Component
Function
Surgeon console
3-D laparoscopic image projected from patient side cart camera
Master controls to direct patient side cart instruments
Foot pedal to adjust camera view
Foot pedal (“clutch”) to switch between first and third robotic arms
Foot pedals to apply monopolar and bipolar cautery
Master display to adjust video and audio properties of system
Patient side cart
Motorized cart to position robot
Robotic camera arm
Three robotic instrument arms
Vision cart
High-definition monitor of laparoscopic camera
Image processing software

Fig. 15.1
Robotics console
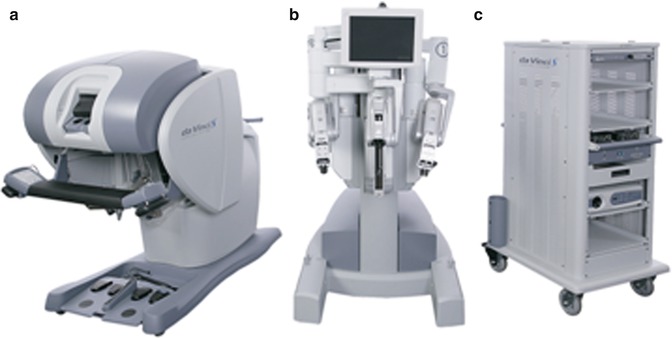
Fig. 15.2
(a) Robotic Console (b) Robot (c) Patient Cart
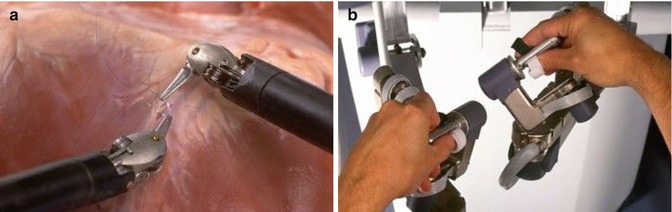
Fig. 15.3
(a) Robotic needle drivers (b) Robotics console joysticks
The operating room configuration depends on the procedure performed and the layout of the room. The patient side cart is positioned at the bedside during surgery. It includes either three or four robotic arms that respond to the commands of the surgeon at the surgeon console. The robotic arms move around fixed points at the level of the anterior abdominal wall, which may reduce trauma to patient incision sites. For pelvic surgery, at least three operating room configurations have been described: side docking, center docking (between the legs when the patient is in the dorsal lithotomy position), and parallel side docking (Figs. 15.4, 15.5, and 15.6) [4, 5]. If side docking is utilized, the location of monitors, surgical equipment, and the anesthesia staff should be organized to accommodate the patient side cart, which occupies one side of the bed. One possible operating room layout described below easily allows for side docking from the right side of the patient. In this scenario, it is recommended that the bedside surgeon and the accessory port are positioned on the patient’s left side. One advantage of side docking versus center docking is that it maximizes assistant access to the perineum/vagina. This allows for greater facility of uterine manipulation and facilitates vaginal delivery of the uterine specimen.
If center docking is preferred, the location of the equipment is flexible and may be organized so that the scrub nurse stands on the same side as the bedside assistant. An advantage of this set- up is that it allows placement of the fourth robotic arm on either side of the patient. In addition, this approach allows robotic trocars to be placed higher in the abdomen without instrument conflict, as may be required in cases with patients with large uteri, for para-aortic lymph node dissection, or for omentectomy in a gynecologic oncology procedure. To obtain better access to the upper abdomen, especially for oncologic procedures, the robot may also be docked from above the head of the patient. This set-up does not allow access to the pelvis and is frequently performed in conjunction with a docking position allowing pelvic access. This approach requires repositioning of both the patient bed and the bedside cart.




Fig. 15.4
Center docking position of the surgical robot

Fig. 15.5
Side docking position of the surgical robot

Fig. 15.6
Parallel docking position of the surgical robot
A variety of EndoWrist instruments (Intuitive Surgical, Inc.; Sunnyvale, CA) are available for robotic gynecologic surgery (Figs. 15.7 and 15.8). The surgeon should limit instrument exchange to improve efficiency and minimize cost. In most cases, the permanent cautery spatula or monopolar curved scissors is utilized in the medial right robotic arm, and fenestrated bipolar forceps or plasma kinetic (PK) dissecting forceps are placed in the left robotic arm. A grasper (ProGrasp forceps; Intuitive Surgical; Sunnyvale, CA, USA) instrument is inserted into the right lateral robotic arm whenever a fourth arm is used. When suturing is required, the medial robotic right instrument is switched for a Mega Suture Cut needle driver (Intuitive Surgical). The left robotic arm is switched to a Mega needle driver (Intuitive Surgical).



Fig. 15.7
Monopolar curved scissors

Fig. 15.8
Maryland bipolar forceps
15.3 Patient Selection
The selection of patients for robotic surgery is similar to the selection of patients for laparoscopic surgery. Most contraindications to robotic surgery are relative and depend on the skill set and experience of the surgeon (Table 15.2) [4]. Patients with decreased pulmonary reserve or poor cardiac function are at increased risk for complications. Patients with decreased pulmonary reserve may not tolerate prolonged ventilation or steep Trendelenburg positions that are required for pelvic robotic surgery. Patients with poor cardiac function may not tolerate prolonged pneumoperitoneum, as this may result in hypotension that may further compromise cardiac function.
The steep Trendelenburg position (30–40°) used during robotic gynecologic surgery plays a role in the tolerance of the procedure. A variety of medical comorbidities may limit patient tolerance of this position, and its judicious use is warranted. Patients are placed in a maximal Trendelenburg position to avoid undocking the robotic arms once the procedure has begun. In some cases, the degree of Trendelenburg positioning required to perform a complex gynecologic robotic-assisted procedure is more than the maximum amount possible on many beds. Surgeons should assess the positioning required at the beginning of the surgery rather than reflexively placing a patient in the maximum amount of Trendelenburg position tolerated. This may allow more patients to tolerate an extended period in this position. Insufflation pressures may also be decreased from the standard 15 mmHg to 10–12 mmHg after initial abdominal entry, as this may also allow more patients to tolerate robotic surgery.
Table 15.2




Relative contraindications to robotic surgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








