Fig. 12.1
Left, Barium swallow showing distal esophageal narrowing, an air-fluid level, slow emptying of barium into the stomach, and a 5 × 6-cm epiphrenic diverticulum. Right, Esophageal manometry showing achalasia, with normal resting pressure of the lower esophageal sphincter but absent relaxation in response to swallowing
12.2 Operation
12.2.1 Patient Positioning
The patient is positioned supine on a beanbag on the operative table. Pneumatic compression stockings are used as prophylaxis against deep vein thrombosis, and preoperative antibiotics are administered prior to skin incision. A rapid sequence induction is performed to prevent aspiration of particulate matter lodged inside the diverticulum or filling the esophageal lumen of patients with underlying esophageal motility disorders, such as achalasia. A Foley catheter is then inserted; the lower extremities are placed in stirrups; and the beanbag is inflated to support the patient in the reverse Trendelenburg. Finally, the abdomen is prepped and draped.
12.2.2 Ports and Instruments
A 1-cm transverse midline incision is made onto the skin approximately 1 inch above the umbilicus (Fig. 12.2). The fascia is grasped with a Kocher clamp and a nick is made with a #15 blade; a Veress needle is inserted; a water drop test is performed; the abdomen is insufflated to 14 mmHg; and an 11-mm trocar is inserted into the abdominal cavity under direct visualization using a 0°, 10-mm laparoscope. Then three trocars are placed. Ports B and C are 11-mm working ports through which the graspers, the laparoscopic LigaSure™ Vessel Sealing System (Covidien, Minneapolis, MN) and the suturing instruments are introduced. Port D is a 12-mm port used for manipulation of a laparoscopic atraumatic Allis clamp; the LigaSure™, to take down the short gastric vessels; and the insertion of a laparoscopic stapler. Finally, a 5-mm incision to the left of the xiphoid process is made to insert a Nathanson retractor, which retracts the left lobe of the liver medially and upwards and exposes the diaphragmatic hiatus and the gastroesophageal junction. The Nathanson retractor is at last secured to the operative table. The 0°, 10-mm laparoscope is exchanged for a 30- or 45°, 10-mm laparoscope, which is used for the entire procedure. Because of its angled lens, this laparoscope allows superior visualization, especially when working in the mediastinum during the mobilization of the cranial portion of the diverticular neck.
Fig. 12.2
Operative ports in order of placement for laparoscopic treatment of epiphrenic diverticula; port A must be in the midline above the umbilicus
12.2.3 Operative Procedure
Step 1
Mobilization of the esophagus
Once all ports are placed, the patient is positioned in steep reverse Trendelenburg. Applying a laparoscopic Allis clamp near the gastroesophageal junction anteriorly starts the operation. This maneuver tents up the gastrohepatic ligament, which is divided with the Ligasure™ until the right diaphragmatic crus becomes visible. The phrenoesophageal ligament is divided from the apex of the right crus to the apex of the left crus, and the anterior vagus nerve is identified. The esophagus is then bluntly dissected away from the right crus to provide access to the posterior mediastinum. The posterior vagus nerve is then identified. The left pillar of the crus is then visualized and a retroesophageal window is created. A Penrose drain is passed around the esophagus, encircling both vagi nerves; it is used to apply caudad traction to the distal esophagus, which makes it easier to deliver the diverticulum closer into the abdomen.
Step 2
Exposing the neck of the diverticulum
The dissection is continued into the posterior mediastinum, where the diverticulum is located. After the diverticulum is discovered, it is bluntly dissected off the pleura and the esophageal wall until its neck is clearly isolated, to provide a safe access for the stapler. The exposure of diverticular neck is completed only after the most cranial portion of the neck has been adequately dissected (Fig. 12.3). Occasionally, the diaphragm is split anteriorly to gain access to a large diverticulum in the mediastinum.
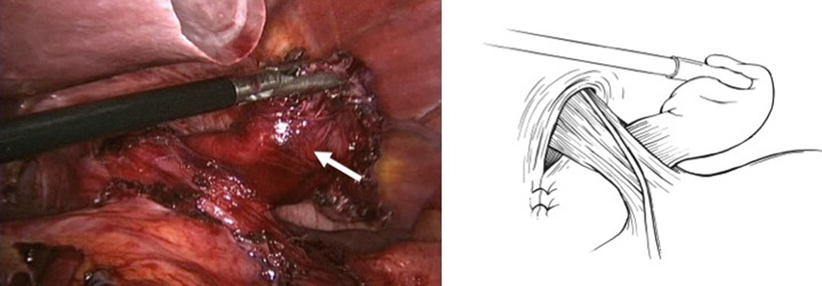
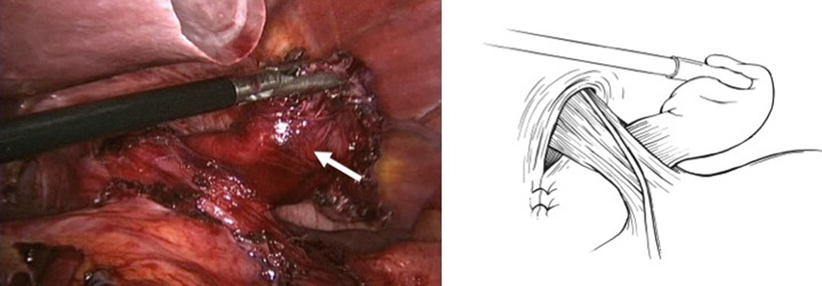
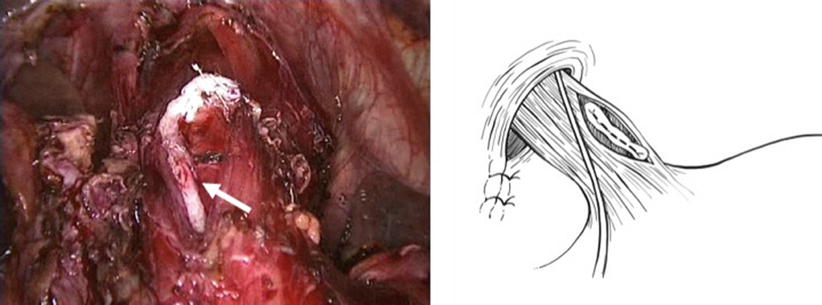
Fig. 12.3
Dissection and identification of the diverticulum (arrow)
Step 3
Stenting of the esophagus
A tapered-tip bougie (54–58 F) is then placed carefully and under direct vision into the esophagus to stent its lumen and prevent stenosis by stapling an excess of the mucosa and submucosa of the diverticular neck. To prevent the inadvertent introduction of the bougie into the diverticulum, the diverticular neck may be gently and loosely closed with a grasper.
Step 4
Stapling of the diverticulum
Once the bougie is in place, the neck of the diverticulum is then stapled with a roticulating laparoscopic stapler equipped with a 2.5-mm vascular cartridge and oriented longitudinally to the esophageal axis (Fig. 12.4). The bougie is gently withdrawn before the stapler is fired, to avoid backward dragging of the stapled mucosa and submucosa. The bougie is then always taken out of the patient’s esophagus.