Fig. 13.1
Setup of the operating room
13.2.2 Ports and Instruments
Five trocars (Fig. 13.2) are used for the procedure:
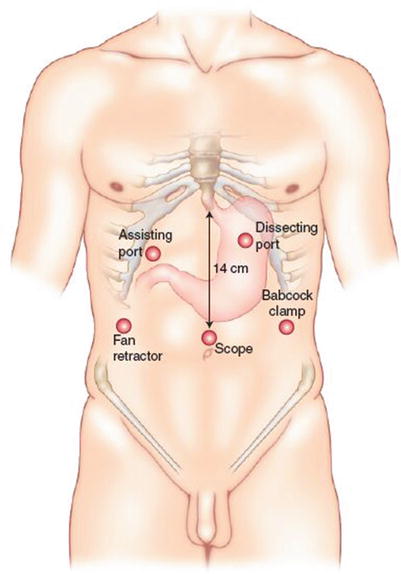
Trocar 1: Placed 14 cm inferior to the xiphoid process in the midline (or 1–2 cm to the left of the midline to be in line with the hiatus). It is used for a 30° camera.
Trocar 2: Placed in the left mid clavicular line (at the same level as trocar 1). It is used for a Babcock clamp, a grasper to hold the Penrose drain, or an instrument used to divide the short gastric vessels.
Trocar 3: Placed in the right mid-clavicular line (at the same level as the first two trocars). It is used for the insertion of a liver retractor.
Trocars 4 and 5: Placed under the right and left costal margins. They are used for the suturing and dissecting instruments.
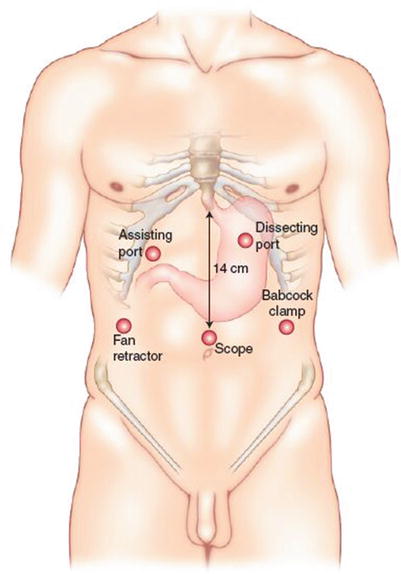
Fig. 13.2
The positions and functions of the five trocars
13.2.3 Operative Procedure
Step 1
Division of the gastrohepatic ligament, peritoneum, and phrenoesophageal membrane
The gastrohepatic ligament is divided, beginning above the caudate lobe of the liver (Figs. 13.3 and 13.4). The peritoneum and the phrenoesophageal membrane above the esophagus are transected with electrocautery, and the anterior vagus nerve is identified (Fig. 13.5). The left crus of the diaphragm is dissected downward toward the junction with the right crus (Fig. 13.6).
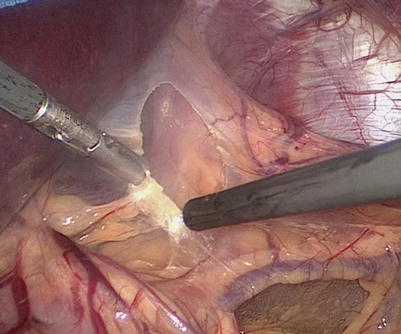
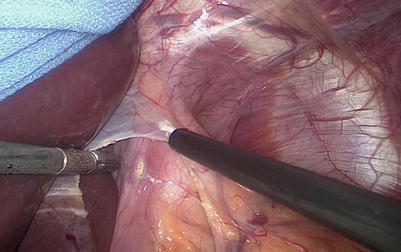
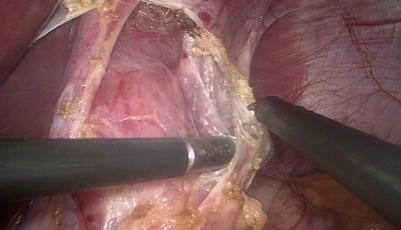
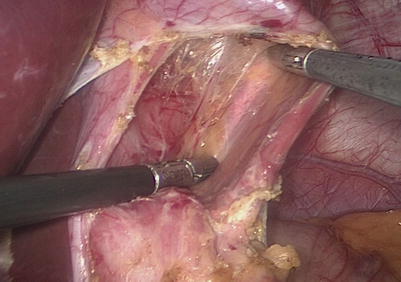
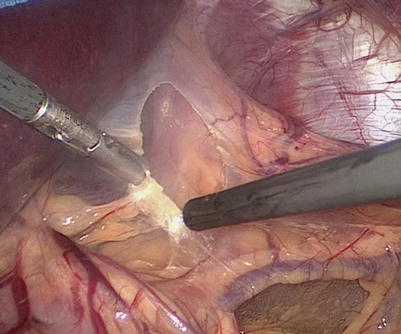
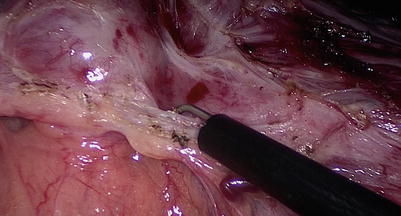
Fig. 13.3
Division of the gastrohepatic ligament
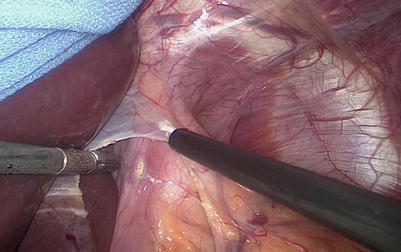
Fig. 13.4
Division of the gastrohepatic ligament
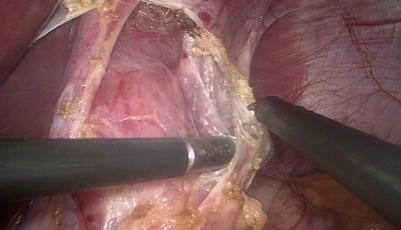
Fig. 13.5
Transection of the peritoneum and the phrenoesophageal membrane above the esophagus, using electrocautery
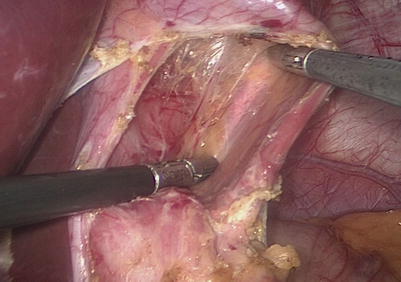
Fig. 13.6
The left crus of the diaphragm is dissected downward toward the junction with the right crus
Step 2
Dissection of the gastric component
The gastric component of the tumor is identified (Figs. 13.7 and 13.8), and the short gastric vessels are divided with a bipolar instrument (Figs. 13.9 and 13.10).
The tumor is dissected using a combination of the electrocautery and the bipolar instrument (Figs. 13.11, 13.12, 13.13, 13.14, 13.15, 13.16, 13.17, 13.18, 13.19, and 13.20). It is possible to identify the characteristic “mother of pearl” appearance of the tumor capsule. Particular attention is given to avoiding a thermal or traction injury to the mucosa.
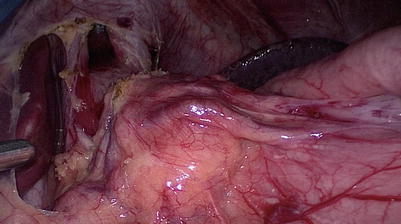
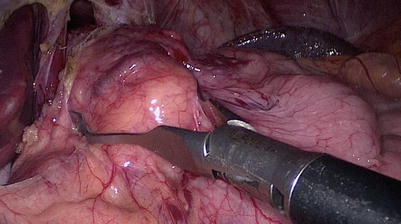
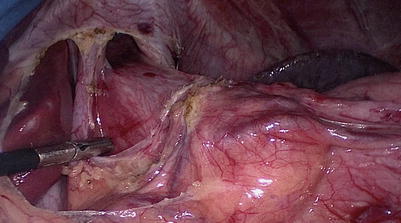
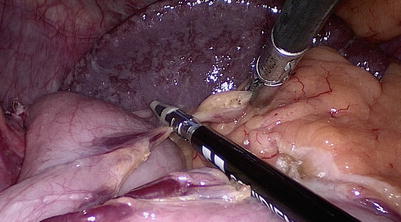
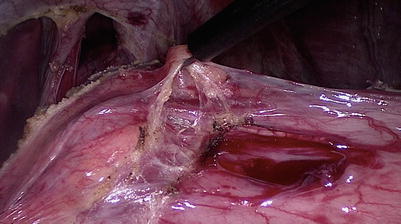
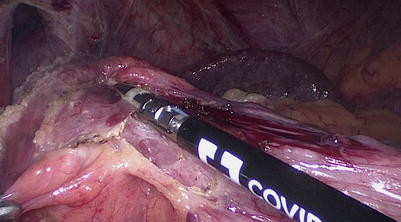
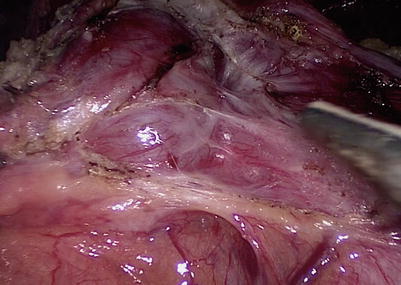
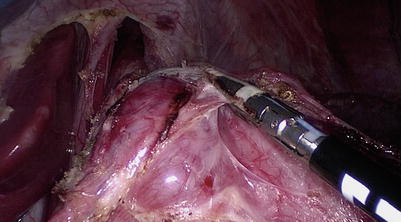
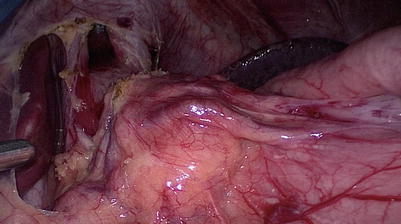
Fig. 13.7
Identification of the gastric component of the tumor
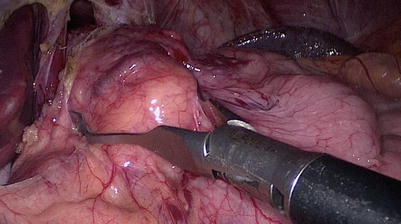
Fig. 13.8
Identification of the gastric component of the tumor
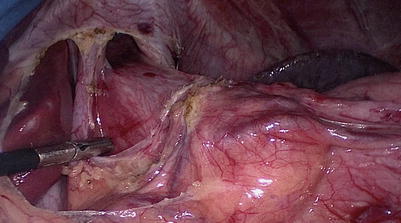
Fig. 13.9
Division of the short gastric vessels
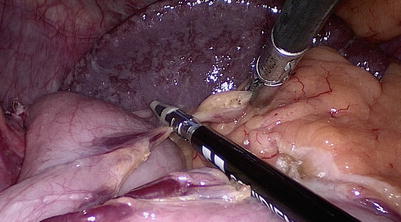
Fig. 13.10
Division of the short gastric vessels
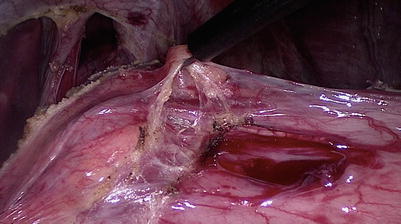
Fig. 13.11
Dissection of the gastric component of the tumor
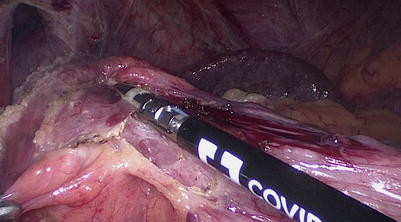
Fig. 13.12
Dissection of the gastric component of the tumor
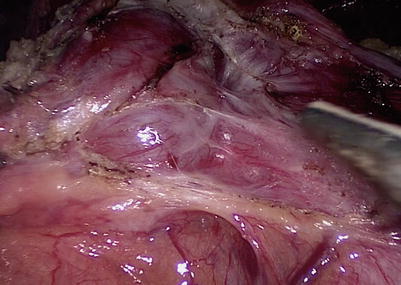
Fig. 13.13
Dissection of the gastric component of the tumor
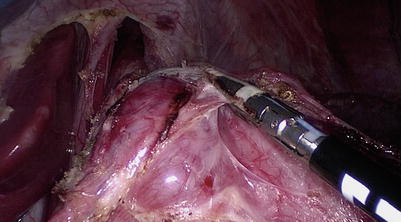
Fig. 13.14
Dissection of the gastric component of the tumor