LigaSure™
Giovanni Milito
Federica Cadeddu
Hemorrhoidectomy is the most effective and definitive treatment for grade 3 or 4 hemorrhoids. A variety of instruments, including the LigaSure vessel sealing system™, have been used in an attempt to reduce postoperative pain and blood loss and to allow fast wound healing and a quick return to work.
Prior to selecting LigaSure™ hemorrhoidectomy, the following factors have to be considered:
Grade of Hemorrhoids
Traditional excisional hemorrhoidectomy is indicated for third or fourth degree hemorrhoids. In a recent study of the Association of Coloproctology of Great Britain and Ireland (ACPGBI) and the Association of Surgeons of Great Britain and Ireland (ASGBI), among 889 surgeons interviewed by a questionnaire on hemorrhoidectomy techniques and indications, the commonest indication was persistent grade III and grade IV hemorrhoids after failure of conservative management. There was no consensus regarding emergency hemorrhoidectomy for thrombosed or strangulated hemorrhoids—undertaken routinely by 20% of ACPGBI and 18% of ASGBI respondents. The majority (59% ACPGBI and 46% ASGBI) of the respondents occasionally performed emergency hemorrhoidectomy (1).
Type of Patient
In rare cases of large hemorrhoids in young patients, especially in female patients after pregnancy, the hemorrhoids may recur. For this reason, hemorrhoidectomy should not be performed on pregnant women and should be postponed until the age of 30–35 years.
Preexisting Medical Conditions
Inflammatory bowel diseases such as Crohn’s disease and immune deficiency due to AIDS are both contraindications to this procedure. Moreover, cancer is also a contraindication to this procedure, as live cancer cells can be implanted in open wounds.
Prior to hospital admission, the patient should be advised to take the appropriate steps to ensure healthy bowel habits and the passage of soft stool. Usually, a phosphate enema is performed 12 hours before surgery and 500 mg of metronidazole is given intravenously at the beginning of surgery. In the ACPGBI/ASGBI trial (1), preoperative bowel preparation was often used, with enema being used in 61% of ACPGBI group cases and 43% of ASGBI group and suppository being used in 13% ACPGBI group cases and 16% of ASGBI group. A significant number of surgeons prefer no bowel preparation (19% ACPGBI and 21% ASGBI).
According to the operative protocol of most centers, patients are operated under general anesthesia as a day-case procedure or short-term surgery.
Day-case hemorrhoidectomy (DCH) has become increasingly popular, possibly stimulated by bed reductions and spending constraints. In the ACPGBI/ASGBI trial, significantly more ACPGBI (20%) than ASGBI (48, 7%; P < 0.01) members performed DCH in 50% or more cases (1).
Vessel Sealing Technology
The term “radiosurgery” has been used to indicate utilization of high frequencies, allowing a considerable improvement of several surgical techniques, including proctologic ones.
The LigaSure vessel sealing system ™ is a bipolar electrothermal device that seals blood vessels through an optimized combination of pressure and radiofrequency.
After providing pressure on the tissues by the LigaSure™ forceps application, the Force Triad energy platform™ generates energy tailored to the tissue impedance, reducing fusion cycle time and tissue desiccation with consistently controlled tissue effect. The completion of coagulation is signalled by the feedback sensors and the tissue can be excised along the line of coagulum.
LigaSure™ is different from conventional bipolar systems by using low voltage and high current and works at lower temperatures (50–80°C) than the electric scalpel (600°C).
LigaSure™ preserves the patient’s own collagen and uses it to form a permanent autologous seal that is strong enough to withstand up to three times the normal systolic (normal systolic: 120 mm/hg) on vessels or tissue bundles. This result makes LigaSure™ comparable to the mechanical methods of vessel occlusion; it ensures complete coagulation of arteries and veins up to 7 mm in diameter with minimal surrounding thermal spread up to 2 mm in diameter and limited tissue charring. Thus, a decrease in thermal injury at the surgical site may reduce anal spasm and pain. In addition, healing time is considerably shorter than that in the traditional techniques (14.8 days with LigaSure™ vs. 25.6 days with conventional diathermy in our experience (2)) and tissue damage is limited to the dissection line. The risk of cicatrization-linked stricture may also be reduced.
The area of thermal spread after monopolar electrocoagulation depends on many factors: time of application, power of electrocoagulation, and number of applications. Thermal injury after monopolar electrocoagulation, LigaSure™, bipolar electrocoagulation, and ultracision has been evaluated in many experimental studies (3). Monopolar electrocoagulation results in poorer hemostasis and more side-thermal injury of the adjacent tissue.
Operative Position
Open hemorrhoidectomy can be performed either in the lithotomy or prone position. In the lithotomy position, the buttocks are raised by a firm pad to project over the
edge of the table. In the prone position, the patient lies face down, hips on a 6-inch gel ridge, with the buttocks projecting upward. Although the prone position may help reduce venous circulation from the anorectal area, extra care should be taken to prevent restriction of breathing and ensure proper lung inflation during surgery. In both the positions, the buttocks are strapped back with an adhesive tape to facilitate access, especially for obese patients. Most surgeons perform LigaSure™ hemorrhoidectomy using an Eisenhammer retractor with the patient in the lithotomy position (Fig. 2.1).
edge of the table. In the prone position, the patient lies face down, hips on a 6-inch gel ridge, with the buttocks projecting upward. Although the prone position may help reduce venous circulation from the anorectal area, extra care should be taken to prevent restriction of breathing and ensure proper lung inflation during surgery. In both the positions, the buttocks are strapped back with an adhesive tape to facilitate access, especially for obese patients. Most surgeons perform LigaSure™ hemorrhoidectomy using an Eisenhammer retractor with the patient in the lithotomy position (Fig. 2.1).
Operative Technique
Hemorrhoid Exposure
The main hemorrhoidal masses are identified and delineated, usually in the “classical” locations corresponding to the sites of inferior hemorrhoidal vessels—left lateral right posterolateral, right anterior quadrants. The hemorrhoids are prolapsed out from the anal canal with an Allis clamp or forceps. Tension should be applied in order to visualize the mucocutaneous junction.
Dissection and Hemorrhoid Removal
 Figure 2.2 LigaSure™ hemorrhoidectomy is performed by applying the precise LigaSure™ forceps close to the edge of each pile. Completion of coagulation is signalled by the feedback sensors. |
A small V-shaped anodermal seal is formed by applying the precise LigaSure™ forceps close to the outer edge of the internal hemorrhoid (Fig. 2.2). The seal is then transected with scissors along the line of coagulum. Care should be taken in order to limit the
amount of tissue removed to minimize the risk of stricture (Fig. 2.3). Repeated applications of the device are performed and the excision is continued into the anal canal, lifting the pile from the internal anal sphincter (Fig. 2.4). The vascular pedicle is finally sealed by LigaSure™ and divided (Fig. 2.5).
amount of tissue removed to minimize the risk of stricture (Fig. 2.3). Repeated applications of the device are performed and the excision is continued into the anal canal, lifting the pile from the internal anal sphincter (Fig. 2.4). The vascular pedicle is finally sealed by LigaSure™ and divided (Fig. 2.5).
Final Control
The area is inspected with the Eisenhammer retractor to ensure hemostasis. The operation is terminated by placing a hemostatic absorbable gelatin sponge in the anal canal (Fig. 2.6). At the end of the operation, a single layer of nonadhesive gauze is used to dress the wounds. Finally, a large surgical dressing is applied to the buttocks and held in place with a bandage.
Treatment of Vascular Pedicles
In the LigaSure™ hemorrhoidectomy, pedicles are not transfixed, but sealed by LigaSure™ to avoid incorporation of the underlying sphincter in the ligatures.
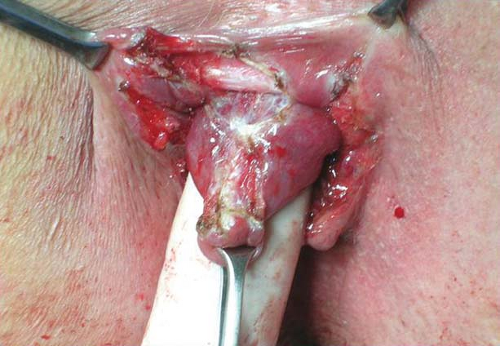 Figure 2.4 Repeated applications of the LigaSure precise are carried out to lift the pile from the internal anal sphincter (black narrow), taking care to avoid sphincter injuries. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




