Fig. 18.1
Position of the operating team around the operating table
Fig. 18.2
Placement of trocars
The gastrohepatic ligament is divided, beginning the dissection above the caudate lobe of the liver where the ligament is thinner (Figs. 18.3 and 18.4). An accessory left hepatic artery originating from the left gastric artery is divided between clips (Figs. 18.5 and 18.6).

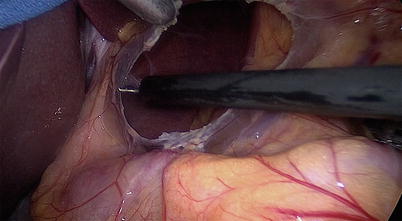

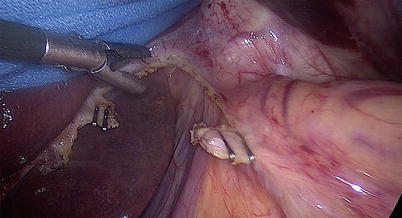

Fig. 18.3
The gastrohepatic ligament
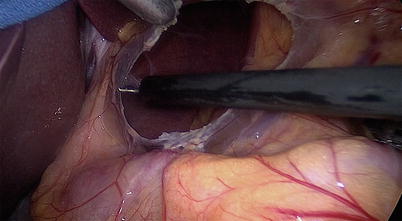
Fig. 18.4
The dissection of the gastrohepatic ligament, begun above the caudate lobe of the liver, where the ligament is thinner

Fig. 18.5
Clips placed on an accessory left hepatic artery originating from the left gastric artery so it can be divided
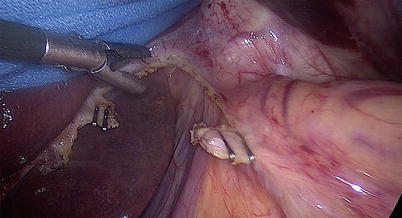
Fig. 18.6
The accessory left hepatic artery divided between clips
Dissection is continued proximally, and the right pillar of the crus is separated from the esophagus (Fig. 18.7). The phrenoesophageal membrane is divided using electrocautery (Fig. 18.8). Dissection is then performed in the posterior mediastinum (laterally, anteriorly and posteriorly) for about 5 cm above the diaphragm (Fig. 18.9). This step is important as it allows separation of esophagus from the aorta. Sometimes it can be difficult to find the plane between these two structures, either because of radiation changes or extramural spread of the tumor. In these cases, it is safer to proceed with this part of the dissection during the thoracotomy. Lower mediastinal lymph nodes are retrieved.
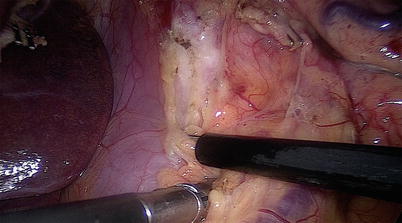
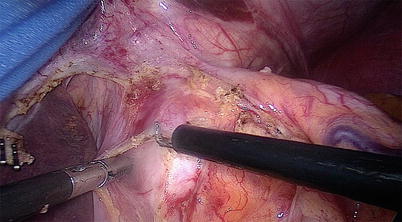
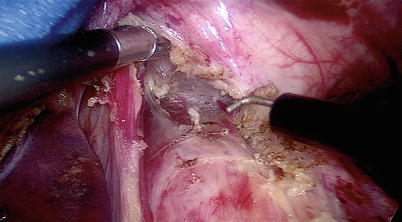
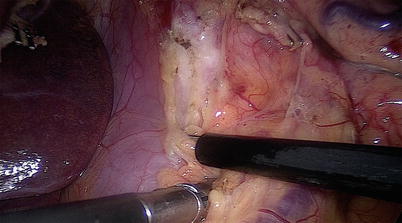
Fig. 18.7
Dissection continued proximally; the right pillar of the crus is separated from the esophagus
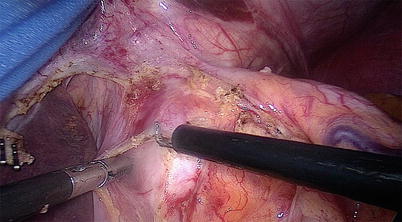
Fig. 18.8
The phrenoesophageal membrane is divided using electrocautery
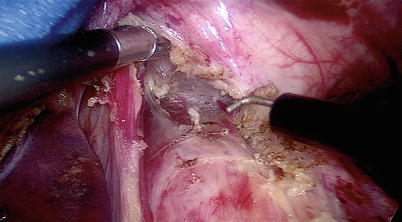
Fig. 18.9
Dissection performed in the posterior mediastinum (laterally, anteriorly, and posteriorly) for about 5 cm above the diaphragm
The right gastroepiploic artery is identified (Fig. 18.10) and the gastrosplenic ligament is opened using a bipolar instrument (Fig. 18.11). All the short gastric vessels are divided, and the dissection is continued all the way to the left pillar of the crus (Fig. 18.12). A window is created between the left pillar of the crus, the esophagus, and the stomach (Figs. 18.13 and 18.14). A Penrose drain is passed around the esophagus.
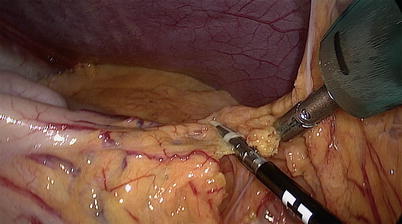
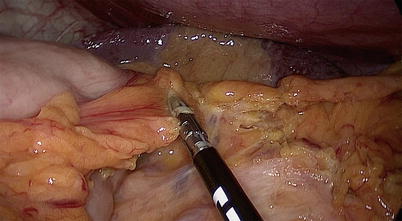
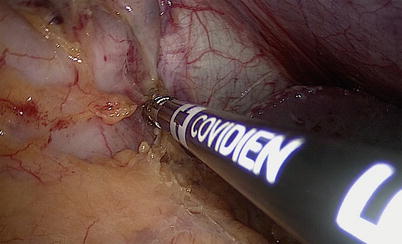
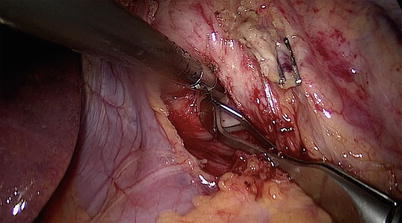
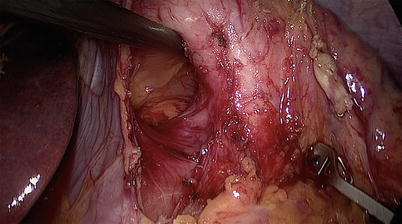
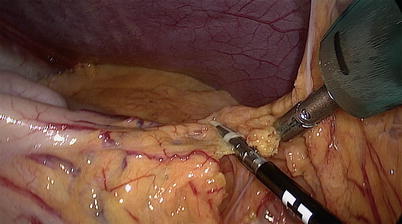
Fig. 18.10
Identification of the right gastroepiploic artery
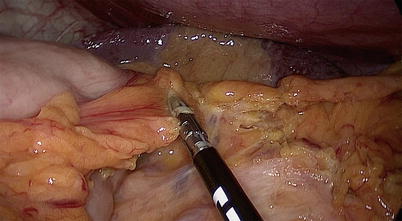
Fig. 18.11
Opening of the gastrosplenic ligament, using a bipolar instrument
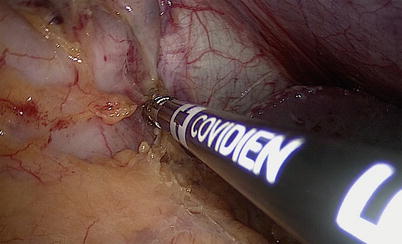
Fig. 18.12
Division of the short gastric vessels; dissection continued all the way to the left pillar of the crus
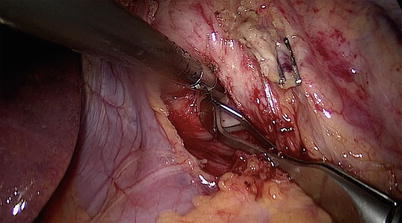
Fig. 18.13
Creation of a window between the left pillar of the crus, the esophagus, and the stomach
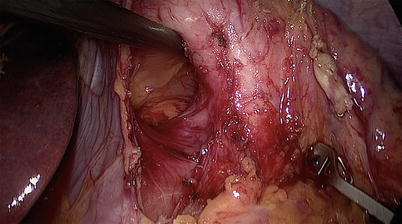
Fig. 18.14
Creation of a window between the left pillar of the crus, the esophagus, and the stomach
The coronary vein and the left gastric artery are divided. The vessels are dissected all the way to their base in order to retrieve as many left gastric nodes as possible (Figs. 18.15, 18.16, 18.17, and 18.18). An Endo GIA™ stapler (Covidien, Minneapolis, MN) with a 45-mm vascular cartridge is inserted through port 2 and is used for the transection of these vessels (Figs. 18.19, 18.20, and 18.21). Adhesions posterior to the esophagus and stomach are taken down using scissors or the hook cautery.
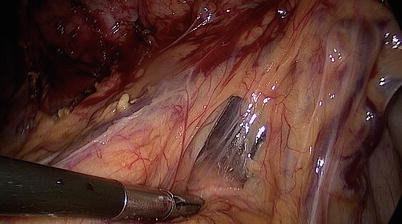
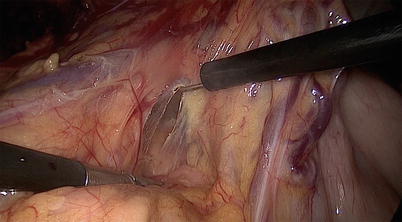
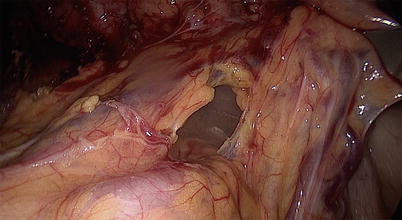
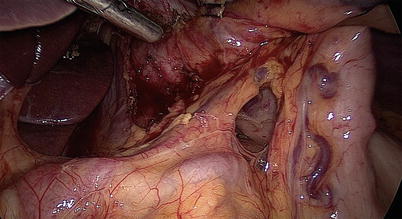
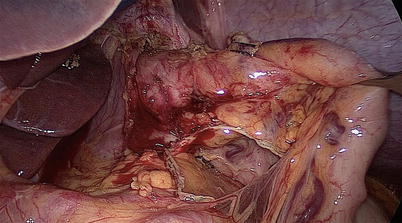
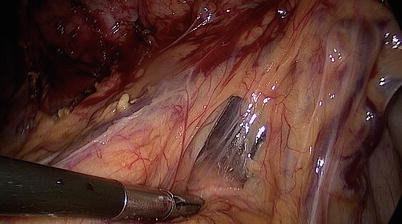
Fig. 18.15
Division of the coronary vein and the left gastric artery, which are dissected all the way to their base
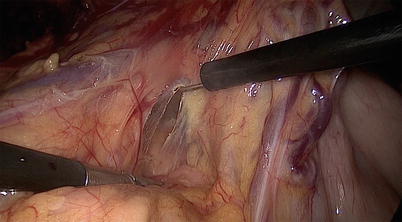
Fig. 18.16
Division of the coronary vein and the left gastric artery, which are dissected all the way to their base
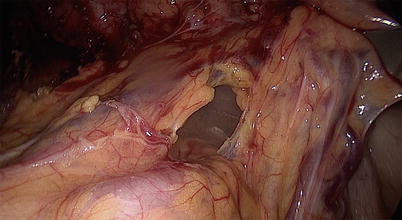
Fig. 18.17
Division of the coronary vein and the left gastric artery, which are dissected all the way to their base
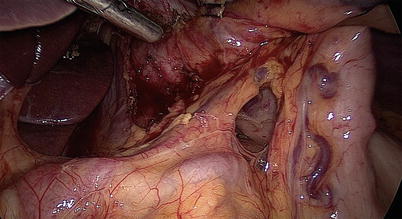
Fig. 18.18
Division of the coronary vein and the left gastric artery, which are dissected all the way to their base
Fig. 18.19
(a, b) An Endo GIA™ stapler (Covidien, Minneapolis, MN) with a 45-mm vascular cartridge is used for the transection of the coronary vein and left gastric artery
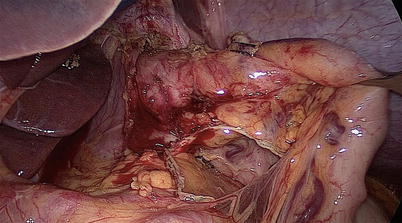
Fig. 18.20




The transected vessels after stapling
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








