14 Chronic diarrhoea and fatty stools
Case
A 48-year-old man presents with a history of frequent watery diarrhoea for the last 3 months, up to six times daily. He travelled to Southeast Asia, including Thailand, 3 months ago. There has been no blood in the stools and they have not been excessively pale or difficult to flush away. After he drinks milk or eats gluten-containing foods, his symptoms are worse.
Introduction
Chronic diarrhoea can be simply defined as the frequent or urgent passage of unformed stool for at least one month. As with acute diarrhoea (Ch 13), a careful history and physical examination will often help suggest the diagnosis and direct investigations.
History
The clinician needs to determine what the patient means by diarrhoea. The patient should be asked about the frequency and consistency of the stools. Diarrhoea needs to be distinguished from rectal urgency alone or faecal incontinence (Ch 16).
Clues to the cause of the diarrhoea can be obtained from the history and examination (Table 14.1). Small-volume, frequent stools suggest large bowel disease and tenesmus (a constant sense of the need to defecate) suggests rectal involvement. Large-volume, watery stools are consistent with small bowel disease, whereas obvious clinical steatorrhoea with pale, bulky, oily stools that float suggests the presence of small bowel or pancreatic disease.
Table 14.1 Clinical features in chronic diarrhoea
| Clinical feature | Conditions to consider |
|---|---|
| Young age | Coeliac disease, inflammatory bowel disease, lactase deficiency, irritable bowel syndrome |
| Oil droplets in stool | Pancreatic insufficiency |
| Previous surgery | Bacterial overgrowth, dumping, post vagotomy diarrhoea, ileal resection, short bowel syndrome |
| Peptic ulcer | Zollinger-Ellison syndrome |
| Medications | Laxatives, magnesium antacids, antibiotics, lactulose, colchicine |
| Frequent infections | Immunoglobulin deficiency |
| Marked weight loss | Thyrotoxicosis, malignancy, malabsorption |
| Arthritis | Inflammatory bowel disease, Whipple’s disease, hypogammaglobulinaemia, Yersinia spp. |
| Hyperpigmentation | Whipple’s disease, Addison’s disease, coeliac disease |
| Fever | HIV, inflammatory bowel disease, lymphoma, Whipple’s disease |
| Flushing | Carcinoid syndrome |
| Chronic lung disease | Cystic fibrosis |
| Neuropathy | Diabetes mellitus, vitamin B12 deficiency, amyloidosis |
| Family history of diarrhoea | Colon cancer, coeliac disease, inflammatory bowel disease |
The presence of blood may indicate local anal bleeding or other colonic disease. Bright red blood that is separate from the stool is consistent with an anal or rectal cause, but may occur with more proximal colonic disease. Altered blood, or blood with the stool is in keeping with higher colonic bleeding, such as from inflammatory bowel disease or colon cancer (Ch 10).
Symptoms associated with the diarrhoea may also provide valuable information about the nature of the underlying disease process. Weight loss suggests an organic disorder and may be marked with malabsorption, carcinoma or inflammatory bowel disease. Large joint arthritis or sacroileitis suggests inflammatory bowel disease. Yersinia infection and Whipple’s disease can also present with arthritis.
Physical Examination
Evidence of malnutrition and wasting should be sought and the skin examined for rashes, pigmentation and evidence of nutritional deficiency. There may be evidence of iron deficiency (pallor, cheilosis, glossitis and koilonychias) or vitamin B12 deficiency (peripheral neuropathy, glossitis and knuckle pigmentation). Protein deficiency may result in peripheral oedema and white nails.
Further clues to the cause of diarrhoea may be obtained from abdominal examination. An abdominal mass or liver secondaries may be identified. A rectal mass may be present on rectal examination, or faecal impaction, particularly in elderly patients, may be noted and sphincteric tone should be tested to rule out faecal incontinence. Perianal disease with fissures, fistulae and abscesses is common in Crohn’s disease (Ch 12).
Assessment
The history and physical examination will often direct the order and nature of investigations.
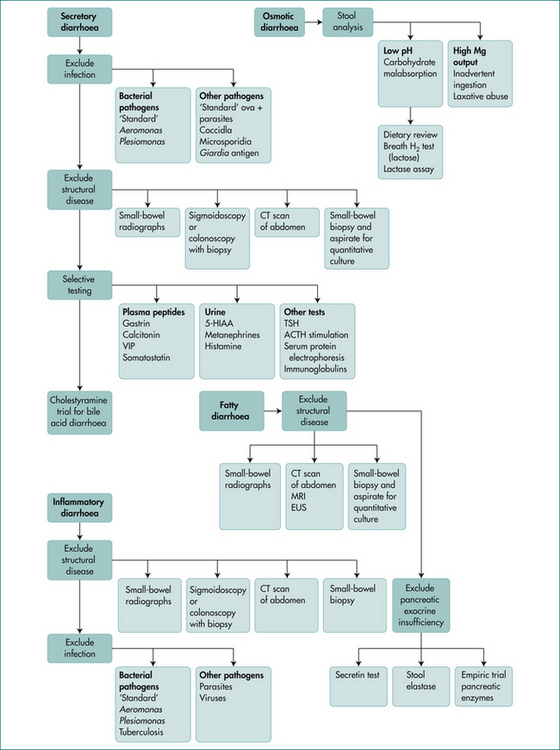
Categorising the pattern of diarrhoea into osmotic (ceases on fasting), secretory (persists in fasted state), inflammatory (passage of blood) and classical steatorrhoea helps in directing investigations though overlap can occur. (See Figs 14.1 and 14.2.)
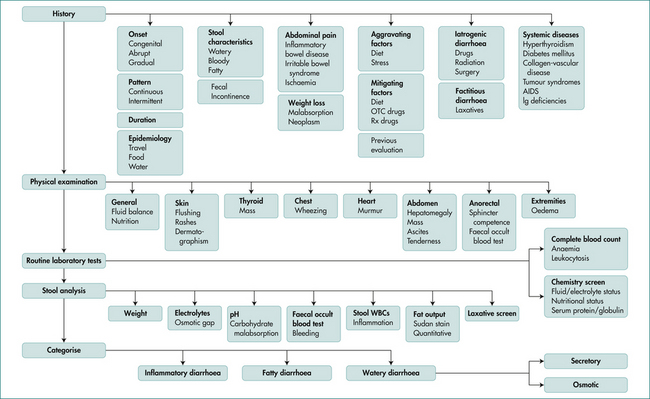
Figure 14.1 Flow chart 1.
Adapted from Fine, KD, Schiller, LR. AGA technical review on the evaluation and management of chronic diarrhea. Gastroenterology 1999; 116:1464.
Malabsorption
The basic physiological problem the body faces in assimilation of food is the passage of nutrients across the limiting cell membrane of the enterocyte. The problem is solved by breaking food particles down to basic components (digestion) and the insertion of special carrier proteins into the absorptive cells to facilitate absorption. The term ‘malabsorption’ is generally used to encompass both impaired digestion and defective absorption. A classification of malabsorption is shown in Box 14.1.
Box 14.1 Classification of malabsorption and example of causes
Physiology
Understanding malabsorption requires knowledge of the physiology of normal digestion and absorption.
The enterocyte
The small intestine is lined by specialised cells called enterocytes and, like all cells, they are surrounded by a limiting membrane (a lipid bilayer) with the function of preventing the loss of cytosol and the entry of unwanted molecules. The purpose of digestion is to break down nutrients into molecules small enough to be absorbed. The lipid bilayer allows diffusion of fats into the cell and is equipped with carriers to enable the absorption of sugar and amino acids. Anatomical modifications in the small intestine (valvulae conniventes, villi and microvilli) increase the luminal surface area by approximately 600-fold.
Fat assimilation
Enterocytes absorb free fatty acids and monoglycerides and carry fats to the interior surface membrane. Bile salts are finally absorbed in the terminal ileum. Within the enterocyte, monoglycerides are re-esterified to triglycerides and coated with small amounts of protein to form a chylomicron. These pass into the mesenteric lymphatics and enter the blood stream via the thoracic duct.
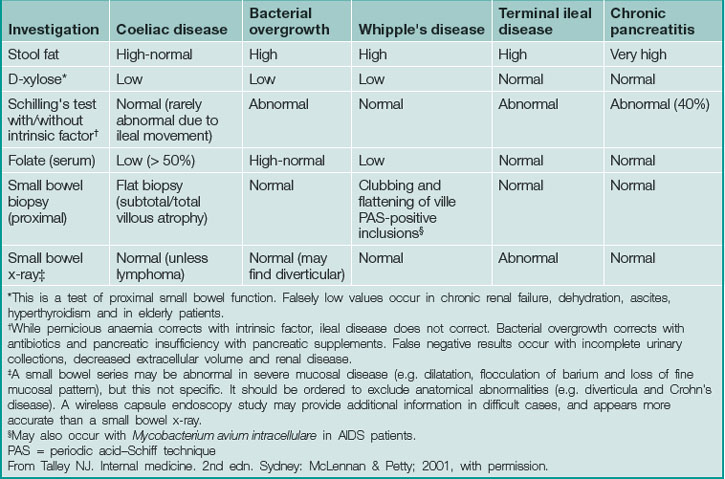
Clinical Approach to the Patient with Malabsorption
Diagnosis in malabsorption requires firstly suspecting its presence, secondly confirming its existence and thirdly demonstrating the cause (Table 14.2).