The evidence for decision-making in MDT meetings covers many different aspects of the MDT meeting across a range of specialities [8]. Several studies have found that MDTs make a difference to the outcome of care management decisions, compared with the decisions of individual clinicians. However, decisions in MDT meetings cannot always be reached, often due to the lack of clinical information. Furthermore, MDT decisions are not always implemented, because information relating to the patients’ clinical state or their comorbid conditions is sometimes insufficient. In particular, patient’s preferences are not taken into account when such decisions are made. Studies suggest that high-quality, feasible decisions also require support from good leadership, protected time for team-members to prepare prior to the meeting and adequate organizational facilities. The roles played by different team members within the MDT are varied, with typically lower importance placed on the input of nurses, who have skills in understanding patient’s psychosocial issues and choices for treatment.
This array of factors that can potentially impede the quality of decision-making is complex and difficult to understand as a whole. In order to better understand and assess decision-making in MDT meetings we took the systems approach as described above and applied it to the evidence for decision-making in MDT meetings [8]. By applying this approach we were able to develop a model of the factors that affect decision-making (Fig. 1.2). This model has provided a useful framework that we have used to systematically study the quality of teamwork and decision-making in MDT meetings.
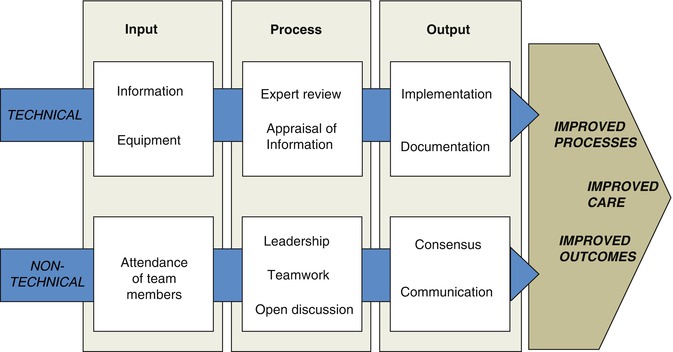
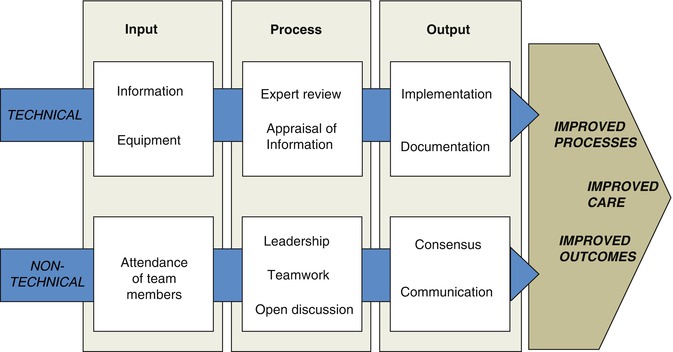
Fig. 1.2
A systems approach to decision-making in MDT meetings. ‘Technical’ refers to organizational factors and clinical skills. ‘Non-technical’ refers to team skills (Adapted from Lamb et al. [8])
1.3 Assessing Decision-Making in MDT Meetings
With a better understanding of MDT decision-making and the aspects that are important to high quality performance, we set out to construct a tool for the scientific assessment of MDT decision-making. In order to improve something, you first must be able to measure it. Using the principles of the observational assessment of team working from other areas of healthcare and other industries, along with evidence from the literature and our own research, we developed an observational tool, MDT-MODe to assess behaviors and information presentation in MDT meetings (Fig. 1.3). MDT-MODe was tested for inter-rater reliability, assessors’ learning curves, and cross-validated against MDT members’ own self-assessment. Presentation of a patient’s case history, radiological, and pathological information, information on psychosocial aspects and the patient’s comorbidities and their own views were assessed, as well as ratings of the MDT Chair’s effectiveness, and contribution to decision-making of the different MDT members, including urologists, oncologists, radiologists, pathologists, Clinical Nurse Specialists and MDT Coordinators. Whether a treatment decision was reached for each case, meeting characteristics including the number and profession of team members in attendance, number of cases discussed per meeting and start and end times of the meeting were also recorded.
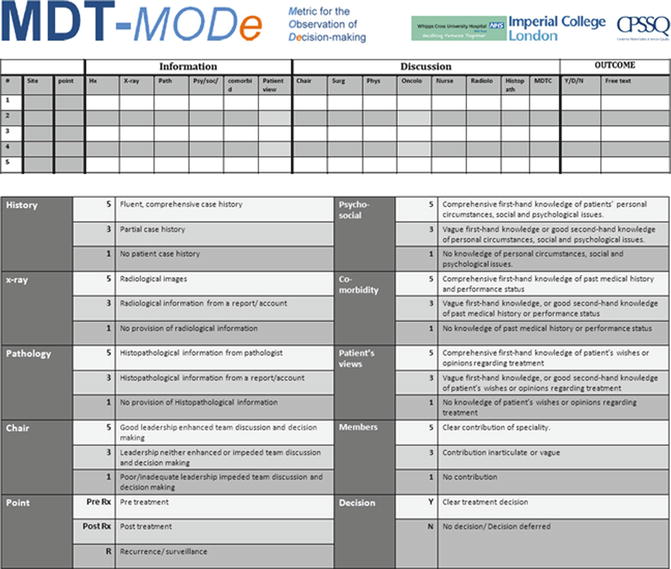
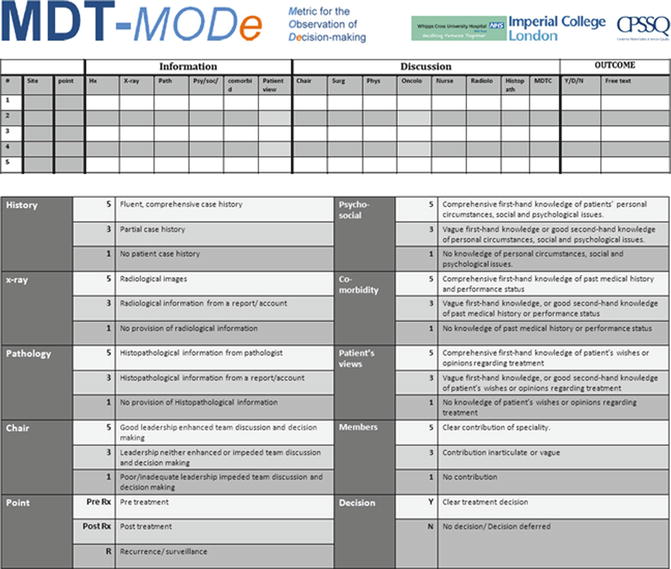
Fig. 1.3
Figure displaying MDT-MODe used to score behaviors during MDT meetings—including information provision and team-member contribution. Observed behaviors are compared to and scored against examples of behaviors of varying quality (Copyright 2013 Imperial College London. Accessed from http://www1.imperial.ac.uk/medicine/about/institutes/patientsafetyservicequality/cpssq_publications/resources_tools/mdt/)
This assessment tool was piloted with eight MDTs over 500 cases. Good reliability and learning curves were obtained in the assessment of MDT performance (median reliability coefficient = 0.71) [9]. Positive correlations were found between observational and self- assessments of MDTs (Spearman’s Rho = 0.66–0.91; Ps < 0.05)—thus showing validity [10]. The lack of standardization in MDT meetings was apparent during the study leading to variability in the information presented, case discussion between the team members and team decision-making. The observers found that information was presented in a haphazard manner and discussions did not always include all team members. The overall pattern of results suggested that bio-medical information is more comprehensively presented than patient-centered information, and urologists dominated the case discussion and inadvertently, other MDT members often had little overt involvement in team decision-making (Fig. 1.4). Treatment decisions were reached in 85 % of cases. Cases towards the end of meetings were associated with lower rates of decision-making, information quality and team working (r = −0.15 to −0.37). Increased numbers of cases per meeting and team-members in attendance were associated with better information and team working (r = 0.29–0.43). More time per case was associated with improved team working (r = 0.16). A positive correlation was found between the ability to reach decisions and improved information and team working (r = 0.36–0.54) (all P ≤ 0.001) [11].
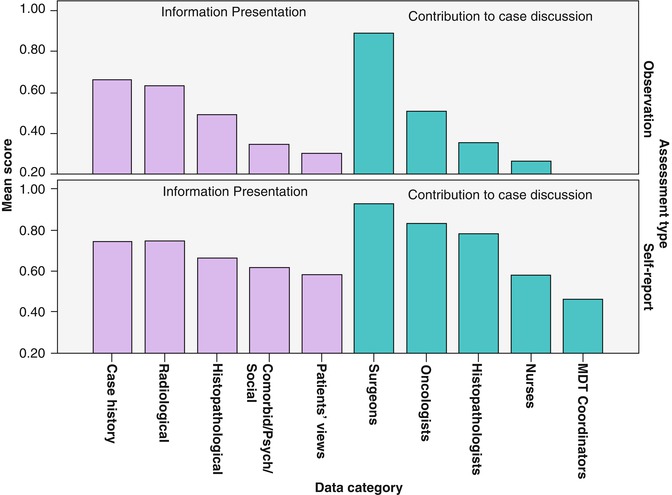
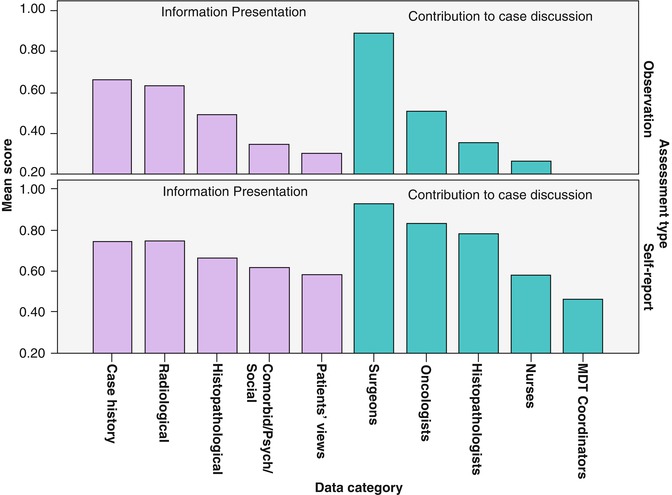
Fig. 1.4
Bar graphs displaying mean scores for information presentation and contribution to case discussion in MDT meetings for observational and self-report data (From Lamb et al. [10])
1.4 MDT Meeting Checklist
Equipped with tools to objectively and reliably measure the quality of decision-making in urology MDT meetings, we conducted a prospective longitudinal study over a 16-month period which evaluated decision-making for 1421 urological cancer patients treated at large cancer center in London [12]. Interventions to improve the MDT processes were introduced in stages including the development of a checklist, MDT-QuIC (Fig. 1.5), MDT team training, and simple written guidance to team-members. We found significant improvement over the course of the study: the MDT’s ability to reach a decision rose 13 %, quality of information presentation at the MDT meeting showed a 29 % increase, and quality of team working within the MDT improved by 14 %. The MDT’s ability to reach a treatment decision was related to the quality of available information and the quality of the team working within the MDT. Across the study period, the top three barriers to the teams’ ability to decide on a treatment plan were inappropriate patient referrals, inadequate radiological information and inadequate pathological information. This study suggested that both the decision-making ability and also the levels of team working and information quality within the MDT meeting is variable and could be improved using a combination of simple, evidence-based interventions.
Fig. 1.5




Figure displaying MDT-QuIC, a checklist designed to improve MDT decision-making (Copyright 2013 Imperial College London. Accessed from http://www1.imperial.ac.uk/medicine/about/institutes/patientsafetyservicequality/cpssq_publications/resources_tools/mdt/)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








