Fig. 36.1
Retrograde pyelogram showing midrenal calyceal diverticulum; stone seen as filling defect
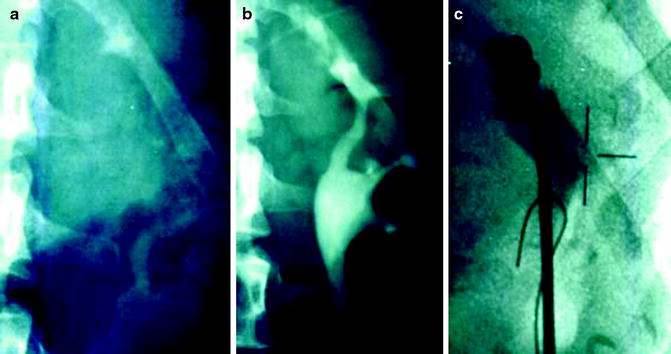
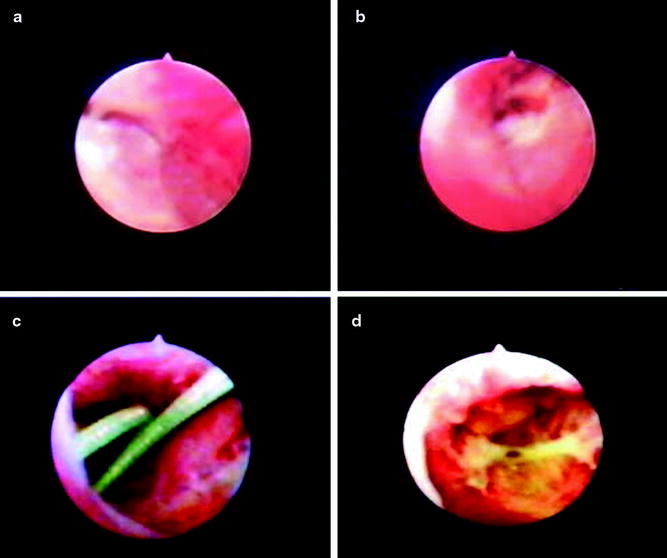
Fig. 36.2
(a) KUB depicting well fragmented stone after E-SWL in upper pole of left kidney. (b) IVP showing the stone gravel in an upper pole calyceal diverticulum. (c) Flexible ureteroscope at the mouth of a stone-bearing diverticulum. Contrast injection delineates the spacious diverticulum cavity
Before performing RIRS, an existing urinary infection must be treated with culture-directed antibiotics. A sterile urine culture should be confirmed within 5 days of the planned surgery. Broad-spectrum or culture-specific antibiotics should be utilized preoperatively for prophylaxis. In patients with relapsing UTI antibiotic coverage should be started prior to the procedure even when the preoperative urine is found to show no growth.
RIRS is best performed in the intubated patient under general anesthesia in the lithotomy position. Occasionally, a procedure can be performed with regional anesthesia or even local anesthesia but kidney movement with extensive breathing excursion may increase the technical difficulty of performing the delicate instrumentation. At our institution, the procedure is performed as a day-surgery case, with plans for the patient to return home under supervision the same evening. The procedure is performed on a multipurpose endoscopy and lithotripsy table (Modulith, Karl Storz Medical; Kreuzlingen, Switzerland), which allows for endoscopic surgery with real-time fluoroscopy as well as the simultaneous employment of E-SWL during RIRS for larger stone burden or stone portions which cannot be readily and safely accessed with the flexible endoscope.
Equipment
Table 36.1 lists the equipment commonly used at our institution for RIRS and the treatment of calyceal diverticulum and infundibular stenosis (Table 36.1).
Table 36.1
Equipment for retrograde intrarenal surgery for calyceal diverticula and intrarenal stenoses
Basic equipment (manufacturer) | Alternatives |
|---|---|
21-F rigid cystoscope (Karl Storz)a | Wolfb, Olympusc, ACMId scopes |
9.5-F semirigid ureteroscope (Karl Storz)a | Ureteral balloon dilator set |
Ureteral serial dilator set (Cook, Microvasive) | |
7.5-F flexible ureteroscope (FleXX2, Karl Storz) (Olympus-ACMId)a | |
Holmium laser system w/200 μm fiber (ACMI-Dornier) | 3-Fr EHL (Calcutript, Storz) |
1.6-Fr EHL (Storz)a | |
3-Fr Bugbee electrode | |
Nitinol tipless basket (Cook) | 4 wire baskets |
2/3 pronged grasper (Cook, Microvasive) | |
5-F angiographic catheter (Cook) | |
0.038-in. Bentson wire (Cook) | 0.038-in. or 0.035-in. straight wire |
Double-J stent (Cook, Microvasive) | |
Xenon light source, irrigation tubing, suction apparatus | |
Optional equipment (manufacturer) | |
0.035-in. Glide wire (Microvasive) | |
8-Fr or 10-Fr coaxial catheters (Cook, Microvasive) | |
Multi-purpose endoscopy table with fluoroscopy and simultaneous E-SWL (Storz Modulith , Dornier MFL5000, Siemens Lithostar) | |
Access to the Kidney
After cystoscopy, a retrograde pyelography is performed under fluoroscopic control; the film is stored for further reference during the procedure. After a safety 0.038-in. guide wire is placed into the renal pelvis, diuresis is induced with furosemide (weight adjusted; 0.25 mg/kg) to reduce the risk of pyelorenal reflux and infectious complications.
If there is no previous stenting, we routinely use a graduated 9.5-Fr semirigid ureteroscope to optically dilate the ureter in preparation for flexible upper tract endoscopic surgery. The semirigid instrument is advanced over a second 0.038-in. working wire under direct vision as far as the scope can reach and then is withdrawn. In cases where the semirigid ureteroscope cannot be advanced into the ureter, an indwelling stent is placed to allow the narrow ureter to passively dilate for 10–14 days. Access to the kidney is then usually possible without difficulty.
If a stent was placed previously, it is removed after a safety wire has been placed into the kidney. A flexible ureterorenoscopy (7.5-Fr) is then advanced into the kidney alongside the safety wire. If difficulty engaging the orifice is encountered, the scope can be railroaded over a second working wire and up into the renal pelvis. Access sheaths are rarely used in a straightforward case, but they can be helpful in cases of patients with coagulopathy (reduced risk of bleeding), in cases of larger stone burden in the kidney (improved visibility and more expeditious removal of stone particles), and occasionally for increasing fulcrum to negotiate a tight access of the scope into a stenotic area in the kidney.
RIRS for Intrarenal Stenoses
Flexible upper tract endoscopy with analog—and more recently digital—ureterorenoscopes allows selective and complete evaluation of the entire renal collecting system in all but rare cases of severely abnormal intrarenal anatomy. Using a camera system with up to 15 times magnification, the intrarenal pathology such as the entry point to the narrow diverticulum or stenosed calyceal neck, the area of MSK stones protruding from under the papilla, or the area of stone gravel encased in fibrinous matrix can be identified. The access point to a diverticulum usually presents itself as a small dimple, anywhere from the fornix of the calyx to the infundibulum. Dilute contrast is injected through the scope directly into the area of the perceived opening to identify and confirm the diverticulum fluoroscopically (Fig. 36.2c). If a diverticulum or stenotic segment fills with contrast but the entry point is not clearly identifiable, the so-called “Blue Spritz” technique can be used. Saline colored by methylene blue is instilled through the work channel of the flexible scope into the collecting system. The whole system then is decompressed by suction. Residual blue dye trapped in the diverticulum then slowly trickles out from the stenotic area thus allowing the identification of the entry point.
Once the access into the diverticulum is identified, a 0.038-in. guide wire is advanced through the 7.5-Fr flexible ureteroscope past the neck into the diverticulum, and an attempt is made to coil as much of the wire as possible inside. The instrument is cautiously withdrawn, leaving the guide wire coiled in the diverticulum. The instrument then is reintroduced alongside the guide wire and advanced back up into the kidney. At this point, access of the ureteroscope into the diverticulum is negotiated. Depending on the length and width of the “infundibulum” access is gained either by advancing the scope over a second guide wire in case of a wider, accommodating “infundibulum” or by performing a Holmium laser incision of the intrarenal stricture with a 200 μm laser fiber in case of a short “infundibulum.” In case of a longer, narrow access a 3-Fr zero-tip dilating balloon (Microvasive) which dilates up to 12 Fr can be inserted through the work channel of the 7.5-Fr flexible ureteroscope and is inflated under fluoroscopic or endoscopic control [18]. So incision of the neck with the Holmium laser is used for short connections into a wide diverticulum or when the diverticulum presents as an area of bulging mucosa. Balloon dilation is preferred for longer connections as the use of the laser incision in such circumstances would have a higher risk of bleeding and extravasation. The flexible ureteroscope is then advanced into the diverticulum, while the surgeon inspects the neck for adequacy of dilatation and the stone/s can then be treated.
RIRS for Stones in a Diverticulum
If the neck accommodates a Nitinol tipless basket (Cook), stones less than 5 mm may be removed intact with the basket. The tipless basket reduces risk of mucosal trauma with forward basketing. Stones that are too large for direct removal are fragmented and vaporized with the Holmium laser using a 200 μm laser fiber. Larger stones can be treated expeditiously by simultaneously employing intracorporeal laser lithotripsy and E-SWL. Fragments are then removed actively with the Nitinol basket if they are larger than 3 mm; the rest are flushed out of the diverticulum and are left for spontaneous passage from the renal collecting system.
In a first time treatment of a diverticulum containing stone usually no attempt is made to fulgurate the mucosa of the diverticulum since there is no data to suggest that this maneuver reduces stone recurrence or infection.
Once stone treatment is completed we place a double-J pigtail stent across the widened infundibulum and coil it in the diverticulum cavity if space permits this. Otherwise, the upper curl may be placed in the renal pelvis. The distal placement of the stent then is checked endoscopically. A Foley catheter is placed in the bladder and withdrawn in recovery before patient discharge.
RIRS for Stones Associated with MSK or Retained in Fibrinous Matrix after E-SWL
In patients with MSK and stones, the first step of RIRS is to assess the renal collecting system and to “take inventory” of all stones freely mobile in the collecting system (target 1) and of the stones trapped partially under mucosa (target 2). The target 2 areas are marked on a stored retrograde pyelogram film with a marker so as to assure eventual complete removal of all accessible stone. Depending on the overall stone burden in the kidney simultaneous E-SWL can be utilized to accelerate stone fragmentation. If simultaneous E-SWL is performed the Holmium laser incision of tissue trapping the partially exposed stones is performed first to ascertain optimal visibility as the use of E-SWL will cause some minor oozing from the parenchyma which may compromise visibility for precise and safe Laser incision. The laser incision itself basically does not result in any bleeding as the tissue covering the stones is thin and rarely vascularized. “Liberation” of trapped MSK stones is usually started in the lower pole region as access and treatment of the lower pole is technically more challenging and therefore is best undertaken first. Using the roadmap retrograde pyelogram we approach all calyces from the bottom up until all are accessible, i.e., visible stone has been addressed.
In patients with stone gravel retained in fibrinous matrix after E-SWL usually only one calyx is involved and this is mostly in the lower pole or an otherwise dependent calyx. Careful inspection of the renal collecting system using the plain KUB film and the retrograde pyelogram for guidance will allow identification of the stone-bearing calyx. In most cases a small piece of stone may be seen poking through the matrix or the irregular appearance of the occluded calyx will identify the location (Fig. 36.3a). Holmium laser incision is then cautiously performed to liberate the stones which usually are found well fragmented and can be removed completely with Nitinol baskets (Figs. 36.3b–d and 36.4).