia minora and clitoral hood formation is more demanding or even impossible. Most patients treated with puberty-suppressing hormones have had no preoperative sexual experience. Preoperative consultation with a pelvic floor physical therapist may facilitate an easy postoperative dilation regimen. If intestinal vaginoplasty is performed as a revision procedure, an in-depth analysis of the reason for primary failure is important to prevent failure of the revision procedure. Comorbidities, intraoperative and postoperative complications, dilation regimen, and pelvic floor hypertonicity are assessed to prevent failure in revision procedures. In selected cases, preoperative endoscopic examination of the sigmoid can be performed to assess the health and mucosal integrity of the intestinal segment. Patients with inflammatory bowel disease are not eligible for intestinal vaginoplasty. Also, patients with a familial predisposition to colon cancer (Lynch syndrome) should be offered small bowel (ileum) vaginoplasty. Laser depilation of the genital region must be performed before surgery. A preoperative anesthetic assessment is performed, as is standard preoperative care for elective surgery. HIV-infected patients must have an adequate CD4 cell count and undetectable viral load to reduce the risk of postoperative complications.4 In colon vaginoplasty, full bowel preparation is used to prevent stool spillage from the transposed sigmoid segment into the perineal wound bed when the segment is opened. As is standard, intravenous antibiotics (750 mg of cefuroxime and 500 mg of metronidazole for gram-negative bacteria) are administered 30 minutes before surgery. After general anesthesia is administered, the patient is placed on a surgical vacuum mattress in an extended lithotomy-Trendelenburg position in stirrups. The right arm is positioned alongside the body, sufficiently padded to prevent iatrogenic neuropathy and pressure-related physical problems. The left arm is put on an armrest, so the intravenous catheter is easily accessible to the anesthesiologist. In this way a simultaneous abdominoperineal approach is facilitated. The bladder is catheterized. The gastrointestinal laparoscopic surgeon is positioned at the patient’s right lateral side. The plastic surgeon is positioned between the legs. Fig. 6-1 Surgical construction of the female external genitalia. A, Design of the perineoscrotal flap. B, Dissection of the neovaginal tunnel. The plastic surgeon begins by incising a caudally based perineoscrotal full-thickness triangular skin flap measuring 2 by 4 cm, continuing in a cranially directed midscrotal incision (Fig. 6-1, A). This opens the way to the perineal bottom. By dissecting the bulbospongiosus muscle off the bulbar part of the urethra, a safe entrance to the pelvic floor is created. To check rectal wall integrity, a straight clamp with gauze is placed rectally. This gauze directs the surgeon and prevents rectal injury during dissection of the perineal cavity. With sharp dissection of the midline raphe, the loose plane of Denonvilliers fascia is reached. To facilitate further dissection of the cavity, partial (diathermic) dissection of the levator ani muscle is performed (Fig. 6-1, B). This provides sufficient width for the neovaginal cavity. Next, blunt dissection above Denonvilliers fascia is carried out up to the peritoneal fold. Gauze with epinephrine is placed in the newly formed cavity, until the laparoscopic surgeon is ready to open the peritoneal fold. From the intraabdominal approach, this gauze can be visualized through the parietal peritoneum and functions as a guide for the laparoscopic surgeon to find the proper direction and plane to the neovaginal cavity. The blood supply of the corpus spongiosum is ligated, and a reduction of the corporeal body is performed and oversewn. Bilateral orchiectomy is executed after careful ligation of the vas deferens, ensuring that the stumps are freed and able to retract back into the inguinal canal (Fig. 6-2, A). The urethra is shortened and spatulated. After circumcision, leaving about 3 to 4 cm of the preputium to the corona, the penile skin is dissected off the penile body with the avascular plane superficial to Buck fascia, leaving it attached proximal to the pubic region (Fig. 6-2, B). Fig. 6-2 A, Bilateral orchiectomy. B, Penile skin dissection. C, Sculpturing of the clitoris, clitoral hood, and labia minora. D, Dissection of the neurovascular bundle. E, Measurement of the length of the sigmoid conduit by transillumination. F, Resection of redundant scrotal skin to form the labia majora. A clitoris, clitoral hood, and labia minora are sculptured from the preputium and part of the glans penis (Fig. 6-2, C). By dissecting a pedicled dorsal penile neurovascular bundle off the corporeal cavernous bodies, sensation and vascularization of the neoclitoris and labia minora are well preserved (Fig. 6-2, D). In patients who have been treated with puberty-suppressing hormones, penile hypoplasia may be so severe that the whole penile skin is needed for labial construction.5,6 In these patients, the penile skin will serve as the outer layer and the short preputial flap as the inner layer of the labia minora. The penile skin is then inverted. At the level of the future vulva, a vertical incision is made in the inversion flap to bring out the clitoris, labia minora, infundibulum, and urinary meatus. They are sutured to the inversion flap. Depending on the length and width of the penile skin, a part can be inverted into the neovaginal canal. This forms a small skin bridge between the caudal part of the neomeatus and the attachment of the intestinal vagina. Redundant scrotal skin is trimmed to form the labia majora, and the neovaginal depth is measured (Fig. 6-2, E and F). Scars are placed as inconspicuously as possible in the inguinal fold. At this point in the operation, the simultaneous laparoscopic dissection and mobilization of the sigmoid segment is completed. After open introduction of the first (umbilical) trochar, the pneumoperitoneum (12 to 14 mm Hg) is applied. After abdominal inspection for adhesions and unexpected findings, a 5 mm right lateral trochar is positioned in the midclavicular line at the height of the umbilicus. A third 12 mm trochar is then placed just lateral to the epigastric vessels in the right lower quadrant. The procedure starts with mobilization of the sigmoid segment from the peritoneal lateral adhesions (Fig. 6-3, A). The peritoneal fold is opened, and the mesosigmoid is mobilized from lateral to medial. The vascular anatomy is identified, with special attention to the sigmoid arteries and veins. A 6- to 7-inch sigmoid segment will be isolated for creation of the neovagina. The distal part must be introduced through the neovaginal tunnel for suturing at the level of the penile-inverted skin in the perineum. Vascular mobilization should allow this descent of the sigmoid. Because the anatomy of the vessels differs widely among patients, careful perioperative mapping should be done to avoid damage to the sigmoid arteries and the common branch of Drummond, because vascularization of the sigmoid segment will depend on this branch. Near-infrared fluorescence angiography can be used for intraoperative assessment of the adequacy of blood perfusion. Just above the rectum at the height of the upper margin of the promontory, the sigmoid artery is divided with a linear stapler/cutter (60 mm) (Fig. 6-3, B). The mesosigmoid is transected to the base of the sigmoid arteries (Fig. 6-3, C). In most cases the first distal or first and second distal arteries must be divided to obtain sufficient mobilization for the sigmoid segment to descend safely and tension free to the perineal anastomosis. The distal part is completely dependent on the arcade of Drummond. In some patients the arcade is incomplete at the midsigmoid level (Sudeck point). In that case transection of the first or first and second artery may lead to ischemia of the distal sigmoid. After complete mobilization of the sigmoid and mesosigmoid and transsection of the first and if needed second vascular trunk, the distal sigmoid is checked for pulsations in the mesentery and transverse arteries ascending to the bowel.
Male-to-Female Gender Affirmation Colon Vaginoplasty: Total Laparoscopic Sigmoid Vaginoplasty
Key Points
 Total laparoscopic sigmoid vaginoplasty is a feasible and safe surgical technique for vaginal construction (reconstruction), if performed by an experienced team, with the right medical infrastructure and laparoscopic equipment.
Total laparoscopic sigmoid vaginoplasty is a feasible and safe surgical technique for vaginal construction (reconstruction), if performed by an experienced team, with the right medical infrastructure and laparoscopic equipment.
 It is indicated for primary and revision vaginoplasty in transgender and biologic women.
It is indicated for primary and revision vaginoplasty in transgender and biologic women.
 The technique provides good surgical and functional outcomes.
The technique provides good surgical and functional outcomes.
Indications and Contraindications
The Team and Infrastructure
Patient Evaluation
Preoperative Planning and Preparation
Intraoperative Measures and Positioning
Surgical Technique in Primary Cases
Perineal Phase and Vulvoplasty
Dissection of the Neovaginal Tunnel
Surgical Construction of the Female External Genitalia
Laparoscopic Isolation and Transposition of the Sigmoid Segment
Mobilization of the Sigmoid Segment
Abdominal Key
Fastest Abdominal Insight Engine