Laparoscopic Low Anterior Resection with Transanal Anastomosis or Colonic J Pouch Creation
Sharon L. Stein
Conor P. Delaney
Laparoscopic low anterior resection with transanal anastomosis is performed primarily for oncologic indications. Patients with tumors invading beyond the muscularis mucosa or lymph node involvement should undergo enbloc resection of the rectum and mesorectum. Oncologic resections mandate negative margins: ideally 2 cm of uninvolved distal tissue in the rectum and anus although 1 cm may be acceptable in tumors with favorable pathology to preserve sphincter function. When patients present with low rectal cancers, it may be impossible to achieve appropriate margins while using a double-stapled technique. Some low lying early rectal cancers, circumferential lesions, or tumors with unfavorable pathologic findings may be inappropriate for local excision and a transanal approach should be considered. Transanal or coloanal hand-sewn anastomosis allows for removal of mucosa or internal sphincter providing greater distal margins, while preserving bowel continuity.
Occasionally, during surgical operations for benign disease, technical problems such as stapling misfiring, ischemia, or benign pathology such as low rectovaginal fistula, may call for a coloanal technique. Ability to perform a hand-sewn transanal anastomosis will allow the surgeon to reestablish bowel continuity when the patient might otherwise require a permanent colostomy.
Transanal techniques, while preserving intestinal continuity, have a greater incidence of frequent bowel movements and mild-to-moderate incontinence. Patients with poor preoperative candidates are poor candidates for this technique and should undergo creation of permanent colostomy. Patients with tumors invading the sphincters or into the lateral pelvic sidewalls should undergo abdominal perineal resection or pelvic exenteration and should not be considered for transanal anastomosis.
Laparoscopic surgery may be safely performed in experienced hands in a wide variety of patients. While laparoscopic surgery and small incisions are convenient in thin fit patients, morbidly obese patients and elderly patients are also candidates for laparoscopic proctectomy and may benefit from decreased incision lengths, earlier mobility, and decreased respiratory compromise. With appropriate retraction and preservation of appropriate oncologic margins, laparoscopic surgery can be performed on most operative candidates. Several preliminary studies on laparoscopic proctectomy have demonstrated functional and oncologic results equivalent to open surgery and a randomized trial is underway to assess the outcomes of laparoscopic proctectomy for cancer. Patients with extensive adhesions and scarring from past surgery may not be good candidates for laparoscopic surgery. In addition, laparoscopic proctectomy is an advanced laparoscopic procedure and should not be performed for oncologic indications by inexperienced laparoscopic surgeons.
Prior to surgery, all patients should undergo appropriate preoperative staging for the rectal neoplasia. Local, nodal, and metastatic evaluation of the tumor should be performed. Prior to surgery, a tumor biopsy and pathologic diagnosis should be established. A rigid proctoscopy and digital exam should be performed by the operating surgeon to evaluate tumor location, fixation, and appropriate surgical approach.
In addition, depth of invasion and nodal status should be established using either endorectal ultrasound or magnetic resonance imaging. Choice of exam should be based on local expertise and tumor staging. For T1 and T2 tumors, endorectal ultrasound is more accurate for staging, while in more advance T staging MRI has been shown to be more sensitive.
Advanced tumors should be evaluated for neoadjuvant therapy prior to surgical resection. T2 tumor with unfavorable histology, any T3 or T4 tumor, and any tumor with nodal involvement are candidates for preoperative chemoradiation. Assessment of appropriate oncologic margins should be performed preoperatively, as posttreatment regression of tumor does not necessarily equate with resolution of microscopic disease.
Metastatic evaluation includes computed tomography of the abdomen and pelvis and baseline CEA level, which may be useful for postoperative monitoring. In addition, there is an 8–10% rate of synchronous polyps or neoplasia and patients without obstructing lesions should have preoperative assessment of the entire colon and rectum.
All patients should have a preoperative evaluation of baseline continence. Personal history of fecal incontinence including nighttime soilage, incontinence to liquid, solid or flatulence should be addressed. Physical exam should include digital evaluation of sphincter tone and strength of contraction. Although anal manometry may be performed, digital rectal exam has been shown to be a better predictor of postoperative continence.
Patients should be consented for temporary ileostomy and should be aware of the possibility of a permanent colostomy. Temporary ileostomy is used in very low rectal anastomosis to protect the anastomosis during immediate postoperative period secondary anastomotic leak rates of up to 17%. Permanent colostomy may be necessary if the tumor is found to invade the sphincter muscles intraoperatively. Patients should have the opportunity to meet with an enterostomal therapist for preoperative counseling and should be marked for left- and right-sided stomas prior to surgical positioning.
Appropriate preoperative evaluation of medical comorbidities should be performed as indicated by patient history. All patients receive preoperative laboratory assessment including standard metabolic, coagulation, and blood count studies. Patients should also have type and cross match of blood for possible transfusion.
Preoperative bowel preparation is controversial. Although data demonstrate that bowel cleansing may not be necessary in all colon surgery, bowel preparation avoids leaving a column of stool in the diverted colon. In addition, bowel cleansing provides the ability to perform colonoscopy intraoperatively if not completed preoperatively. The authors routinely perform preoperative bowel preparation.
Essential equipments for successful laparoscopic low anterior resection include 5 or 10 mm 30-degree camera for adequate visualization especially vital in the pelvis for deep dissection, nontraumatic laparoscopic bowel graspers, laparoscopic scissors with electrocautery capability, and an energy device or staplers for vessel transection. A Lonestar retractor and lighted Hill Ferguson anal retractors facilitate perineal dissection.
Prophylaxis
Prior to incision, antibiotics with appropriate anaerobic and aerobic coverage should be given and redosed every 4 hours throughout the operation. Subcutaneous low-dose molecular heparin is given prior to induction. Sequential compression devices are used for all patients intraoperatively. Skin preparation of perineum and perianal region is performed per standard protocol.
Positioning
The authors position patients in modified lithotomy position in yellow-fin or padded stirrups. Care should be made to ensure that the lower leg is well protected to prevent injury to the perineal nerve. An electric operating table is lined with either a gel pad or bean bag to reduce the risk of pressure injury and facilitate varied positioning throughout the operation. An orogastric tube, placed after induction of anesthesia, allows for decompression of the stomach intraoperatively and is removed prior to extubation.
Steps in Laparoscopic Low Anterior Resection with Coloanal Anastomosis
Abdominal exploration
High ligation of inferior mesenteric artery and vein
Splenic flexure takedown and left colon mobilization
Protectomy with total mesorectal dissection
Perineal dissection
Removal of specimen
Creation of a neorectum
Anastomosis
Creation of diverting ileostomy
Abdominal Exploration
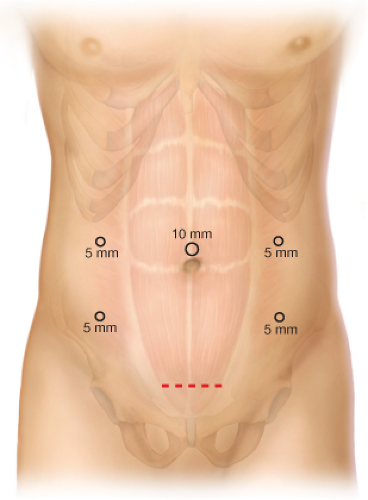
The abdomen is entered using an open technique and Hasson port. Additional ports are placed under laparoscopic guidance. Our typical port placement is shown in Figure 15.1.
Initial evaluation occurs to determine laparoscopic feasibility of the operation. If significant adhesions from prior surgery exist, the decision is made to convert to open surgery. The abdomen is evaluated for metastatic disease. The peritoneum is inspected for signs of tumor implantation. Attention is drawn to the liver, which may be elevated to examine the inferior aspect. The ovaries are inspected in female patients, as there is a 3–8% incidence of ovarian metastasis in colorectal cancer patients. The pelvis is assessed to evaluate for lateral extension of the tumor. In the case of large bulky tumor, it may be difficult to assess invasion of sphincter muscles preoperatively, and decision to convert to abdominal perineal resection may occur intraoperatively.
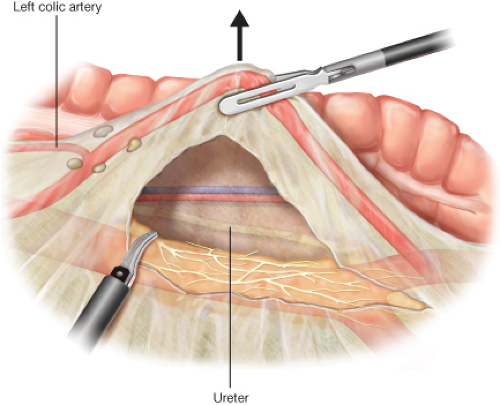
High Ligation of Inferior Mesenteric Artery and Vein (Fig. 15.2)
The patient is placed in Trendelenburg, left side up to isolate the left colon from the small bowel. The superior hemorrhoidal vessels are elevated at the sacral promontory and dissected in the open space caudal to the vessels. Branches of the hypogastric nerves lying between the aorta and the inferior mesenteric artery are preserved and
swept caudally toward the aorta. The left colic artery is conserved to maintain blood flow to the left colon. The left ureter must be definitively identified and preserved prior to transection of the inferior mesenteric artery. The artery is transected using a stapler, clips, or an energy device. A stapler is placed through the colon extraction site, most commonly the left lower quadrant incision. If an energy device is used, three firings (two proximal and one distal) are used prior to transection. The inferior mesenteric vein is located proximal to the pancreas and ligated. High ligation of the inferior mesenteric artery and vein are essential for adequate colonic length. In situations where the left colon does not reach the anus comfortably, the left colic artery may be sacrificed, but care must be taken to ensure that this does not compromise anastomotic blood supply.
swept caudally toward the aorta. The left colic artery is conserved to maintain blood flow to the left colon. The left ureter must be definitively identified and preserved prior to transection of the inferior mesenteric artery. The artery is transected using a stapler, clips, or an energy device. A stapler is placed through the colon extraction site, most commonly the left lower quadrant incision. If an energy device is used, three firings (two proximal and one distal) are used prior to transection. The inferior mesenteric vein is located proximal to the pancreas and ligated. High ligation of the inferior mesenteric artery and vein are essential for adequate colonic length. In situations where the left colon does not reach the anus comfortably, the left colic artery may be sacrificed, but care must be taken to ensure that this does not compromise anastomotic blood supply.
Splenic Flexure Takedown and Left Colon Mobilization (Figs. 15.3 and 15.4)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree