23 Jaundice and pruritus
Case
A 50-year-old female presented with a 2-week history of episodic right upper quadrant pain that radiated around the costal margin to the back. Similar pains had occurred over 5 years. The current episode had persisted, although fluctuating over several days with the development of jaundice, pale stools and dark urine. Serum alkaline phosphatise was 400 IU/L and alanine aminotransferase (ALT) 300 IU/L. Physical examination revealed a jaundiced patient in obvious discomfort with right upper abdominal quadrant tenderness. An abdominal ultrasound examination was performed. This revealed no cholelithiasis but a dilated common bile duct of 1.2 cm diameter; no stones were seen. Subsequently, an endoscopic ultrasound study demonstrated a gallstone within the distal common bile duct. At endoscopic retrograde cholangiopancreatography with sphincterotomy, the stone was removed. The patient’s symptoms and biochemical abnormalities resolved. She subsequently underwent laparoscopic cholecystectomy and remained well.
Introduction
Jaundice is yellow pigmentation of the sclera, skin, and mucous membranes caused by deposition of bilirubin in tissue. Jaundice becomes apparent when the serum bilirubin level rises above 50–75 μmol/L (normal: 3–15 μmol/L). It is most often associated with hepatocellular dysfunction or cholestatic syndromes including biliary obstruction, and is often associated with pruritus. The history and physical examination of the patient with suspected liver disease and an approach to abnormal liver function tests are discussed in Chapter 24. Here, bilirubin physiology and diagnostic methods are outlined, focusing on the clinical approach to patients with obstructive jaundice.
Physiology
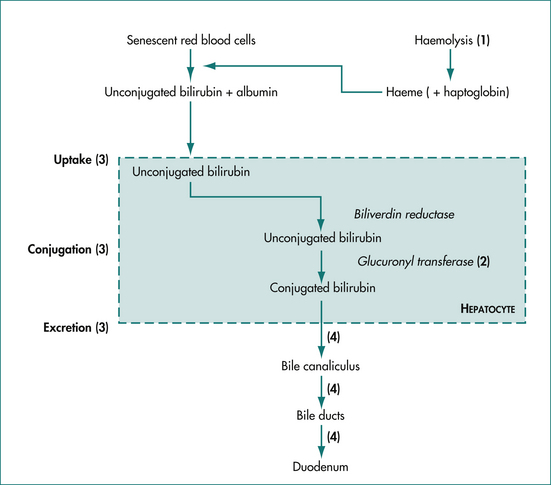
Jaundice results from either increased production and/or decreased excretion of bilirubin. The metabolism of bilirubin is summarised in Figure 23.1. Under normal conditions, 80% of serum bilirubin is generated by senescent red blood cells, which are broken down by the reticuloendothelial system in the spleen, liver and bone marrow. The released haeme (ferroprotoporphyrin IX) is oxidatively cleaved to biliverdin and then bilirubin, which is tightly bound to albumin and transported in the serum. The other 20% of serum bilirubin arises from the breakdown of other haeme-containing proteins (e.g. cytochrome, myoglobin and haeme-containing enzymes) and ineffective erythropoiesis (the premature breakdown of red cells in the bone marrow before release). Bilirubin, which is lipid soluble, is made water soluble by conjugation in the liver.
Jaundice may be caused by obstruction or overloading at various points in the bilirubin metabolism pathway (Fig 23.1). The proportions of conjugated and unconjugated bilirubin detected in the serum depend on the site of the obstruction or overloading. Haemolysis or reabsorption of a haematoma leads to an unconjugated hyperbilirubinaemia because the hepatocytes become overloaded. Reduced uptake and rates of conjugation will likewise lead to increases in serum unconjugated bilirubin.
Measurement of serum bilirubin
The normal range for serum bilirubin is 3–15 μmol/L in adults. Bilirubin is classified as direct (conjugated) and indirect (unconjugated). This terminology is derived from the commonly used assay that makes use of a diazo reaction. Diazotised aromatic amines cleave the bilirubin molecule into two identical molecules, which are bound to the azo compound. These are measured spectrophotometrically. In an acidic aqueous media, conjugated bilirubin reacts ‘directly’ with the azo compound; whereas unconjugated bilirubin requires the addition of an accelerator molecule such as alcohol, thus reacting ‘indirectly’.
The causes of jaundice are typically classified into three groups corresponding to the site of impaired bilirubin metabolism: prehepatic, hepatic and posthepatic (cholestasis, obstruction). This classification is clinically useful when evaluating patients with jaundice or hyperbilirubinaemia. There are distinctive clinical features and liver function test profiles and clinical presentations for each group (Table 23.1). These help the physician to identify the likely site of impaired bilirubin metabolism, narrow the differential diagnosis, and then order the most appropriate investigations.
Table 23.1 Clinical features and liver function test profiles in hepatic (hepatocellular) and cholestatic (or obstructive) jaundice
| Suggests hepatocellular jaundice | Suggests obstructive jaundice | |
|---|---|---|
| Clinical features | Nausea, anorexia, fatigue, myalgia, known infectious exposure, IV drug use, blood transfusions, alcohol, medication abuse, positive family history of liver disease or jaundice | Pain, pruritus, dark urine, pale stools, fever, past biliary surgery, weight loss, older age |
| Transaminases (AST, ALT) | ++ (> 3 × normal) | + (< 3 × normal) |
| Alkaline phosphatase | Normal to increased (< 3 × normal) | ++ (> 3 × normal) |
| INR or prothrombin time after vitamin K | Does not correct | Corrects if extrahepatic obstruction |
ALT = alanine aminotransferase; AST = aspartate aminotransferase; INR = international normalised ratio.
Prehepatic jaundice
Isolated unconjugated hyperbilirubinaemia is a common clinical problem. Patients typically present with mildly elevated serum bilirubin but normal levels of serum transaminases and alkaline phosphatase (refer to Ch 24 for a detailed discussion of liver function tests). The serum bilirubin is almost entirely unconjugated. Hepatocellular function and biliary excretion are normal.
Hepatic jaundice
Hepatic jaundice may be acute or chronic in origin. These two groups have different clinical presentations and liver function test profiles, but there may be considerable overlap. The level of hyperbilirubinaemia can vary greatly and it is seldom a clue to the diagnosis (Ch 24).
Obstruction or cholestasis
Obstructive jaundice occurs when bile flow through the extrahepatic biliary tree is impaired, usually by a stone or tumour. Intrahepatic cholestasis occurs when excretion of conjugated bilirubin from the liver cell into the bile canaliculus is disrupted. The most common cause is a drug reaction, but some cases of viral hepatitis and some chronic liver diseases (e.g. primary biliary cirrhosis) can also cause cholestasis.
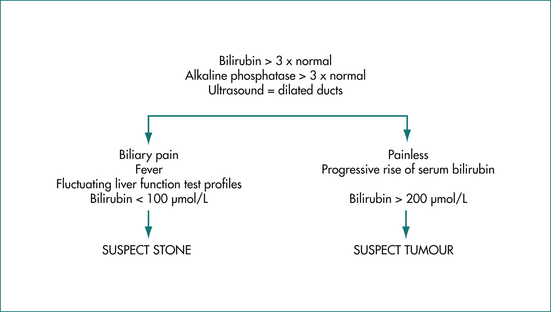
The clinical features and liver function test abnormalities produced by cholestasis and obstruction are similar. Both present with prominent jaundice, dark urine and pale stools. Pruritus may be present if the cholestasis or obstruction is longstanding. The serum alkaline phosphatase level is usually greater than three times the normal level, transaminases are usually less than three times normal, and serum bilirubin concentration is elevated. It should be noted that in acute biliary obstruction, as may occur in choledocholithiasis, serum transaminase levels rise earlier than the alkaline phosphatase. The prothrombin time may be prolonged due to poor absorption of vitamin K but is rapidly corrected by administering parenteral vitamin K in obstruction. Constant pain in the right upper quadrant may be present. Severe episodic pain lasting a few hours suggests stones in the bile duct. Painless jaundice is the hallmark of malignant biliary obstruction commonly seen in patients with pancreatic cancer (Ch 17) (Fig 23.2).
Clinical Syndromes
Prehepatic jaundice
Gilbert’s disease
Other causes of unconjugated hyperbilirubinaemia are bilirubin overproduction, impaired uptake by hepatocytes, or impaired delivery to the liver (Table 23.2).
Table 23.2 Mechanisms for the development of unconjugated hyperbilirubinaemia with typical examples
| Mechanism | Example |
|---|---|
| Impaired conjugation | Gilbert’s syndrome |
| Impaired uptake | Drug, e.g. rifampicin |
| Overproduction: | |
| Impaired delivery | Portal systemic shunt |
Bilirubin overproduction
Overproduction arises from accelerated red blood cell destruction and is a common cause of prehepatic jaundice. Examples include chronic haemolysis seen in patients with prosthetic heart valves, hereditary spherocytosis and glucose-6-phosphate dehydrogenase deficiency, or acute intravascular haemolysis seen in patients with sickle cell crisis or transfusion reactions. Haemolysis can be diagnosed on the basis of a characteristic blood film, low haptoglobin and high lactate dehydrogenase levels.
Cholestatic and obstructive jaundice
Intrahepatic cholestasis
Viral hepatitis, particularly hepatitis A, can occasionally cause intrahepatic cholestasis. Acute hepatitis A can cause a cholestatic hepatitis with an elevated alkaline phosphatase level, fever, arthralgia and jaundice lasting 2–8 months. When chronic alcohol consumption leads to significant fatty infiltration of the liver, cholestasis can also occur. These diseases are discussed in Chapter 24.