Hypertension after Transplantation
Fernando G. Cosio
Stephen C. Textor
Divisions of Nephrology and Hypertension, Department of Medicine and Transplant Center, Mayo Clinic Foundation and Mayo Clinic Medical School, Rochester, Minnesota, 55905
INTRODUCTION/PREVALENCE
Arterial hypertension is a major feature complicating the clinical course of patients with advanced kidney disease before and after transplantation. It is increasingly relevant to clinicians participating in the care of transplant patients to understand the role of hypertension in determining cardiovascular risk and the long-term success of the allograft. Thus, as outcomes of kidney allografts continue to improve, premature death of the patient with a functioning graft has become a major cause of transplantation failure. Furthermore, there is increasing evidence that nonimmunologic factors, such as hypertension, are major determinants of long-term kidney graft survival.
Hypertension is particularly common after kidney transplantation in patients treated with calcineurin inhibitors (CNIs). In the precyclosporine era of transplantation, prior to 1985, the reported incidence of hypertension was estimated between 40% and 60% (1,2). The incidence of hypertension increased with the introduction of the CNIs cyclosporine and then tacrolimus. For example, initial reports on the use of cyclosporine reported that approximately 70% of patients were significantly hypertensive (3). Since then, the reported incidence of hypertension has varied between 60% and 90%. It is likely that much of this variability reflects the different diagnostic criteria for hypertension used in different studies. Figure 19.1 displays the prevalence and severity of hypertension in kidney transplant recipients. As can be seen both at 6 months and at 2 years posttransplant more than 90% of recipients are hypertensive and this finding was independent of the origin of the allograft (living donor [LD] or deceased donor [DD]) and of the race of the recipient (African American or white). It should also be noted that the adequacy of blood pressure control improves with time posttransplant. Overall, the average number of blood pressure medications per patient was 3.2, at 6 months and that number was not significantly different among groups (see Fig. 19.1). Thus, posttransplant hypertension is common and difficult to control particularly during the early period.
This chapter will undertake to examine the relationship of hypertension to kidney transplant recipients from several points of view. First, we will consider the role of the kidney and immunosuppression in the regulation of arterial pressure after transplant. Second, we will consider the role of hypertension in determining the cardiovascular risks of the individual and the associations between hypertension, graft function and survival. Third, we will outline principles that
apply to the management of hypertension in kidney transplant recipients.
apply to the management of hypertension in kidney transplant recipients.
PATHOGENESIS/ASSOCIATIONS
Prior to kidney transplantation the majority of patients with chronic kidney disease are hypertensive (4). However, kidney transplantation is associated with an increase in both the prevalence and the severity of hypertension (3,5). From the practical point of view posttransplant hypertension can be considered in two stages: (a) hypertension that may develop during the immediate posttransplant period (arbitrarily defined as <3 months posttransplant); and (b) hypertension throughout the remaining follow-up period. This distinction is useful when considering the pathogenesis and the management of posttransplant hypertension.
Hypertension during the Immediate Posttransplant Period
During the first few days following transplantation arterial hypertension is common and often severe (Fig. 19.1). Few studies address changes in blood pressure during this time period. Based on the authors clinical experience, severe hypertension during this period is particularly common in three populations: (a) in patients with severe hypertension prior to transplantation; (b) in African Americans; and (c) in patients with delayed kidney graft function.
Table 19.1 lists variables that likely contribute to severe hypertension during the first few days and weeks posttransplant. Hypervolemia is present in many patients during the first few days posttransplant and likely contributes to hypertension. However, volume expansion rarely causes severe hypertension in patients with good allograft function. High doses of glucocorticoids likely contribute to the hypertension observed immediately posttransplant. Pharmacologic doses of glucocorticoids cause hypertension in humans at least in part by enhancing the pressor responses to a variety of mechanisms (see later) (6). Postoperative pain can contribute to hypertension. Consequently, adequate pain control merits careful attention from the responsible clinicians. Since most patients take antihypertensive medications before surgery, changes in medication in the perioperative period may lead to labile arterial pressures. It is also possible that certain characteristics of the donor graft can cause hypertension. Kidneys from marginal donors, such as those with preexisting hypertension and/or dying from intracranial hemorrhage are recognized to have relatively impaired early function and may aggravate hypertension in the recipient (7). Supporting this concept is the observation that transplantation of kidneys from donors with hepatorenal syndrome can be associated with severe hypertension (8). This clinical circumstance is rare but exemplifies how the status of the donor graft may contribute to hypertension.
Hypertension during Long-term Posttransplant Follow-up
Table 19.1 displays a series of variables that have been associated with sustained hypertension after kidney transplantation.
Although many of those variables are shared with blood pressure determinants in the general population, some are unique to the transplant situation.
Although many of those variables are shared with blood pressure determinants in the general population, some are unique to the transplant situation.
TABLE 19.1. Variables associated with the presence of hypertension following transplantation | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Donor variables: Experimental studies have long supported the concept that the kidney is an overriding determinant of blood pressure levels. Seminal studies by Dahl and collaborators (9) showed that transplanting the kidney from a normotensive, salt-resistant rat into a hypertensive rat that was previously nephrectomized results in normalization of blood pressure. Such studies indicate that blood pressure levels can “follow the kidney”. This concept has been difficult to study in humans where multiple factors contribute to blood pressure posttransplant. However, several studies confirm that under some circumstances the transplant kidney can normalize blood pressure in the recipient. Furthermore, Curtis and collaborators (10) showed that achievement of normotension after transplantation can result in reversal of hypertensive end organ damage (e.g., retinal changes and left ventricular hypertrophy).
Table 19.1 lists donor variables that have been associated with blood pressure levels following transplantation. Considering that kidney graft function is a powerful determinant of blood pressure (1,4,11,12) (see later) it is difficult to determine whether these donor variables are independent determinants of blood pressure or simply are related to graft function. For example; increasing donor age (13,14) and a history of hypertension in the donor (15) relate to both reduced kidney allograft function and higher levels of blood pressure. Studies comparing kidney function and blood pressure levels between pairs of recipients who received kidney grafts from one donor (12) indicate that serum creatinine and blood pressure in these individuals correlate with each other. Additional studies indicate that kidneys from African American donors are associated with hypertension in the recipient. In summary, donor variables and/or graft function relate to blood pressure levels in the recipient. A well functioning kidney allograft frequently improves or even normalizes blood pressure levels in the recipient (10,16).
Recipient Variables
The general demographic characteristics of kidney transplant recipients related to hypertension are similar to those in the general population and in individuals with kidney disease (4). Thus, as noted in Table 19.1, hypertension is more common among kidney transplant recipients of African American race; recipients with higher weight/body mass index; and in male recipients (1,11,12,17,18). It also should be noted that recipients who have diabetes prior to the transplant are also more likely to be hypertensive (18). Furthermore, these recipients are likely to have particularly elevated systolic blood pressure and widened pulse pressure (calculated as systolic blood pressure-diastolic blood pressure) compared to nondiabetic recipients (18). Other studies have shown an association between this blood pressure characteristic and increased cardiovascular risk (19).
Not surprisingly, posttransplant hypertension correlates with the presence of pretransplant hypertension (5,20,21). However, it should also be noted that after transplantation the prevalence and severity of hypertension increases. For example, in a group of 116 African American recipients, 78% were hypertensive before transplantation compared to 95% after transplantation. Posttransplant patients also required more anti-blood pressure medications (5). Recent studies, using more strict criteria for the diagnosis of hypertension (systolic blood pressure >140 mm Hg and/or diastolic blood pressure >90 mm Hg) reported that more than 85% of patients with chronic kidney disease are hypertensive prior to transplantation (4,22). It should be reemphasized that a transplanted kidney with good function may normalize blood pressure levels even in individuals with severe hypertension prior to the transplant (10). Thus, the presence of severe hypertension pretransplant should raise the physician’s level of vigilance about posttransplant blood pressure monitoring and treatment. In a latter section of this chapter we will consider the possible contribution of native kidney disease to posttransplant hypertension.
Hypertension and Graft Dysfunction
In patients with native kidney disease the glomerular filtration rate (GFR) is the strongest correlate of blood pressure levels (4). Similarly, several studies report correlations between graft function and hypertension following transplantation (1,11,12). It should be noted that hypertension is both
a sign of kidney disease and a cause of kidney dysfunction. Thus, from the practical point of view, worsening hypertension posttransplant should raise the possibility of acute or chronic graft pathology that may be otherwise clinically silent. For example, acute rejection is associated with significant elevations in blood pressure levels (23,24). In patients with chronic native kidney disease blood pressure rises as GFR declines and hypertension is particularly severe in those with glomerular diseases (4). Similar studies have not been done in transplant recipients although it is our clinical impression that hypertension is particularly severe in patients with chronic transplant glomerulopathy and in those patients who develop focal segmental glomerulosclerosis late after transplantation (25). In patients with declining kidney function and de novo or worsening hypertension, the possibility of transplant renal artery stenosis should be considered. This disorder will be considered later on in this chapter.
a sign of kidney disease and a cause of kidney dysfunction. Thus, from the practical point of view, worsening hypertension posttransplant should raise the possibility of acute or chronic graft pathology that may be otherwise clinically silent. For example, acute rejection is associated with significant elevations in blood pressure levels (23,24). In patients with chronic native kidney disease blood pressure rises as GFR declines and hypertension is particularly severe in those with glomerular diseases (4). Similar studies have not been done in transplant recipients although it is our clinical impression that hypertension is particularly severe in patients with chronic transplant glomerulopathy and in those patients who develop focal segmental glomerulosclerosis late after transplantation (25). In patients with declining kidney function and de novo or worsening hypertension, the possibility of transplant renal artery stenosis should be considered. This disorder will be considered later on in this chapter.
The Role of Corticosteroids
Corticosteroids are known to be associated with hypertension (1,2,6). However, the magnitude of this effect on posttransplant hypertension is not well understood. Several studies indicate that reductions or discontinuation of corticosteroids is associated with significant reductions in blood pressure (26, 27, 28, 29). Of interest, this effect is noted even in patients taking doses of prednisone as low as 10 mg per day. More recent studies report that withdrawal of corticosteroids after transplantation results in blood pressure lowering (30, 31, 32). However, the magnitude of this effect is variable and particularly significant in those patients receiving low doses of cyclosporine (30). Thus, there is convincing evidence that corticosteroids, even at low maintenance doses, contribute to hypertension after kidney transplantation. Some authors suggest that up to 15% of posttransplant hypertension is explained by glucocorticoid effect and that this complication adds substantially to the cost of managing transplant recipients (33).
The mechanism by which corticosteroids cause hypertension has been clarified, at least in part (reviewed in [6]). There is clear evidence from human studies that glucocorticoids by themselves, in the absence of a mineralocorticoid effect, can cause hypertension. However, at the doses used after transplantation, some activation of mineralocorticoid receptors is observed leading to potassium wasting, particularly during high sodium intake. The mechanism of glucocorticoid-induced hypertension appears to be independent of volume retention and of sodium intake, although high sodium diets enhance the hypertensive effect of this hormone. Glucocorticoids do not alter sympathetic tone. However, these drugs have significant hemodynamic effects including increased cardiac output that appear to be a dose dependent (34). Finally, the use of glucocorticoids in normal humans enhances the pressure responses to epinephrine, somewhat to angiotensin II, and to other pressure stimuli (6).
The Role of Calcineurin Inhibitors
The introduction of cyclosporine into clinical transplantation led to significant increases in the incidence and severity of hypertension (2,3). Hypertension develops rapidly after the introduction of these drugs and, contrary to initial reports (3), elevated blood pressures persist throughout the posttransplant period. Similarly, in nontransplant patients, the use of cyclosporine produces significant elevations in blood pressure (35). The evidence that CNIs cause hypertension in kidney transplant recipients is based on clinical observations. Thus, reducing the dose of cyclosporine (36,37), switching from cyclosporine to a non-CNI immunosuppressive medication (38,39), or discontinuing cyclosporine (40) are associated with either lowering of blood pressure levels and/or reductions in the number of antihypertensive drugs required to achieve blood pressure control. In contrast, it should be emphasized that reductions or withdrawal of CNIs in patients with advanced allograft dysfunction have only minor effects on blood pressure levels (37).
There is evidence that tacrolimus (Prograf, FK-506) causes less severe hypertension than cyclosporine. These observations are most evident in patients receiving tacrolimus for liver, cardiac or other nonrenal solid organ transplants. Several clinical trials in kidney transplant recipients compared, in a randomized fashion, the immunosuppressive effects of cyclosporine and tacrolimus. Those trials focus on the immunologic consequences of these drugs and changes in blood pressure levels are either not reported or appear only in a cursory fashion. In several of these studies there is little differences in blood pressure levels between patients assigned to cyclosporine or tacrolimus (17,41,42). In contrast, one clinical trial reported lower blood pressure levels in kidney transplant recipients receiving tacrolimus than in those receiving cyclosporine (43,44). This latter study is consistent with observations in liver transplant recipients where tacrolimus causes less hypertension than cyclosporine (45,46). Furthermore, transition from cyclosporine to tacrolimus is associated with a significant drop in blood pressure in kidney (42,47, 48, 49, 50), liver (51,52), and heart (53) allograft recipients.
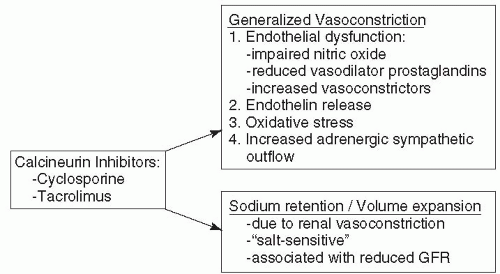
The mechanism underlying CNI-induced hypertension is widespread, intense vasoconstriction, particularly within the kidney. CNIs disturb multiple vasoactive mechanisms (Fig. 19.2), including impairment of the production of vasodilator substances (e.g. prostacyclin [54, 55, 56] and endotheliumderived nitric oxide [56,57]) and enhancement of the production of potent vasoconstrictors, such as endothelin (58, 59, 60, 61). Both circulating and urinary excretion of the latter is elevated in cyclosporine-treated transplant recipients (62). The role of the renin-angiotensin system in hypertensive effects of cyclosporine is less clear (63,64). Experimental studies indicate elevated activity in rats, but studies in renal, cardiac and liver transplant recipients indicate suppression of circulating levels of plasma renin activity soon after transplantation in humans. After the first year posttransplant,
impaired renal function may be associated with “inappropriately” elevated levels of renin activity (63,64). Experimental studies indicate that CNIs augment sympathetic nervous activity, as reflected by increased nerve traffic measured by microneurographic techniques (65,66). Data in humans are less consistent, however, some studies indicate that increased nerve traffic is more related to the presence of diseased native kidneys than to the use of CNIs (67).
impaired renal function may be associated with “inappropriately” elevated levels of renin activity (63,64). Experimental studies indicate that CNIs augment sympathetic nervous activity, as reflected by increased nerve traffic measured by microneurographic techniques (65,66). Data in humans are less consistent, however, some studies indicate that increased nerve traffic is more related to the presence of diseased native kidneys than to the use of CNIs (67).
Within the kidney, administration of CNI is followed promptly by intense afferent arteriole vasoconstriction that reduces renal blood flow and glomerular filtration rate (68,69). These effects reverse rapidly as the drug is removed from the blood stream. By this mechanism, CNIs cause alterations in sodium excretion resulting in volume expansion that contributes to hypertension. Continuous exposure to CNIs eventually causes chronic nephrotoxicity manifest by hyalinosis of the afferent arterioles and the appearance of interstitial fibrosis due, at least in part, to vascular occlusion (70,71). Despite these chronic vascular changes, discontinuation of CNIs in these patients still results in improvements in graft function, presumably due to improving blood flow, and some improvement in hypertension (72).
CNI-induced allograft endothelial injury deserves particular attention. This type of injury can produce a syndrome of accelerated hypertension associated with microangiopathic hemolytic anemia. Such a sequence has been observed with either cyclosporine or tacrolimus, which is often manifest as a “hemolytic uremic” syndrome (HUS) with a rapid rise in creatinine (73, 74, 75). This syndrome usually abates after therapy and temporary withdrawal of the CNI inhibitor. The mechanisms leading to these effects of CNI are unknown. However, patients with HUS in their native kidneys may be particularly predisposed to this toxicity (76).
The fact that CNIs affect so many different vascular pathways may explain the nearly universal findings of both posttransplant hypertension and hemodynamically mediated nephrotoxicity. These complex pathways (see Fig. 19.2) may also explain why no single antihypertensive agent is universally effective in reversing these effects of CNIs.
Hypertension and Other Immunosuppressive Medications
Neither azathioprine (Imuran) or mycophenolate mofetil (CellCept) are associated with hypertension. Similarly, there is no evidence that antilymphocyte antibodies have significant effects on blood pressure levels. Of interest, the initial clinical trials comparing sirolimus with cyclosporine in the prevention of acute rejection do not report differences in the incidence of hypertension between the treatment groups (77,78). This may be interpreted to indicate that the hypertensive effects of sirolimus are similar to those to cyclosporine. However, it should be noted that blood pressure levels and the number of antihypertensive medications used by patients in the two treatment groups do not appear in these reports. Thus, it is possible that patients taking cyclosporine were in fact more severely hypertensive than patients treated with sirolimus. This later hypothesis is supported by additional studies testing the substitution of cyclosporine for sirolimus and reporting that this maneuver was associated with significant reductions in blood pressure levels (79).
CONSEQUENCES OF HYPERTENSION IN KIDNEY TRANSPLANT RECIPIENTS
Hypertension after renal transplantation poses major concerns both regarding cardiovascular disease in the recipient and the long-term outcome of the allograft. Until now, no prospective studies have been performed to establish whether blood pressure control after transplantation reduces these risks. However, data from the general population and from patients with native kidney diseases leaves no doubt that hypertension control offers major benefits to allograft recipients. In this section, we will also consider the possible associations between hypertension and acute rejection.
Hypertension and Patient Survival
Studies in the General Population and in Patients with Native Kidney Diseases
In the general population, hypertension is a major cardiovascular risk factor (80, 81, 82). Furthermore, numerous prospective, randomized, controlled trials establish that lowering blood pressure reduces the risk of stroke, myocardial infarction, congestive heart failure and overall cardiovascular mortality (81, 82, 83, 84). Compared to the general population, patients with chronic kidney disease have a high prevalence of hypertension (4) and cardiovascular disease (85,86). Furthermore, survival analyses indicate that kidney disease
independently magnifies the mortality risk attributable to these disorders (82,87,88). The effects of blood pressure control on the cardiovascular risk of patients with kidney disease have not been studied prospectively. However, there is little reason to believe that blood pressure control would not be at least as effective in preventing cardiovascular disease in these patients as in the general population. The available evidence, although limited, supports this postulate. Thus, in patients with diabetes (with or without kidney disease) lower blood pressure levels reduce the risk of macrovascular disease (84,89). In addition, prospective studies show that maintenance of lower blood pressure levels is associated with lower risk of hospitalizations for cardiovascular-related problems in patients with chronic kidney disease (90).
independently magnifies the mortality risk attributable to these disorders (82,87,88). The effects of blood pressure control on the cardiovascular risk of patients with kidney disease have not been studied prospectively. However, there is little reason to believe that blood pressure control would not be at least as effective in preventing cardiovascular disease in these patients as in the general population. The available evidence, although limited, supports this postulate. Thus, in patients with diabetes (with or without kidney disease) lower blood pressure levels reduce the risk of macrovascular disease (84,89). In addition, prospective studies show that maintenance of lower blood pressure levels is associated with lower risk of hospitalizations for cardiovascular-related problems in patients with chronic kidney disease (90).
Hypertension and Transplant Patient Survival
The evidence that blood pressure control relates to the survival of kidney transplant recipients comes from retrospective studies. Several studies demonstrated an association between high blood pressure levels and either risk of cardiovascular disease and/or transplant patient survival (91, 92, 93). The relationship between systolic blood pressure levels 1 year following transplantation and patient survival after transplantation is shown graphically in Figure 19.3. As can be seen, increasing levels of systolic blood pressure are associated with progressive reductions in patient survival. Supporting the concept that hypertension control improves cardiovascular risk, well controlled hypertension leads to regression of left ventricular hypertrophy and reduces the risk of congestive heart failure in kidney transplant recipients (94,95). Additionally, lower levels of blood pressure correlate with slower progression of atherosclerotic carotid artery disease (96). Taken together, these data supports the hypothesis that hypertension is a strong determinant of cardiovascular risk and survival in kidney transplant recipients. Assuming that control of hypertension would be at least as effective in reducing the cardiovascular risk of patients with kidney disease as in the general population. We propose that improving blood pressure control offers an under-utilized opportunity to improve the survival of kidney transplant patients.
Hypertension, Kidney Disease and Its Progression
Hypertension and Native Kidney Disease
There is substantial evidence that hypertension causes native kidney disease and affects the progression of kidney dysfunction. In this section we will briefly review this evidence in patients with native chronic kidney disease and use this evidence to better understand the possible relationships between hypertension and kidney graft dysfunction.
The clinical evidence is convincing that malignant hypertension causes kidney disease. However, the evidence that milder forms of hypertension cause kidney damage is based mainly on epidemiologic studies showing that patients with hypertension have an increased risk of later developing renal disease (97, 98, 99). The epidemiologic evidence also shows that the risk of kidney disease is higher in hypertensive individuals of African American race and in those with low socioeconomic status (98). Based on this correlative evidence some authors propose that mild to moderate hypertension causes chronic kidney disease. However, there is some skepticism about this relationship, particularly in non-African American individuals. In part, this skepticism is based on the results of two prospective, randomized clinical trials testing directly the hypothesis that blood pressure control slows down the progression of kidney dysfunction. These trials were justified by several retrospective studies showing that the presence of hypertension and its severity correlate with the rate of progression of kidney dysfunction in both adults and children (88,89,100, 101, 102). The Modification of Diet in Renal Disease (MDRD) study tested prospectively whether diets low in protein and/or low blood pressure targets slow down the rate of progression of nondiabetic kidney disease. The results of that study clearly showed that, compared to a blood pressure of 140/90, a blood pressure of 125/75 significantly slows down the progression of kidney dysfunction. However, this effect was significant only in patients with proteinuria that is, in patients with glomerular disease (103, 104, 105, 106). A more recent study tested prospectively the effect of blood pressure control on the rate of progression of kidney disease in African Americans with hypertensive nephrosclerosis (107). Lower blood pressure levels did not change the rate of progression of renal dysfunction. Thus, there is little evidence that lowering blood pressure alters the progression of nonglomerular kidney diseases.
Considering that chronic allograft nephropathy is primarily a tubulointerstitial and vascular process, it is reasonable to question whether blood pressure control would affect the progression of this pathology.
Considering that chronic allograft nephropathy is primarily a tubulointerstitial and vascular process, it is reasonable to question whether blood pressure control would affect the progression of this pathology.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree