CHAPTER 95 Liver Transplantation
Despite continued advances in the treatment of chronic liver disease, most notably antiviral therapy, and management of complications of chronic liver disease, such as transjugular intrahepatic portosystemic shunt (TIPS) placement, liver transplantation remains the only prospect for long-term survival in patients with advanced liver disease who have reached the limits of purely medical interventions. The major indications for liver transplantation in adults are decompensated cirrhosis, unresectable primary hepatic malignancies, and acute liver failure in which spontaneous recovery is not anticipated.1 Liver transplantation has continued to evolve in response to the shortage of deceased-donor organs and the frequency of recurrent disease. The availability of a wider array of immunosuppressive agents has made graft rejection a lesser threat than disease recurrence.2 Recurrence of hepatitis C virus (HCV) infection, because of its frequency as an indication for liver transplantation, high rate of graft reinfection and failure, and lack of effective prophylaxis, has become a major challenge in the care of liver transplant recipients.3 By contrast, modern regimens of prophylaxis to prevent hepatitis B virus (HBV) reinfection now allow liver transplantation to be undertaken with a low likelihood of recurrence.4 Recurrence of nonviral liver disease is now recognized as a threat to the graft, albeit of an order of magnitude less frequent than that for HCV reinfection.5 Because immunosuppression has a proviral effect, a number of liver transplantation centers have attempted earlier reduction or withdrawal of glucocorticoids in recipients with chronic HBV or HCV infection.6 By contrast, more intensive immunosuppression may be necessary in liver transplant recipients with autoimmune liver diseases.7
The apparently intractable shortage of deceased donors is reflected in continuing deaths of potential recipients listed for liver transplantation. A major change in the allocation of available organs has occurred with the introduction of the Model for End-stage Liver Disease (MELD) score, which has achieved its stated aim of reducing the number of deaths on the liver transplantation waiting list.8 This method of organ allocation assigns organs to recipients on the basis of an objective, continuous measure of severity of liver disease, thereby removing time spent on the waiting list as a determining factor. Extension of live-donor liver transplantation (LDLT) to adult recipients has increased the organ pool despite the tempering of enthusiasm following an increased appreciation of potential risks to the donor.9 Other innovations such as splitting deceased-donor grafts to benefit two recipients and use of so-called marginal or extended criteria grafts, including those from older and non–heart-beating donors, also have expanded the organ supply modestly.10 An increased frequency of complications, most notably of the biliary tract, has been a consequence of expanding the donor criteria, however.11 Efforts to expand the deceased-donor supply by public education programs have succeeded in enhancing organ donation, although the major discrepancy between the number of potential recipients and the number of available organs persists, resulting in continuing attrition of listed patients who succumb to complications of decompensated liver disease while awaiting liver transplantation.12
Although the organ allocation system will undoubtedly continue to evolve and recurrence of disease will remain a threat, the prospects for long-term survival are very good to excellent for most liver transplant recipients who otherwise would succumb to their liver disease. For instance, the likely one-year survival rate for patients with decompensated cirrhosis is less than 10% without liver transplantation but approximately 85% to 90% at one year and 75% at five years after transplantation for most indications.13
Access to liver transplantation has transformed the management of advanced liver disease but has resulted in an expanding cohort of decompensated potential recipients who require frequent medical attention.14 Because the best outcomes following liver transplantation are obtained in patients who have not already experienced multiple complications of liver disease,15 referral for transplantation evaluation is appropriate when a cirrhotic patient has had an index complication, such as the onset of ascites. For at least some potential recipients, access to LDLT may avoid a lengthy waiting period with the risk of further and potentially life-threatening complications of liver disease.
In parallel with the evolution of liver transplantation, the care of transplantation candidates with advanced disease has become a major clinical challenge. The transplantation hepatologist must combine the skills necessary to practice gastroenterology, multidisciplinary internal medicine, and intensive care. This skill set has been formally recognized by the development of a secondary subspecialty in transplantation hepatology by the American Board of Internal Medicine.16
INDICATIONS
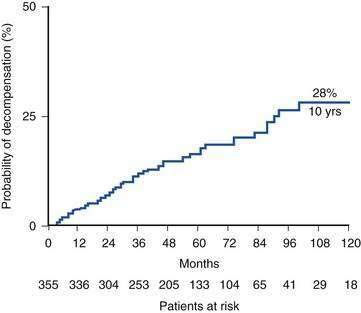
The major indications for liver transplantation in adults reflect the most frequent causes of adult liver disease, notably chronic hepatitis C, alcoholic liver disease, and, to a lesser extent, chronic hepatitis B, primary biliary cirrhosis (PBC), primary sclerosing cholangitis (PSC), autoimmune hepatitis, and hemochromatosis (Fig. 95-1). Many liver transplantation candidates previously diagnosed as having “cryptogenic” cirrhosis are now considered to have underlying nonalcoholic fatty liver disease (NAFLD). An uncommon but important indication for liver transplantation is acute liver failure, which has a high mortality rate in the absence of liver transplantation. The role of liver transplantation in primary hepatic malignancy has become better defined; a subset of patients with primary hepatocellular carcinoma (HCC) have a high likelihood of cure with transplantation, although the roles of adjunctive therapies such as transarterial chemoembolization (TACE), radiofrequency ablation, and the oral chemotherapy agent sorafenib need to be defined (see Chapter 94).17 The other major primary adult hepatic malignancy, cholangiocarcinoma, had been regarded as a contraindication to liver transplantation because of its rapid and almost invariable recurrence post–liver transplantation, although acceptable outcomes have been reported in a subset of patients with hilar tumors who receive adjuvant external beam radiation and chemosensitization (see Chapter 69).18 The major indication for pediatric liver transplantation is biliary atresia following a failed Kasai procedure (portoenterostomy) or delayed recognition of the diagnosis (see Chapter 62). Other major pediatric indications include α1-antitrypsin deficiency and other metabolic disorders (see Chapter 76).
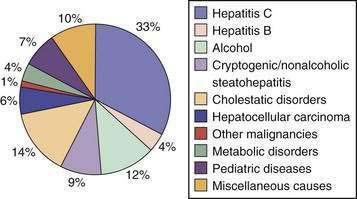
Figure 95-1. Proportion of liver transplants performed for specific indications, 1992 to 2007.
(From O’Leary JG, Lepe R, Davis GL. Indications for liver transplantation. Gastroenterology 2008; 134:1764-76, with permission.)
Recognition of cirrhosis per se is not an indication for liver transplantation, although a key issue in managing a cirrhotic patient is deciding whether transplantation will be needed in the future and when referral for evaluation is appropriate (Table 95-1). Another important aspect of the management of a compensated cirrhotic patient is the anticipation of complications. Endoscopic surveillance of patients with cirrhosis for gastroesophageal varices, for instance, to offer prophylaxis, either pharmacologic or endoscopic, to prevent initial or recurrent gastrointestinal bleeding is now routine practice (see Chapter 90).14 Surveillance for HCC is also regarded as the standard of care in a cirrhotic patient (see Chapter 94). Discovery of a hepatic mass suggestive of HCC in a cirrhotic patient should prompt evaluation to determine whether hepatic resection or liver transplantation is the most appropriate curative approach. Otherwise, liver transplantation should normally be a consideration only when the limits of medical therapy for complications of cirrhosis have been reached, particularly if LDLT is an option. The risk of surgery must always be weighed against a realistic assessment of the potential recipient’s prognosis in the absence of liver transplantation. For example, in a patient with decompensated cirrhosis caused by HBV infection, effective suppression of viral replication by an effective antiviral agent may result in impressive clinical improvement, thereby delaying or even obviating the need for liver transplantation (see Chapter 78). Similarly, abstinence from alcohol can result in resolution of signs of hepatic decompensation in a patient with alcoholic liver disease (see Chapter 84). The course of chronic liver disease remains unpredictable, however, and observing an apparently well-compensated patient deteriorate dramatically because of an intercurrent complication such as variceal bleeding is sobering. Although recognition of cirrhosis implies a risk of major complications and diminished life expectancy, a cirrhotic patient can remain stable for a protracted period of time. For example, Fattovich and colleagues19 observed that in patients with well-compensated cirrhosis caused by HCV infection, major complications of portal hypertension such as ascites and variceal hemorrhage occurred in less than 30% at 10 years; in the absence of an index complication, survival was excellent (Fig. 95-2). Once a complication supervenes, however, survival diminishes rapidly. For example, after the development of ascites refractory to diuretics, only 25% of patients survive beyond 1 year.20 A prospective study of more than 200 Italian patients with HCV-related compensated cirrhosis followed for up to 17 years found that HCC was the most common complication of cirrhosis detected, occurring in 32%, followed by ascites. These findings imply that HCC, rather than complications of portal hypertension, is the most frequent reason for a worsening prognosis in a patient with cirrhosis.21
Table 95-1 Indications for Liver Transplantation
The development of predictive models based on the natural history of PBC (see Chapter 89) and PSC (see Chapter 68)22 has helped clinical decision making for patients with these cholestatic disorders, which tend to progress in a fairly stereotypical fashion. Before the introduction of the MELD score, analogous models had not been available for the noncholestatic forms of cirrhosis, and the decision to refer a patient for liver transplantation generally was based on an estimate of disease severity using objective parameters such as the serum albumin level as well as more subjective factors such as the presence of hepatic encephalopathy, as in the Child-Turcotte-Pugh score (see Chapter 90).
On clinical rather than biochemical grounds, important indications for liver transplantation remain disease severity reflective of hepatocellular failure, reflected by coagulopathy and jaundice; complications of portal hypertension, such as refractory ascites and recurrent variceal bleeding; or the combination of portosystemic shunting and diminished hepatocellular function, as in hepatic encephalopathy (see Table 95-1). Following validation of predictive models for the natural history of PBC and PSC, prediction of an individual patient’s course has been possible on the basis of simple clinical and laboratory parameters, the most ominous of which is a rising serum bilirubin level. Although deterioration in a patient’s quality of life typically may not be reflected adequately in predictive models, including MELD, the presence of potentially disabling symptoms such as pruritus and osteopenia in patients with cholestatic and other forms of cirrhosis, as well as recurrent bacterial cholangitis in those with PSC, are important considerations in deciding when to refer a patient for liver transplantation. MELD exceptions, such as adding points to the so-called biological MELD score in order to increase the likelihood of liver transplantation, require approval by a local regional review board, which includes representatives from local transplantation programs. The awarding of extra MELD points recognizes that although this system is a major advance in organ allocation, at least some patients may be disadvantaged by its use of purely objective parameters and exclusion of factors such as intractable ascites or encephalopathy that were incorporated into older allocation schemes. Ideally, liver transplantation should occur before a protracted period of disability reduces the likelihood that post-transplantation rehabilitation will lead to full employment and normal social functioning.
LISTING CRITERIA AND POLICIES OF THE UNITED NETWORK FOR ORGAN SHARING
Organ allocation within the United States is administered by the United Network for Organ Sharing (UNOS), which now considers only disease severity (and not waiting time, as in the past) to determine a patient’s priority for liver transplantation. A variety of organ allocation systems have been used since the 1980s to allocate the limited number of deceased-donor organs in an equitable manner. Older systems were based on a combination of clinical and biochemical parameters such as the Child-Turcotte-Pugh score. The MELD score is a mathematical formula (available at www.unos.org) that incorporates the serum bilirubin level, creatinine level, and international normalized ratio (INR) and provides a more objective and accurate way to stratify liver transplantation candidates for organ allocation and to eliminate time waiting for a donor organ as a determining factor.23 The MELD score overcomes some of the inherent limitations of the Child-Turcotte-Pugh score, including limited discriminatory ability, subjective interpretation of parameters such as presence or absence of ascites on the basis of the physical examination, and the “ceiling effect” of the Child-Turcotte-Pugh score (e.g., no greater weight is given to a serum bilirubin level of 35 mg/dL than to a level of 3.5 mg/dL, even though a patient with the markedly higher bilirubin level clearly has more advanced liver disease). Inclusion of the serum creatinine level reflects the major prognostic importance of renal dysfunction in patients with advanced liver disease. Adoption of the MELD score has been a major step in achieving an equitable organ allocation system in the United States, although it will undoubtedly continue to undergo refinement.
ABSOLUTE AND RELATIVE CONTRAINDICATIONS
Contraindications to liver transplantation have also evolved, reflecting innovations in surgical technique and postoperative care. As an example of the latter, effective prophylaxis against HBV recurrence now allows excellent graft and patient survival rates in patients with chronic hepatitis B.24 On the other hand, greater experience has highlighted the futility of retransplantation in many debilitated recipients with a failing graft caused by recurrent HCV infection.25 By contrast, the introduction of highly effective antiretroviral therapy has allowed consideration of liver transplantation in human immunodeficiency virus (HIV)–infected patients with decompensated liver disease, typically caused by either HCV or HBV infection.26 Still, absolute and relative contraindications remain. An absolute contraindication (Table 95-2) to liver transplantation is a clinical circumstance in which the likelihood of a successful outcome is so remote that liver transplantation should not be offered. A relative contraindication implies a suboptimal likelihood of a good outcome, although liver transplantation may still be considered in some patients.
Table 95-2 Absolute Contraindications to Liver Transplantation
* ICP, intracranial pressure; CPP, cerebral perfusion pressure; CPP, equals the mean arterial pressure minus ICP.
The role of liver transplantation in the management of HCC has become better defined with the recognition that a large tumor burden is associated with a high probability of metastatic spread within a short time of liver transplantation.27 Some tumor characteristics predictive of a poor outcome, most notably vascular invasion, may only be apparent once the explant is examined, despite the sophistication of current imaging techniques. Although results of liver transplantation for cholangiocarcinoma have been poor because of a high rate of tumor recurrence, a subset of patients with hilar tumors may benefit from multimodal therapy and liver transplantation. The results of liver transplantation remain poor for angiosarcoma, and its recognition pre–liver transplantation remains an absolute contraindication. By contrast, at least some patients with epithelioid hemangioendothelioma have been transplanted successfully, despite an extensive tumor burden, with documented regression of extrahepatic metastases.
For a transplantation candidate with a prior extrahepatic malignancy, therapy needs to have been curative, with the resection specimen indicating a low likelihood of metastatic spread. A two-year recurrence-free interval is adequate for most nonhepatic malignancies prior to liver transplantation, but for breast cancer, colon cancer, and malignant melanoma, a longer period following resection is desirable.28 Myeloproliferative disorders frequently underlie Budd-Chiari syndrome (see Chapter 83), but fortunately their evolution to acute leukemia is not accelerated following liver transplantation.29
Ongoing alcohol or recreational drug use remains an absolute contraindication to liver transplantation. If continued abuse is a concern, random toxicology screens are appropriate. Although medicinal marijuana may be used legitimately for palliation, most transplantation programs discourage the use of marijuana because of concerns about the overall compliance of users and possible pulmonary side effects, as well as some evidence that its use may adversely affect the course of liver disease (a point that may be moot in a patient already listed for liver transplantation). A history of prescription narcotic abuse is also a cause for concern because it may contribute to difficulties with pain management post–liver transplantation. Non-narcotic alternatives should be attempted for the management of chronic pain. Other analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs) also are contraindicated in persons with end-stage liver disease because of potential renal and gastrointestinal complications. Cigarette smoking is prohibited in liver transplantation candidates as well because of its multiple adverse effects, including an associated risk of hepatic artery thrombosis and malignancy post–liver transplantation.30 With the increasing use of herbal compounds and other so-called health products, a discussion of their unproven efficacy and unknown toxicities and caution against their use in the post–liver transplantation setting because of the potential for drug interactions are appropriate (see Chapter 87).31
The careful medical evaluation necessary prior to liver transplantation frequently uncovers important comorbidities, typically cardiac and pulmonary. Although patients with decompensated cirrhosis were previously thought to be somewhat protected against coronary artery disease (CAD) because of low afterload, reflecting peripheral vasodilatation, decreased hepatic synthesis of cholesterol, and increased circulating estrogen levels, cirrhotic patients have a prevalence of CAD at least as great as that of an age-matched control population.32 Risk factors for CAD in cirrhotic patients include a high prevalence of diabetes mellitus. Additional risk factors in the post–liver transplantation period include immunosuppressive drugs that contribute to systemic hypertension, hyperlipidemia, and obesity. Assessment of cardiac risk in cirrhotic patients may be inadequate because of poor physical stamina during routine stress testing. Administration of dobutamine mimics the physiologic effects of exercise and is used with stress echocardiography to exclude clinically significant CAD in liver transplant recipients with cirrhosis. Patients who reach 85% of the maximal predicted heart rate without an abnormality on stress echocardiogram have a low likelihood of peri- and postoperative ischemic cardiac events.33 Discrete coronary artery stenoses can be managed by angioplasty and stenting pre–liver transplantation. Although surgical bypass grafting may be contraindicated because of a significant perioperative risk of excessive bleeding in a patient with decompensated cirrhosis, such surgery, if successful, may render a patient an acceptable candidate for liver transplantation. Pre–liver transplantation cardiac evaluation may overestimate cardiac performance. impaired cardiac function may become apparent only after the protective effect of the decreased systemic vascular resistance that characterizes cirrhosis is lost after liver transplantation, when afterload increases because of the hypertensive effects of the primary immunosuppressive agents and when overvigorous volume repletion may occur.34 Specific forms of cirrhosis may be associated with extrahepatic manifestations that diminish long-term survival. For example, lethal cardiac arrythmias may result in poorer survival in patients who undergo liver transplantation for decompensated cirrhosis caused by hemochromatosis.35
Pulmonary evaluation in the liver transplantation candidate may reveal abnormal arterial oxygenation (see Chapter 92). Although severe chronic obstructive pulmonary disease or pulmonary fibrosis precludes liver transplantation, respiratory restriction as a result of ascites or diminished respiratory muscle strength caused by chronic illness is reversible and does not preclude liver transplantation. Even patients who undergo liver transplantation for α1-antitrypsin deficiency may show improvement in pulmonary function tests postoperatively.36 The hepatopulmonary syndrome (HPS) is characterized by the triad of chronic liver disease, pulmonary vascular dilatations (with right-to-left shunting), and hypoxemia.37 The diagnosis is suggested by the finding of a Pao2 value of less than 70 mm Hg on an arterial blood gas determination obtained from the patient in the supine position. Definitive diagnosis is made by the demonstration of intrapulmonary vascular dilatations by contrast-enhanced echocardiography (which is the most sensitive technique), perfusion lung scanning with 99mTc–labeled macroaggregated albumin, or pulmonary arteriography. Detection of contrast in the left side of the heart within several beats after its appearance in the right atrium indicates intrapulmonary shunting. Predictors of potential reversibility of HPS after liver transplantation include younger age, a lesser degree of preoperative hypoxemia, and adequate correction of hypoxemia with inspiration of 100% oxygen (Pao2 >200 mm Hg).38 In the majority of patients with HPS, hypoxemia resolves within several months of liver transplantation, although a protracted period of ventilatory support in the immediate postoperative period may be required. Because of the potential for improvement with liver transplantation, extra MELD points may be allocated to a patient with HPS. HPS must be distinguished from portopulmonary hypertension, because the latter is associated with high perioperative mortality and frequently unchanged pulmonary hemodynamics despite liver transplantation. Specifically, documentation of a mean pulmonary arterial pressure greater than 35 mm Hg, pulmonary vascular resistance greater than 300 dynes • s • cm−5, and cardiac output less than 8 L/minute are indicative of a high perioperative risk because the patient will be unable to increase the cardiac output appropriately in response to altered intra- and postoperative hemodynamics. Vasodilator therapy may reduce pulmonary arterial pressure and permit liver transplantation.39
Hepatic hydrothorax is a frequent manifestation of portal hypertension characterized by collection of a transudate in the pleural cavity, usually on the right side and often with relatively little ascites remaining in the abdominal cavity (see Chapter 91). Hepatic hydrothorax can be particularly difficult to manage and often requires repeated thoracentesis or placement of a TIPS pre–liver transplantation.40 The temptation to insert a permanent chest tube needs to be resisted because a chest tube can lead to infection in the pleural cavity with the risk of fistula formation. Similarly, interventions such as pleurodesis or pleural decortication should be avoided because hepatic hydrothorax can be controlled only by a reduction in portal pressure.
Active uncontrolled extrahepatic infection is an absolute contraindication to liver transplantation, which should be deferred if sepsis is suspected. In a patient with decompensated cirrhosis, an unexplained clinical deterioration such as altered mental status or systemic hypotension in the absence of gastrointestinal hemorrhage must be presumed to reflect sepsis and is an indication to start broad antibiotic coverage while culture results are awaited. Liver transplantation, however, may be the only option for a patient with recurrent bacterial cholangitis in the setting of PSC (see Chapter 68). Repeated bouts of spontaneous bacterial peritonitis need to be controlled by antibiotic therapy prior to attempting liver transplantation (see Chapter 91). A particularly ominous finding is fungemia, which is typically impossible to eradicate in a debilitated cirrhotic patient and precludes liver transplantation.
An important technical consideration in the liver transplantation candidate is the presence of vascular abnormalities that may increase the difficulty of surgery. With increased surgical experience, however, such abnormalities, most notably portal vein thrombosis, are less likely to be obstacles to liver transplantation. More extensive vascular thrombosis with involvement of the superior mesenteric vein may require extensive vascular reconstruction.41 The presence of a prior portosystemic shunt, particularly a nonselective (side-to-side or end-to-side) portocaval shunt, increases the technical complexity of liver transplantation but is no longer regarded as a contraindication. With the widespread use of TIPS to control manifestations of portal hypertension, including variceal hemorrhage, intractable ascites, and hydrothorax, without disrupting the vascular anatomy, TIPS is now the most frequent shunt encountered in liver transplant recipients and does not usually present an additional operative challenge during liver transplantation.
Age restrictions have been relaxed in liver transplantation candidates, although close attention must be paid to comorbid conditions in older patients that not only increase the risk of perioperative mortality, but also may decrease the likelihood that the liver transplant recipient will be able to return to an active lifestyle, particularly because severe liver disease may cause more debility in older than in younger patients.42 Because a subset of robust older recipients have good outcomes after liver transplantation, candidates in their late 60s or even older who are otherwise in good health should not be precluded a priori from liver transplantation.
The differential diagnosis of renal insufficiency in patients with advanced liver disease includes hepatorenal syndrome, which is potentially reversible. Renal failure remains an important predictor of a poor outcome post–liver transplantation (see Chapter 92).43 Typically, renal dysfunction in patients with decompensated cirrhosis reflects a variety of insults, including sepsis, hypotension, and use of nephrotoxic medications. In liver transplant recipients with decompensated cirrhosis, renal insufficiency severe enough to require dialysis has been associated consistently with poorer patient outcomes. Assessment of the potential for improvement following liver transplantation is critical. A rule of thumb is that return of adequate renal function is unlikely after liver transplantation if dialysis has been required for more than one month prior to liver transplantation. Inclusion of the serum creatinine level in the MELD score reflects the major prognostic importance of renal insufficiency in patients with advanced liver disease. A consequence of this recognition has been an increased rate of combined liver-kidney transplantation in the MELD era of liver transplantation, with a consequent depletion in the supply of kidneys for patients awaiting isolated deceased-donor renal transplantation.44 An important reflection of impaired free-water handling in patients with decompensated cirrhosis is dilutional hyponatremia. Consequences of hyponatremia include altered mental status with more profound degrees of hyponatremia and an increased risk of calcineurin-induced neurotoxicity after liver transplantation (see later). Incorporation of the serum sodium level into the MELD formula (MELDNa) may increase the prognostic accuracy of the MELD score, particularly in patients with relatively low MELD scores.45
A major systemic manifestation of decompensated cirrhosis is malnutrition. Loss of muscle mass increases the likelihood of perioperative morbidity, with a need for more protracted ventilator support and poorer patient survival. Peripheral edema and ascites make changes in body weight or anthropometric measurements unreliable for assessing nutritional status in a patient with advanced cirrhosis. More profound nutritional deficiencies may reflect the specific cause of cirrhosis, as in a malnourished alcoholic person with multiple vitamin and electrolyte deficiencies or a patient with cholestatic liver disease and depletion of fat-soluble vitamins as a result of small intestinal malabsorption. Evaluation by a dietitian is an integral part of the assessment of the liver transplantation candidate. Attempts to improve the nutritional status of liver transplantation candidates have included enteral and parenteral feeding, which may result in improvement, albeit modest, in some patients.46 An increasingly obese liver transplantation candidate pool is raising concerns about the role of obesity in the pathogenesis of NAFLD and in postoperative mortality resulting from cardiovascular events, as well as postoperative complications such as wound infections.47
TRANSPLANTATION EVALUATION AND LISTING
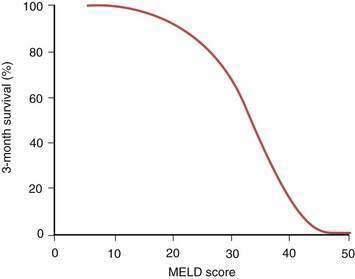
The details of the formal liver transplantation evaluation vary from center to center, but the essentials are to establish that liver transplantation is indicated in the management of the potential recipient’s liver disease, the patient has no comorbidities severe enough to preclude transplantation, and the patient has adequate emotional and social resources to undergo a major surgical procedure and continue on long-term immunosuppression afterward (Table 95-3). Generally in the United States, clearance is needed from the patient’s insurance carrier before the extensive testing necessary for liver transplantation evaluation is undertaken. The patient is seen by a transplantation surgeon, hepatologist, psychiatrist, dietitian, and social worker, with additional consultations as clinically indicated. As increasingly frailer and older candidates are evaluated, identifying potential causes of perioperative morbidity, such as carotid artery stenosis, is imperative. Detailed abdominal imaging is performed not only to screen for HCC, but also to uncover vascular abnormalities such as portal vein thrombosis that may make surgery technically challenging. Disease-specific issues need to be addressed, such as the likelihood of recidivism in the alcoholic patient or management of a large tumor burden in the patient with HCC. The appropriateness of liver transplantation for each candidate is then discussed formally at a meeting of the patient selection committee with input from the members of the transplantation team. If the patient’s candidacy is deemed to be appropriate, formal listing is undertaken with UNOS by matching of the recipient by blood type and weight with potential deceased donors. Once listed, the patient’s priority for organ allocation is determined by the MELD score, based either on the pure score consisting of the serum bilirubin level, serum creatinine level, and INR or that score plus additional points awarded for specific indications, such as HCC. Waiting time on the list is no longer a determining factor. With the critical and seemingly intractable shortage of deceased-donor organs, a major challenge for UNOS and organ retrieval agencies elsewhere in the world has been to develop an equitable system of allocation in an effort to ensure that hepatic allografts are not used for patients whose prognosis without liver transplantation remains good. Patients with a MELD score of less than 15 appear have a better survival without transplantation than with transplantation. As shown in Figure 95-3, the MELD score has been shown to correlate with the three-month survival rate. Patients with a MELD score of less than 10 are ineligible for active listing with UNOS unless they are eligible to receive extra points because of an additional complication of liver disease, such as HCC or HPS.
Table 95-3 Transplantation Evaluation Process
| Financial screening | Secure approval for evaluation |
| Medical evaluation | As discussed in text |
| Hepatology evaluation | Confirm diagnosis and optimize management |
| Laboratory testing | Assess hepatic synthetic function, serum electrolytes, renal function, viral serologies, markers of other causes of liver disease, tumor markers, ABO-Rh blood typing; 24-hour urine for creatinine clearance; urinalysis and urine drug screen |
| Cardiac evaluation | Electrocardiography and two-dimensional echocardiography, stress testing and cardiology consult if risk factors are present and/or patient is age 40 years or older |
| Hepatic imaging | Ultrasonography with Doppler to document portal vein patency, triple-phase computed tomography or gadolinium magnetic resonance imaging for tumor screening |
| General health assessment | Chest film, prostate specific antigen level (men), Pap smear and mammogram (women), colonoscopy if patient is age 50 years or older or has primary sclerosing cholangitis |
| Transplantation surgery evaluation | Assess technical issues and discuss risks of procedure |
| Anesthesia evaluation | Required if unusually high operative risk, e.g., patient has portopulmonary hypertension, hypertrophic obstructive cardiomyopathy, previous anesthesia complications |
| Psychiatry or psychology consultation | If history of substance abuse, psychiatric illness, or adjustment difficulties |
| Social work evaluation | Address potential psychosocial issues and possible effect of transplantation on patient’s personal and social system |
| Financial and insurance counseling | Itemize costs of transplantation and post-transplantation care; help develop financial management plans |
| Nutritional evaluation | Assess nutritional status and patient education |
From O’Leary JG, Lepe R, Davis GL. Indications for liver transplantation. Gastroenterology 2008; 134:1764-76, with permission.
DISEASE-SPECIFIC INDICATIONS
ALCOHOLIC LIVER DISEASE
Despite the high frequency of chronic HCV infection as an indication for liver transplantation (see later), alcoholic liver disease (ALD) remains the most frequent cause of decompensated chronic liver disease (see Chapter 84). Decompensated alcoholic cirrhosis is now firmly established as a legitimate indication for liver transplantation despite some lingering controversy.48 Concerns in the past included the risk of recidivism following liver transplantation as well as potentially poor compliance by transplant recipients with a history of alcoholism. In addition, the large number of patients with ALD was thought to have the potential to outstrip the donor supply. These fears have not been confirmed, and even patients with evidence of acute alcoholic hepatitis in the explant do not appear to have inferior post–liver transplantation survival rates despite some earlier reports to the contrary. Excellent graft and patient survival rates are the norm following liver transplantation for ALD.
Key factors in determining an alcoholic patient’s suitability for liver transplantation include recognition by the patient of the key role alcohol has played in the genesis of the liver disease, participation in some form of alcohol rehabilitation, such as attendance at Alcoholics Anonymous, stable social support, and a defined period of abstinence from alcohol before transplantation. Conventionally this period of abstinence has been six months, although rigorous studies have failed to confirm that this duration of abstinence per se confers a high likelihood of continued sobriety but have emphasized the importance of factors such as a lack of either isolation or depression. Despite these strategies, however, a substantial proportion of alcoholic recipients resume drinking after liver transplantation, although surprisingly, graft loss or early death attributable to alcohol abuse has been uncommon. A higher rate of return to alcohol use is elicited by use of anonymous questionnaires or toxicology screening than by direct questioning of patients. With longer-term follow-up, as many as 40% of alcoholic recipients resume alcohol use.49 A particularly difficult dilemma arises in the alcoholic patient with severely decompensated liver disease and alcohol use until the time of hepatic decompensation in whom the likelihood of surviving without prompt liver transplantation is low. Clearly enunciated criteria, including a contractual commitment by the patient to sobriety and active involvement in some form of alcohol rehabilitation such as participation in Alcoholics Anonymous, ensure that the selection process is equitable under these circumstances. Patients who return to pathologic drinking after liver transplantation appear to have a higher rate of medical problems, including pneumonia, cellulitis, and pancreatitis, that require hospital admission and occasionally lead to graft loss and death. In addition, alcoholic liver transplant recipients are prone to develop de novo oropharyngeal and lung tumors, likely reflecting other aspects of an alcoholic lifestyle, most notably cigarette smoking.48
HEPATITIS B
Effective prevention of graft reinfection in the HBV-infected candidate has been a major triumph of liver transplantation. HBV recurrence was frequent and resulted in reduced patient and graft survival rates during the 1980s; as a result, Medicare refused to fund liver transplantation in HBV-infected persons. Key factors in improving outcomes included recognition of the key role of pre–liver transplantation active viral replication, as demonstrated by detection in serum of hepatitis B e antigen or HBV deoxyribonucleic acid (DNA) by molecular hybridization techniques as a predictor of recurrent HBV infection in the graft and the protective effect of long-term use of high-dose hepatitis B immunoglobulin (HBIG). In a seminal study50 Samuel and colleagues observed that patients with a fulminant presentation of acute HBV infection or hepatitis D virus coinfection had a reduced risk of recurrent hepatitis B post–liver transplantation in the absence of immunoprophylaxis, reflecting the lower level of HBV replication in patients with fulminant hepatitis B than in those with chronic hepatitis B. Long-term administration of high-dose HBIG, initially administered intravenously, resulted in markedly reduced rates of recurrence of hepatitis B post-transplantation; HBIG administered in combination initially with the nucleoside analog lamivudine further decreased the rate of HBV recurrence. Lamivudine had been used as monotherapy to prevent recurrent HBV infection post-transplantation but was limited by frequent mutations in HBV polymerase gene, leading in turn to graft reinfection.51 The optimal dosing regimen for HBIG has been difficult to establish in the absence of controlled clinical data. Some groups have titrated HBIG doses according to trough serum levels of antibody to hepatitis B surface antigen (anti-HBs). Subsequently, intramuscular administration of HBIG has been confirmed as an efficacious, and less expensive, alternative to intravenous regimens, when used in combination with lamivudine.52 HBV infection that recurs despite administration of HBIG may reflect inadequate doses of HBIG or a genomic mutation in the “a” moiety of HBsAg that results in less avid binding of the virus to HBIG.53 Lamivudine resistance, acquired before liver transplantation, has also been implicated in HBV recurrence despite apparently adequate immunoprophylaxis after liver transplantation. The availability of additional oral antiviral agents with efficacy against HBV has expanded options for preventing graft reinfection (see Chapter 78). A large, multicenter study, for example, has demonstrated that adefovir dipivoxil taken for 48 weeks results in significant virologic, biochemical, and clinical improvement in patients with chronic HBV infection both pre– and post–liver transplantation and may obviate the need of liver transplantation because of improved hepatocellular function.54 Despite the complexities of managing HBV infection in the liver transplantation patient, excellent graft and patient survival rates are now routine, in contrast to the gloomy picture for HBV-infected liver transplantation candidates prior to the use of HBIG. The ever-expanding list of oral antiviral agents promises to improve outcomes further, even in patients in whom antiviral resistance develops. With the licensing of several effective oral agents to treat HBV, HBIG use will likely be superseded by the use of combinations of oral antiviral agents. The liver transplantation candidate with chronic HBV infection is now readily accepted for liver transplantation, albeit with the requirement for long-term antiviral immunoprophylaxis.
HEPATITIS C
A particular challenge is to identify liver transplant recipients with recurrent HCV infection at increased risk of rapidly progressive graft injury. Less than 10% of patients with mild recurrent hepatitis C at one year post–liver transplantation appear to progress to allograft cirrhosis by five years. By contrast, two thirds of patients with at least moderately severe hepatitis C at one year post-transplantation progress to cirrhosis by 5 years.55 Concern has been raised, however, that with prolonged follow-up, some patients with initially mild recurrent hepatitis C after liver transplantation may experience a more aggressive course. A study by Berenguer and colleagues56
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree